Laboratory 1 Donor History
advertisement

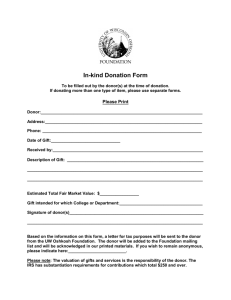
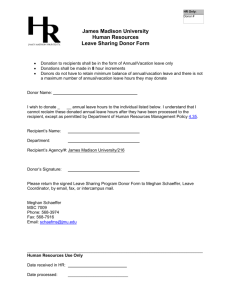
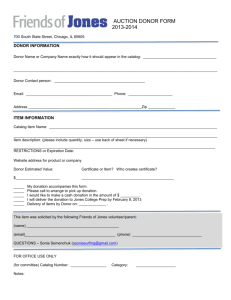
Laboratory 1 Donor History Laboratory 1 Donor History Skills: 10 points Objectives 1. Properly register the donor by obtaining all necessary information. 2. In a tactful, respectful manner, ask the donor all appropriate questions and correctly record the responses. 3. Evaluate the donor responses and determine the length of time for deferral for all unacceptable responses to the questions asked. 4. List 4 conditions which would permanently defer a donor. 5. List 4 conditions which would temporarily defer a donor. 6. List the deferral time periods for the immunizations listed in your lecture guide. 7. State the reason for deferral for sexually transmitted diseases. 8. Explain why donors who have spent 3 months or more in the United Kingdom are indefinitely deferred as blood donors. 9. List the two broad reasons for performance of the donor interview and physical exam. Discussion Careful donor selection plays a major role in determining whether or not a unit of donor blood will be therapeutically effective and free of transmissible disease. There are two parts in the selection of eligible blood donors. The first part involves obtaining a brief oral medical history. The interview must be conducted by qualified personnel in a manner that assures auditory privacy (visual privacy is also recommended), that allays apprehensions, and allows time for any necessary discussion or explanation. Answers to questions must be recorded as "yes" or "no" with details added as indicated. Results of tests must be recorded. Some very specific questions will be necessary but a great deal of pertinent information can be obtained by asking some general or leading questions in simple language that the donor can understand. If a potential donor passes the oral medical history interview they must then undergo a very limited physical exam. The details of the physical exam will be covered in the next laboratory exercise. Based on the answers to specific questions the interviewer must evaluate the responses and determine whether or not the potential donor is eligible to donate blood. The questions asked serve two purposes. The first is to ensure that the donation of blood or blood components will not compromise the health of the potential donor. The second is to make sure that a potential donor’s blood will not transmit a disease state to the potential recipient. Donors may donate one unit of whole blood every 8 weeks. Donation intervals for other types of products (double red cell unit, apheresis platelets, etc.) will vary. Whole blood or red blood cells 8 weeks Two unit red cell unit 16 weeks Platelet apheresis – up to 24 times/year Plasmapheresis– once every 4 weeks, can be done twice a week 1|Page Laboratory 1 Donor History The minimum of age of the donor is 16 according to the AABB. Some states may require parental consent or a higher age. There is no maximum age limit. The potential donor's past and present health status will aid in making this determination. The potential donor's past and present health status will aid in making this determination. There are certain situations in which a potential donor will be accepted (past carcinoma in situ of the cervix). Some conditions will require a certain time period of deferral (12 months if rabies vaccine has been administered). And still other conditions which will result in a permanent deferral of a donor (AIDS, hepatitis B, hepatitis C, etc.). It is of critical importance that the interviewer knows the type of deferral which must be recommended for a variety of conditions. There are some general guidelines to follow when making decisions about donor deferral. Twelve (12) month deferrals o Received blood or blood products, skin graft or tissue transplant (including corneas) o Hepatitis exposure or hepatitis B immune globulin shot o Heart attack or heart surgery o Pacemaker or implanted defibrillator o Transfusion of blood or blood products o Sexual partner of someone in a high risk group o Ear/body piercing and tattoos-NOT performed under sterile conditions o Accidental exposure to blood or body fluid o Rabies vaccine after animal bite o Had sexually transmitted disease o Travel to Iraq o Travel to a malaria area Permanent deferral o Has an infectious disease such as Hepatitis B Hepatitis C HIV Babesiosis or Chagas disease Crueutzfeldt-Jakob Disease (CJD) or family member with CJD o Had hepatitis or yellow jaundice AFTER the 11th birthday o Chagas’ disease and babesiosis o Has ever used intravenous drugs (illegal IV drugs) o Most cancers o Received a blood transfusion in the United Kingdom or France since 1980 o Cumulative time of 5 years or more in Europe (including time spent in the UK from 1/1/1980 to 12/31/1996) o Received a dura mater graft o Taken Tegison for psoriasis Temporary deferrals o Certain conditions such as pregnancy – six (6) weeks after delivery o Staying more than 72 hours in a correctional facility or jail o Certain medications (see list) o Refer to BLOOD DONOR EDUCATIONAL MATERIALS in this procedure. 2|Page Laboratory 1 Donor History Vaccines o Smallpox – eight weeks after vaccination o Two (2) weeks – measles (rubeola), mumps, oral polio, oral Typhoid, Yellow fever. o Four (4) weeks – German measles (rubella) and chicken pox (varicella zoster) o NO DEFERRAL if symptom-free – anthrax, cholera, diphtheria, influenza, Lyme disease, paratyphoid, polio injection, routine rabies. West Nile virus-no longer symptomatic-120 day wait What tests are performed on blood after it has been donated? After blood is drawn, it is tested for ABO group (blood type) and RH type (positive or negative), as well as for any unexpected red blood cell antibodies that may cause problems for the recipient. Screening tests performed are listed below: Hepatitis B surface antigen (HBsAg) Hepatitis B core antibody (anti-HBc) Hepatitis C virus antibody (anti-HCV) HIV-1 and HIV-2 antibody (anti-HIV-1 and anti-HIV-2) HTLV-I and HTLV-II antibody (anti-HTLV-I and anti-HTLV-II) Serologic test for syphilis Nucleic acid amplification testing (NAT) for HIV-1 ribonucleic acid (RNA), HCV RNA and WNV RNA Nucleic acid amplification testing (NAT) for HBV deoxyribonucleic acid Antibody test for Trypanosoma cruzi, the agent of Chagas' disease 3|Page Laboratory 1 Donor History Procedure Supplies Needed 1. 2. 3. Interview worksheet Pen Potential donor (classmate) Procedure 1. READ EACH OF THE FOLLOWING INSTRUCTIONS CAREFULLY BEFORE STARTING. 2. Determine which student will be the “Interviewer” and which will be the “donor”. 3. If you are the “Interviewer” you will: a. Allow the donor to review the “Blood Donor Education Materials”. b. Allow the donor to review the “Medication Deferral List”. c. Register the donor by recording their name and demographic information in the correct spot. d. Asks the donor about time of their last meal and weight. e. Use great tact and professionalism when asking the donor each question on the questionnaire. f. Accurately record the responses as they are given. g. Upon completion of the interview the “Interviewer” will evaluate each response. If an unacceptable response was given note which question number and the recommended deferral time. h. If you cannot find the deferral time write “Refer to SOP”. SOP stands for Standard Operating Procedure manual. 4. “Donor” will select three (3) items in such a manner as to be deferred as a donor. a. DO NOT ANSWER INAPPROPRIATE TO MORE THAN THREE. b. Use your REAL name, but make up other identifying information. 4|Page Laboratory 1 Donor History Blood Donor Educational Materials: MAKING YOUR BLOOD DONATION SAFE Thank you for coming in today! This information sheet explains how YOU can help us make the donation process safe for yourself and patients who might receive your blood. PLEASE READ THIS INFORMATION BEFORE YOU DONATE! If you have any questions now or anytime during the screening process, please ask blood center staff. ACCURACY AND HONESTY ARE ESSENTIAL! Your complete honesty in answering all questions is very important for the safety of patients who receive your blood. All information you provide is confidential. DONATION PROCESS: To determine if you are eligible to donate we will: Ask questions about health, travel, and medicines Ask questions to see if you might be at risk for hepatitis, HIV, or AIDs -Take your blood pressure, temperature and pulse -Take a small blood sample to make sure you are not anemic If you are able to donate we will: Cleanse your arm with an antiseptic. (If you are allergic to Iodine, please tell us!) Use a new, sterile, disposable needle to collect your blood DONOR ELIGIBILITY – SPECIFIC INFORMATION Why we ask questions about sexual contact: Sexual contact may cause contagious diseases like HIV to get into the bloodstream and be spread through transfusions to someone else. Definition of “sexual contact”: The words “have sexual contact with” and “sex” are used in some of the questions we will ask you, and apply to any of the activities below, whether or not a condom or other protection was used: 1. Vaginal sex (contact between penis and vagina) 2. Oral sex (mouth or tongue on someone’s vagina, penis, or anus) 3. Anal sex (contact between penis and anus) HIV/AIDS RISK BEHAVIORS AND SYMPTOMS AIDS is caused by HIV. HIV is spread mainly through sexual contact with an infected person OR by sharing needles or syringes used for injecting drugs. DO NOT DONATE IF YOU: Have AIDS or have ever had a positive HIV test Have ever used needles to take drugs, steroids, or anything not prescribed by your doctor Are a male who has had sexual contact with another male, even once, since 1977 Have ever taken money, drugs or other payment for sex since 1977 Have had sexual contact in the past 12 months with anyone described above Have had syphilis or gonorrhea in the past 12 months In the last 12 months have been in juvenile detention, lockup, jail or prison for more than 72 hours Have any of the following conditions that can be signs or symptoms of HIV/AIDS: o Unexplained weight loss or night sweats o Blue or purple spots in your mouth or skin o Swollen lymph nodes for more than one month o White spots or unusual sores in your mouth o Cough that won’t go away or shortness of breath o Diarrhea that won’t go away o Fever of more than 100.5°F for more than 10 days 5|Page Laboratory 1 Donor History Remember that you CAN give HIV to someone else through blood transfusions even if you feel well and have a negative HIV test. This is because tests cannot detect infections for a period of time after a person is exposed to HIV. If you think you may be at risk for HIV/AIDS or want an HIV/AIDS test, please ask for information about other testing facilities. PLEASE DO NOT DONATE TO GET AN HIV TEST! Travel to or birth in other countries Blood donor tests may not be available for some contagious diseases that are found only in certain countries. If you were born in, have lived in, or visited certain countries, you may not be eligible to donate. What happens after your donation? To protect patients, your blood is tested for hepatitis B and C, HIV, certain other viruses, and syphilis. If your blood tests positive it will not be given to a patient. You will be notified about test results that may disqualify you from donating in the future. Please do not donate to get tested for HIV, hepatitis, or any other infections! Thank you for donating blood today! Austin Community College 512-For-Blud 6|Page Laboratory 1 Donor History MEDICATION DEFERRAL LIST Please tell us if you are now taking or if you have EVER taken any of these medications: Proscar© (finasteride) usually given for prostate gland enlargement Avodart©, Jalyn (dutasteride) usually given for prostate enlargement Propecia© (finasteride) usually given for baldness Accutane© (Amnesteem, Claravis, Sotret, isotretinoin) usually given for severe acne Soriatane© (acitretin) or Tegison© (etretinate) – usually given for severe psoriasis Growth Hormone from human pituitary glands used usually for children with delayed or impaired growth Insulin from cows (Bovine or Beef Insulin) used to treat diabetes Hepatitis B Immune Globulin – given following an exposure to hepatitis B o NOTE: This is different from the hepatitis B vaccine which is a series of 3 injections given over a 6 month period to prevent future infection from exposures to hepatitis B. Plavix (clopidogrel) and Ticlid (ticlopidine) – inhibits platelet function; used to reduce the chance for heart attack and stroke. Feldene – given for mild to moderate arthritis pain Experimental Medication or Unlicensed (Experimental) Vaccine – usually associated with a research protocol Antibiotics Coumadin (Warfarin) or heparin – prevents clotting of the blood IF YOU WOULD LIKE TO KNOW WHY THESE MEDICINES AFFECT YOU AS A BLOOD DONOR, PLEASE KEEP READING: If you have taken or are taking Proscar, Avodart, Jalyn, Propecia, Accutane, Soriatane, or Tegison, these medications can cause birth defects. Your donated blood could contain high enough levels to damage the unborn baby if transfused to a pregnant woman. Once the medication has been cleared from your blood, you may donate again. Following the last dose, the deferral period is one month Proscar, Propecia and Accutane, six months for Avodart and Jalyn, and three years for Soriatane. Tegison is a permanent deferral. Growth hormone from human pituitary glands was prescribed for children with delayed or impaired growth. The hormone was obtained from human pituitary glands. Some people who took this hormone developed a rare nervous system condition called Creutzfeldt - Jakob disease (CJD, for short). The deferral is permanent. Insulin from cows (bovine, or beef, insulin) is an injected material used to treat diabetes. If this insulin was imported into the US from countries in which “Mad Cow Disease” has been found, it could contain material from infected cattle. There is concern that "Mad Cow Disease" is transmitted by transfusion. The deferral is indefinite. Hepatitis B Immune Globulin (HBIG) is an injected material used to prevent infection following an exposure to hepatitis B. HBIG does not prevent hepatitis B infection in every case, therefore persons who have received HBIG must wait 12 months to donate blood to be sure they were not infected since hepatitis B can be transmitted through transfusion to a patient. Feldene is a non-steroidal anti-inflammatory drug that can affect platelet function. A donor taking Feldene will not be able to donate platelets for 2 days; however, its use will not affect whole blood donations. Plavix and Ticlid are medications that can decrease the chance of a heart attack or stroke in individuals at risk for these conditions. Since these medications can affect platelets, anyone taking Plavix or Ticlid will not be able to donate platelets for 14 days after the last dose. Use of either medication will not prohibit whole blood donations. Experimental Medication or Unlicensed (Experimental) Vaccine is usually associated with a research protocol and the effect on blood donation is unknown. Deferral is one year unless otherwise indicated by Medical Director. 7|Page Laboratory 1 Donor History Interviewer Name (Your Name) ________________________________________________ Donor Name _______________________________________________________ Address _______________________________________________________ Date of Birth _______________________ Social Security Number _________________________ When did you eat last?_________________________ Do you weigh over 110 lbs (circle ONE) ? YES NO Yes No Are you Feeling healthy and well today? Currently taking an antibiotic? Currently taking any other medication for an infection? Please read the Medication Deferral List. Are you now taking or have you ever taken any medications on the Medication Deferral List? Have you read the educational materials? In the past 48 hours Have you taken aspirin or anything that has aspirin in it? In the past 6 weeks Female donors: Have you been pregnant or are you pregnant now? (Males: check “I am male.”) male In the past 8 weeks have you Donated blood, platelets or plasma? Had any vaccinations or other shots? Had contact with someone who had a smallpox vaccination? In the past 16 weeks Have you donated a double unit of red cells using an apheresis machine? In the past 12 months have you Had a blood transfusion? Had a transplant such as organ, tissue, or bone marrow? Had a graft such as bone or skin? Come into contact with someone else’s blood? Had an accidental needle-stick? 8|Page Laboratory 1 Donor History Yes No Had sexual contact with anyone who has HIV/AIDS or has had a positive test for the HIV/AIDS virus? Had sexual contact with a prostitute or anyone else who takes money or drugs or other payment for sex? Had sexual contact with anyone who has ever used needles to take drugs or steroids, or anything not prescribed by their doctor? Had sexual contact with anyone who has hemophilia or has used clotting factor concentrates? Female donors: Had sexual contact with a male who has ever had sexual contact with another male? (Males: check “I am male.”) Had sexual contact with a person who has hepatitis? Lived with a person who has hepatitis? Had a tattoo? Had ear or body piercing? Had or been treated for syphilis or gonorrhea? Been in juvenile detention, lockup, jail, or prison for more than 72 hours? In the past three years have you Been outside the United States or Canada? male From 1980 through 1996, Did you spend time that adds up to three (3) months or more in the United Kingdom? (Review list of countries in the UK) Were you a member of the U.S. military, a civilian military employee, or a dependent of a member of the U.S. military? From 1980 to the present, did you Spend time that adds up to five (5) years or more in Europe? (Review list of countries in Europe.) Receive a blood transfusion in the United Kingdom? (Review list of countries in the UK.) From 1977 to the present, have you Received money, drugs, or other payment for sex? Male donors: had sexual contact with another male, even once? (Females: check “I am female.”) female Have you EVER Had a positive test for the HIV/AIDS virus? Used needles to take drugs, steroids, or anything not prescribed by your doctor? Used clotting factor concentrates? Had hepatitis? Had malaria? Had Chagas’ disease? Had babesiosis? 9|Page Laboratory 1 Donor History Yes No Received a dura mater (or brain covering) graft? Had any type of cancer, including leukemia? Had any problems with your heart or lungs? Had a bleeding condition or a blood disease? Had sexual contact with anyone who was born in or lived in Africa? Been in Africa? Have any of your relatives had Creutzfeldt-Jakob disease? Evaluation of Results Based on the information obtained from your donor history interview, complete the chart below. Refer to your lecture guide and textbook for assistance in determining deferral status, if applicable. Question Number Reason for Deferral Length of Deferral Forms used in this laboratory were downloaded from the AABB web site: http://www.aabb.org/resources/donation/questionnaires/Pages/dhqaabb.aspx 10 | P a g e Laboratory 1 Donor History INFORMED CONSENT I, the undersigned, have reviewed and understand the donor eligibility information and the blood donation process. I agree NOT to donate blood or plasma for transfusion to another person or for further manufacture if I have AIDS, a positive HIV antibody test, or if any of the activities or signs and symptoms associated with AIDS apply to me. I understand that my blood will be tested for laboratory evidence of infectious agents capable of transmission through blood transfusion including, but not limited to, the AIDS virus, hepatitis B, and other viruses. I understand that I will be notified of test results that are important to my health and may affect my eligibility to be a blood donor. If my HIV, hepatitis, or other test results are confirmed positive my blood will not be transfused and my name will become part of a list of permanently deferred blood donors. I understand that test results and medical history information will not be released without my written consent, except as required by law. I have truthfully answered all medical questions. I am voluntarily donating my blood to be used as determined by Austin Community College, and I at my own risk, for good consideration, hereby release Austin Community College and its staff from all claims and demands incidental to or relative to the donation of this blood. Donor (Printed Name)______________________________________ Donor Signature Date _______________________________ _________________________________________ Interviewer (Printed Name) ________________________________ Interviewer Signature ______________________________________ Date _______________________________________ BASED ON THE INFORMATION PROVIDED BY THE DONOR SELECT ONE OF THE FOLLOWING (check ONE): _____ Donor MUST be deferred for _______________ _____ Donor is acceptable. 11 | P a g e Laboratory 1 Donor History Name_________________________________ Date___________________________ ___/14 points Laboratory 1 Donor History Study Questions Each correct answer is worth 0.5 unless otherwise indicated. 1. How often may a donor donate a single unit of whole blood? A potential donor has had the medical history interview. List the deferral time for each situation listed below. (Refer to your lecture guide and textbook). 2. Had surgery and received 2 units of blood. 3. Wishes to donate platelets but took aspirin last night for a headache. 4. Had leukemia but has been in remission for 10 years. 5. Recently had a baby. 6. Had hepatitis at age 8. 7. Has been implicated in 2 cases of post-transfusion hepatitis. 8. Recently had a tattoo. 9. Recently got out of prison. 10. Traveled to a malarial endemic country for a 2 week vacation. 11. Admits to having been a prostitute in 1983. 12. Received pituitary growth hormone of human origin in 1968. 13. Is taking Accutane for treatment of acne. 12 | P a g e Laboratory 1 Donor History List the deferral times for the following immunizations. 14. Measles (rubeola) 15. Immune serum globulin (HBIG) following blood exposure 16. Hepatitis B vaccine 17. German measles (rubella) 18. Mumps 19. Oral Polio 20. Yellow fever 21. Smallpox 22. Cholera 23. What are the minimum and maximum age requirements for qualifying as a routine blood donor? (1 point) a. Minimum – b. Maximum 24. The questions asked during the donor interview (medical history) serve 2 purposes, state these two purposes. (2 points). a. b. 13 | P a g e