chapter_24
advertisement
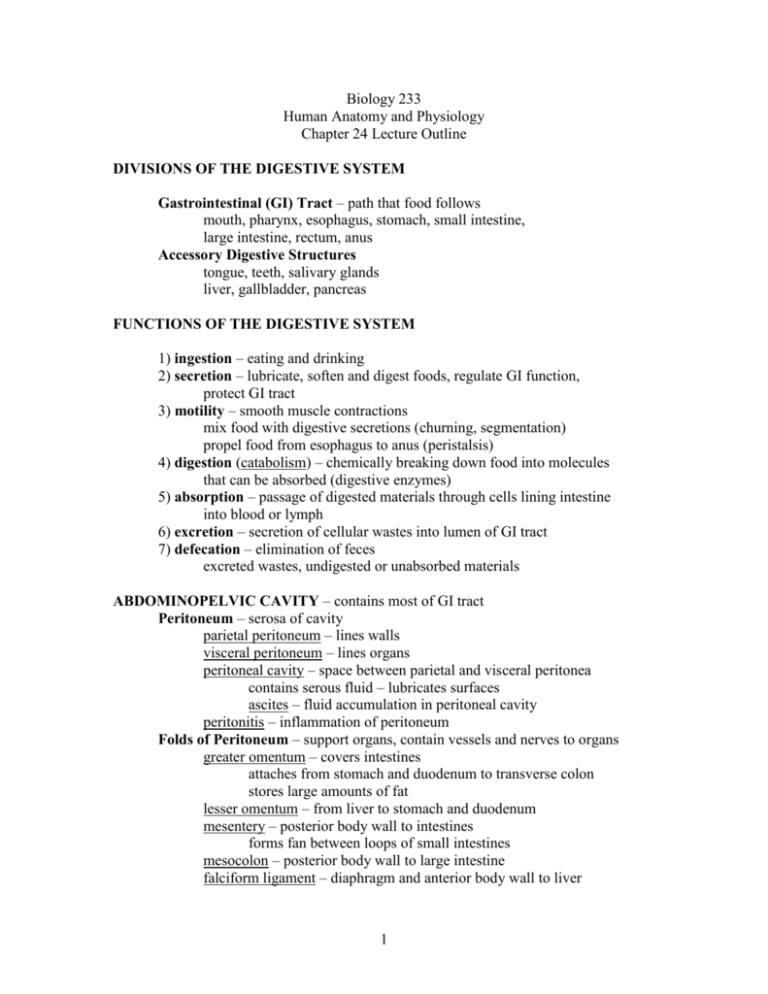
Biology 233 Human Anatomy and Physiology Chapter 24 Lecture Outline DIVISIONS OF THE DIGESTIVE SYSTEM Gastrointestinal (GI) Tract – path that food follows mouth, pharynx, esophagus, stomach, small intestine, large intestine, rectum, anus Accessory Digestive Structures tongue, teeth, salivary glands liver, gallbladder, pancreas FUNCTIONS OF THE DIGESTIVE SYSTEM 1) ingestion – eating and drinking 2) secretion – lubricate, soften and digest foods, regulate GI function, protect GI tract 3) motility – smooth muscle contractions mix food with digestive secretions (churning, segmentation) propel food from esophagus to anus (peristalsis) 4) digestion (catabolism) – chemically breaking down food into molecules that can be absorbed (digestive enzymes) 5) absorption – passage of digested materials through cells lining intestine into blood or lymph 6) excretion – secretion of cellular wastes into lumen of GI tract 7) defecation – elimination of feces excreted wastes, undigested or unabsorbed materials ABDOMINOPELVIC CAVITY – contains most of GI tract Peritoneum – serosa of cavity parietal peritoneum – lines walls visceral peritoneum – lines organs peritoneal cavity – space between parietal and visceral peritonea contains serous fluid – lubricates surfaces ascites – fluid accumulation in peritoneal cavity peritonitis – inflammation of peritoneum Folds of Peritoneum – support organs, contain vessels and nerves to organs greater omentum – covers intestines attaches from stomach and duodenum to transverse colon stores large amounts of fat lesser omentum – from liver to stomach and duodenum mesentery – posterior body wall to intestines forms fan between loops of small intestines mesocolon – posterior body wall to large intestine falciform ligament – diaphragm and anterior body wall to liver 1 Retroperitoneal Organs – behind parietal peritoneum, against posterior wall kidneys, adrenals, pancreas and duodenum GENERAL HISTOLOGY OF THE GI TRACT 4 Main Layers: mucosa – inner epithelial membrane submucosa – connective tissue muscularis – smooth muscle serosa (visceral peritoneum) or adventitia (connective tissue connected to surrounding tissues) 1) Mucosa – 3 layers epithelium (inner layer) – 2 types depending on region nonkeratinized stratified squamous – protects from abrasion mouth, pharynx, esophagus, anal canal simple columnar – secretion, absorption stomach, small and large intestines tight junctions between cells prevent leakage goblet cells – secrete mucus enteroendocrine cells – secrete regulatory hormones lamina propria (middle layer) areolar connective tissue w/ blood and lymph vessels mucous glands MALT (mucosa-associated lymphatic tissue) immune protection – lymphocytes and macrophages muscularis mucosae (outer layer) smooth muscle – tension produces folds in epithelium 2) Submucosa dense irregular connective tissue w/ blood and lymph vessels various digestive glands submucosal plexus – nerves that regulate mucosa and submucosa regulates mucosal movement, vascular diameter, secretions 3) Muscularis (externa) mainly smooth muscle inner circular layer outer longitudinal layer myenteric plexus – nerves that regulate GI motility (skeletal muscle – mouth, pharynx, upper esophagus, anal sphincter) voluntary control of swallowing and defecation 4) Serosa – visceral peritoneum (lines abdominopelvic organs) serous membrane – secretes serous fluid simple squamous epithelium areolar connective tissue (Adventitia – connective tissue around mouth, pharynx, esophagus, rectum) 2 MOUTH (ORAL OR BUCCAL CAVITY) – space containing teeth and tongue; functions in ingestion of food and fluids Cheeks – form walls of mouth; end anteriorly at lips skeletal muscle – positions food in mouth integument lines externally keratinized stratified squamous epithelium oral mucosa lines internally nonkeratinized stratified squamous w/mucous glands Vestibule – space between cheeks (or lips) and teeth Hard and Soft Palates – roof of mouth; lined by oral mucosa hard – maxillae and palatine bones soft – skeletal muscle; covers nasopharynx when swallowing uvula – dangling process Fauces – opening from oral cavity into pharynx Lingual Frenulum – fold of mucosa from floor or mouth to tongue TONGUE functions in sensation and manipulation of food, and bolus formation bolus – ball of food and saliva ANATOMY OF TONGUE skeletal muscle extrinsic muscles – originate on bone and connective tissue around tongue and insert into tongue anchor tongue form floor of mouth move tongue in and out, side to side intrinsic muscles – originate and insert within tongue alter size and shape of tongue aid in manipulating food and producing speech oral mucosa – somewhat keratinized on superior surface papillae filiform – tactile receptors fungiform, circumvallate – taste buds SALIVARY GLANDS – secrete products into mouth saliva – secretions that moisturize and cleanse mouth structures lubricates food and begins chemical digestion COMPOSITION OF SALIVA water (99.4%) solutes (0.6%) mucin (glycoprotein) – forms mucus; lubricates mouth and food ions – Na, Cl, bicarbonate (buffers acidic foods) 3 IgA – antibodies; immune protection lysozyme – bactericide digestive enzymes – salivary amylase (digests starch) lingual lipase (digests triglycerides) Production of Saliva – salivation mucous acini – clusters of cells producing mucus lubricate mouth and food serous acini – clusters of cells producing watery secretions containing digestive enzymes MAJOR SALIVARY GLANDS parotid glands – near ears; serous secretions parotid duct – opens near upper second molar submandibular glands – base of tongue, near mandibles open under tongue; seromucous secretions sublingual glands – under tongue, superior to submandibular glands open under tongue; mucous secretions small salivary glands – found throughout oral mucosa; most secrete mucus lingual glands (tongue) – secrete lingual lipase ANS REGULATION OF SALIVATION parasympathetic – stimulates salivation average 1-1.5 liters/day – swallowing moistens esophagus stimulated by taste, feel, smell, sight, or thought of food sympathetic – inhibits salivation TEETH alveolar processes – maxillae and mandible alveoli – sockets for teeth periodontal ligaments – dense fibrous CT anchors tooth in alveolus shock absorption gingivae (gums) – oral mucosa lining alveolar processes ANATOMY OF A TOOTH Regions of Tooth crown – visible portion above gumline neck – narrowed region in gingival sulcus (pocket) root – portion embedded in alveolus 1-3 roots/ tooth Layers of Tooth pulp cavity – cavity in center of tooth pulp – loose connective tissue w/blood & lymph vessels and nerves 4 root canal – extension of pulp cavity into root of tooth apical foramen – opening at root tip where vessels and nerves enter and exit dentin – main component of tooth harder than bone – 70% calcium salts cementum – outer lining of root; similar to bone enamel – outer lining of crown only hardest substance in body – 95% calcium salts protects tooth from abrasion and acids HUMAN DENTITION – sets of teeth 4 Types of Teeth: 1) incisors – front teeth chisel-shaped; cut food 1 root 2) cuspids (canines) – one cusp (point on crown) pointed; grasp and tear food 1 root 3) bicuspids (premolars) – 2 cusps crush and grind food 1-2 roots 4) molars – back teeth; 4 cusps crush and grind food usually 3 roots Deciduous (primary) Dentition – baby teeth 20 teeth; replaced by adult teeth erupt beginning at 6 months (all by 2-3 years) incisors (8) – central and lateral cuspids (4) primary molars (8) – first and second Permanent (secondary) Dentition – adult teeth 32 teeth erupt beginning at 6 years and into adulthood incisors (8) – central and lateral cuspids (4) bicuspids (8) – first, second molars (12) – first, second, and third first – erupts at 6yr second – 12yr molar third – wisdom tooth (impacted) 5 SUMMARY OF DIGESTIVE FUNCTIONS OF MOUTH ingestion – incisors, cuspids, cheeks & lips, tongue mastication (chewing) teeth grind, tongue and cheeks manipulate, mixed with saliva bolus formation – soft ball of food w/saliva tongue pushes bolus to pharynx for swallowing beginning of chemical digestion salivary amylase - breaks down polysaccharides lingual lipase – breaks down lipids PHARYNX – (nasopharynx), oropharynx, laryngopharynx conducts food and liquid from mouth to esophagus Mucosa of Pharynx: nasopharynx – respiratory epithelium oropharynx and laryngopharynx – oral mucosa PHASES OF DEGLUTITION (swallowing) 1) buccal phase – bolus moved from mouth to oropharynx voluntary tongue moves up and back pushing bolus through fauces 2) pharyngeal phase – bolus moved from pharynx to esophagus involuntary swallowing reflex – integrated in swallowing center (medulla) tactile receptors in pharynx and uvula detect bolus motor neurons stimulate skeletal muscles in pharynx larynx elevated – epiglottis covers glottis soft palate elevated – covers nasopharynx respiratory center inhibited – breathing stops pharyngeal muscles contract – push bolus into esophagus 3) esophageal phase – bolus moves through esophagus into stomach involuntary peristalsis – waves of muscular contraction ESOPHAGUS 10 inch tube from laryngopharynx to stomach posterior to trachea / posterior mediastinum esophageal hiatus – opening through diaphragm hiatal hernia – abdominal organs slip through opening HISTOLOGY OF ESOPHAGUS mucosa – nonkeratinized stratified squamous (abrasion) submucosa – mucous glands (esophageal glands) muscularis – transitions from skeletal to smooth muscle (upper 1/3 is skeletal, lower 1/3 is smooth) adventitia – connective tissue attaches to surrounding tissues of neck and mediastinum 6 FUNCTION OF ESOPHAGUS secretes mucus and transports bolus to stomach upper esopohageal sphincter – relaxes during pharyngeal stage of swallowing esophageal phase of swallowing peristalsis – coordinated contraction and relaxation of circular and longitudinal muscularis regulated by swallowing center and local ENS reflexes lower esophageal sphincter – closed until bolus arrives prevents gastroesophageal reflux heartburn – acid from stomach damages esophageal mucosa STOMACH (GASTRO-) FUNCTIONS OF STOMACH mechanical storage of food churning – mixing and mechanical breakdown of food chyme – soupy mixture of food and secretions secretory – secretes gastric juice (combination of secretions) hydrochloric acid (HCl) denatures proteins – breaks down food tissues activates digestive enzymes pepsinogen pepsin kills bacteria digestive enzymes pepsinogen (active form – pepsin) – digests proteins infants – gastric lipase, rennin – digest milk mucus – protects mucosa of stomach regulatory secretions intrinsic factor – needed to absorb vit. B12 gastrin – hormone that stimulates gastric secretion and motility absorption – minor function some drugs, alcohol ANATOMY OF STOMACH J-shaped; just inferior to liver greater curvature – large, inferior/medial curve lesser curvature – small, superior/lateral curvature rugae – folds in mucosa of empty stomach REGIONS OF STOMACH 1) cardia – superior portion attached to esophagus many mucous glands protect esophagus 2) fundus – rounded superior portion storage portion – stretches to contain large meals 7 3) body – main central portion churning – muscular contractions mix food and secretions 4) pylorus – connects to duodenum pyloric sphincter – allows small amounts of chyme to pass through to duodenum periodically HISTOLOGY OF STOMACH mucosa – simple columnar epithelium surface mucous cells – secrete mucus gastric pits – pits in gastric surface mucous neck cells – mucus gastric glands – produce various secretions parietal cells – HCl, intrinsic factor chief cells – pepsinogen, gastric lipase enteroendocrine cells – gastrin, other hormones submucosa muscularis – 3 layers – assist in churning outer longitudinal middle circular inner oblique serosa REGULATION OF GASTRIC ACTIVITY 1) cephalic phase (head) – taste, smell, sight, thought of food cerebral cortex and hypothalamus stimulated parasympathetic stimulation (CN X) increased secretions and motility 2) gastric phase – food entering stomach stretch receptors and chemoreceptors in stomach submucosal and myenteric plexus reflexes (ENS) increased secretions and motility relaxation of pyloric sphincter enteroendocrine stimulation – increased gastrin secretion stimulates gastric secretions and motility 3) intestinal phase – chyme entering duodenum stretch receptors and chemoreceptors in duodenum enteroendocrine cells in duodenum stimulated release hormones that inhibit gastric functions SMALL INTESTINE – main site of digestion and absorption FUNCTIONS OF SMALL INTESTINE mechanical segmentation – mixing contractions of circular muscles occur when intestine is full peristalsis – slow waves move contents from stomach to large intestine 8 secretory intestinal juice – fluid medium for nutrients and enzymes to interact mucus – alkaline to buffer HCl from stomach enzymes to digest carbohydrates, lipids, proteins, and nucleic acids intestinal enzymes brush border enzymes – attached to mucosal membrane pancreatic enzymes (from pancreas) – secreted into small intestine bile (from liver) – secreted into small intestine emulsifies lipids – breaks up lipid droplets so they can be digested by enzymes enteroendocrine secretions – hormones that coordinate activities of stomach, intestines, liver, and pancreas secretin – inhibits gastric function stimulates liver and pancreatic secretions cholecystokinin (CCK) – inhibits gastric function stimulates pancreatic and gallbladder secretions absorption (site of 90% of absorption) molecules pass through mucosa into blood or lymph circular folds, villi, and microvilli increase surface area for absorption Substances Absorbed in Small Intestine into blood capillaries monosaccharides (carbohydrates) amino acids (proteins) pentoses, phosphates, nitrogenous bases (nucleic acids) electrolytes (ions) water-soluble vitamins water into lymphatic capillaries fatty acids, monoglycerides (lipids) lipid-soluble vitamins micelles – lipids surrounded by bile salts dissolve lipids in intestinal lumen and transport them to mucosa to be absorbed chylomicrons – lipids surrounded by protein coat in mucosa secreted into interstitial space lymph blood ANATOMY OF SMALL INTESTINE Regions of Small Intestine 1) duodenum – proximal portion; attached to stomach retroperitoneal 2) jejunum – middle portion 3) ileum – distal portion; longest ileocecal valve – opening into colon; regulated by a smooth muscle sphincter 9 plicae – folds in mucosa & submucosa from duodenum to mid-ileum increase surface area of mucosa for absorption HISTOLOGY OF SMALL INTESTINE mucosa simple columnar epithelium w/goblet cells villi – finger-like extensions of mucosa and lamina propria increase surface area for absorption microvilli – finger-like extensions of epithelial cell membrane increase surface area for absorption brush border (fuzzy appearance) – brush border enzymes intestinal glands (crypts) – pockets of secretory cells intestinal juice enteroendocrine cells – secretin, CCK, other hormones Peyer’s patches (MALT) lacteals – large lymphatic capillaries in villi extensive capillary network submucosa duodenal glands (Brunner’s glands) secrete alkaline mucus – neutralizes HCl from stomach muscularis – 2 layers serosa REGULATION OF SMALL INTESTINE submucosal and myenteric reflexes (ENS) touch & stretch receptors and chemoreceptors detect chyme increased intestinal motility and secretions enteroendocrine secretions stimulate intestine, liver, pancreas and gallbladder coordination with stomach - parasympathetic stretch reflexes – stomach filling (more stretch) stimulates intestinal function cephalic phase parasympathetic stimulation stimulates intestinal function LARGE INTESTINE FUNCTIONS OF LARGE INTESTINE mechanical haustral churning – haustra (pouches) fill, churn contents, pass contents to the next haustra mass movement – rapid contraction drives contents forward in colon and into rectum 10 secretory – mucus to lubricate feces bacterial flora – normal, symbiotic bacteria living in GI tract ferment carbohydrates – release gases digest peptides – odor bilirubin – converted to a brown pigment produce vitamins – K, biotin, B5 absorption water, vitamins (K, biotin, B5), bile salts form feces – sloughed mucosal cells, bacteria, salts, unabsorbed or indigestible materials (fiber) ANATOMY OF THE LARGE INTESTINE extends from ileocecal valve to rectum Regions of Large Intestine 1) cecum – blind pouch at proximal end appendix – finger-like extension; many lymphoid nodules 2) ascending colon – right abdomen 3) right colic flexure (hepatic flexure) 4) transverse colon – superior 5) left colic flexure (splenic flexure) 6) descending colon – left abdomen 7) sigmoid colon – S-shaped distal end rectum – expands to store feces mucosa – stratified squamous epithelium anus – exit for digestive tract (defecation) internal anal sphincter – involuntary (smooth muscle) external anal sphincter – voluntary (skeletal muscle) HISTOLOGY OF LARGE INTESTINE mucosa simple columnar epithelium reduced surface area (no villi) intestinal glands – long, straight pits into lamina propria many goblet cells – mucus lubricates feces lymphatic nodules (MALT) submucosa muscularis teniae coli – 3 longitudinal bands of smooth muscle tension forms pouches in colon (haustra) serosa fatty appendices – serosal pouches with fat 11 REGULATION OF LARGE INTESTINE activity of small intestine fills proximal colon local ENS reflexes stimulate haustral churning and slow peristalsis gastrocolic reflex – stretch of stomach and duodenum triggers mass movement defecation reflex – triggered by stretch receptors in wall of rectum parasympathetic stimulation of teniae coli in descending and sigmoid colons parasympathetic inhibition of internal anal sphincter somatic reflex (skeletal muscle) contraction of external anal sphincter conscious component relaxation of external anal sphincter contraction of abdominal muscles PANCREAS endocrine function – pancreatic islets regulate blood glucose level exocrine function – secretes pancreatic juice into small intestine COMPOSITION OF PANCREATIC JUICE water, ions sodium bicarbonate – alkaline pH (7.1-8.2) buffers HCl from stomach pancreatic enzymes many – carbohydrases – digest carbohydrates proteases/peptidases – digest proteins/peptides lipases – digest lipids nucleases – digest nucleic acids proenzymes – inactive until activated by intestinal enzymes ANATOMY OF PANCREAS retroperitoneal – behind stomach head – attached to duodenum body and tail pancreatic duct – carries pancreatic juice to duodenum hepatopancreatic ampulla – pancreatic duct and bile duct from liver join duodenal papilla – hepatopancreatic ampulla opens into duodenum hepatopancreatic sphincter – regulates opening (accessory pancreatic duct – empties directly into duodenum) HISTOLOGY OF PANCREAS pancreatic acini – clusters of cuboidal cells; secrete digestive enzymes ducts – epithelium secretes water and bicarbonate pancreatic islets (islets of Langerhans) – secrete hormones 12 REGULATION OF PANCREAS cephalic phase of gastric stimulation parasympathetic (CN X) – stimulates enzyme secretion chyme entering duodenum stimulates enteroendocrine cells CCK – stimulates enzymatic secretions secretin – stimulates bicarbonate secretion LIVER hepatic portal system carries blood and absorbed materials from GI tract to liver for processing before they enter general circulation liver regulates composition of the blood FUNCTIONS OF LIVER 1) carbohydrate metabolism – maintains blood glucose level low glucose glycogenolysis – stored glycogen broken down to glucose gluconeogenesis – amino acids, lactic acid, other monsaccharides converted to glucose high glucose glycogenesis – glucose stored as glycogen lipogenesis – glucose converted to triglycerides (fat) 2) lipid metabolism stores or breaks down triglycerides breaks down fatty acids for energy synthesizes cholesterol 3) amino acid metabolism deamination – removes amino groups (NH2) then converted to carbs or fats, or broken down for energy ammonia (NH3) – toxic by-product of deamination 4) synthesizes plasma proteins (except Igs) albumin, alpha and beta globulins, fibrinogen, prothrombin 5) removal or inactivation of many products in blood detoxification – breaks down may drugs and toxins (eg. alcohol) converts toxic ammonia to urea excretes or stores other drugs and toxins (eg. antibiotics, pesticides) excretes bilirubin – from old blood cells recycles antibodies and hormones (eg. thyroxine and steroids) 6) synthesizes and secretes bile 7) storage glycogen vitamins (A,B12,D,E,K) minerals (iron, copper) 13 8) phagocytosis and antigen presentation Kupffer’s cells – fixed macrophages remove old blood cells, debris, pathogens 9) activation of Vit D (calcitriol) skin, liver, and kidneys participate ANATOMY OF LIVER AND GALL BLADDER largest gland of body immediately inferior to diaphragm falciform ligament – attaches liver to diaphragm and anterior abdominal wall Lobes of Liver right and left lobes (falciform ligament separates) quadrate lobe – inferior, posterior caudate lobe – superior, posterior gallbladder – pear-shaped sac in depression on posterior surface of liver; stores bile from liver BLOOD SUPPLY TO LIVER hepatic artery – branch of aorta hepatic vein – drains from liver to inferior vena cava hepatic portal vein – drains venous blood from GI tract carries nutrients absorbed by GI tract to liver branches into a second capillary bed in liver liver processes nutrients before blood returns to hepatic vein HISTOLOGY OF LIVER lobules – functional units of liver hexagonal (6 sides) central vein – drains into hepatic vein triads (portal areas) at each corner of lobule branch of hepatic artery – brings O2 and hormones to lobule branch of hepatic portal vein – brings GI nutrients to lobule bile duct – drains bile produced in lobule hepatic sinusoids – large capillary spaces connecting central vein to blood vessels of triad Kupffer cells – fixed macrophages in sinusoids hepatocytes – liver cells lining sinusoids process incoming blood produce bile bile canaliculi – ducts which collect bile from hepatocytes drain into bile ducts 14 right and left hepatic ducts – formed by bile ducts converging drain bile from right and left liver lobes common hepatic duct – drains bile into common bile duct OR cystic duct common bile duct – indirectly empties bile into duodenum cystic duct – drains into gall bladder to store bile when hepatopancreatic sphincter is closed COMPOSITION OF BILE 1 quart/day; olive green/yellowish/brownish bicarbonate ions – alkaline pH (7.6-8.6) buffers acid from stomach bile salts – lipids derived from cholesterol amphipathic – have charged and uncharged regions emulsification – break large, insoluble lipid globules into tiny droplets coated by a layer of bile salts (micelles) increases surface area for digestion makes lipids soluble and aids in their absorption (bile salts are removed from lipids as they pass into mucosal cells) bile pigments – from bilirubin; give bile its color REGULATION OF BILE SECRETION following a meal parasympathetic impulses stimulate bile secretion chyme in duodenum stimulates enteroendocrine cells CCK – stimulates contraction of gall bladder relaxes hepatopancreatic sphincter secretin – stimulates bicarbonate secretion from liver bile salts are reabsorbed by large intestine bile salts returning to liver in hepatic portal vein stimulate liver more bile is secreted 15