BIOLOGY PRESENTATION
advertisement
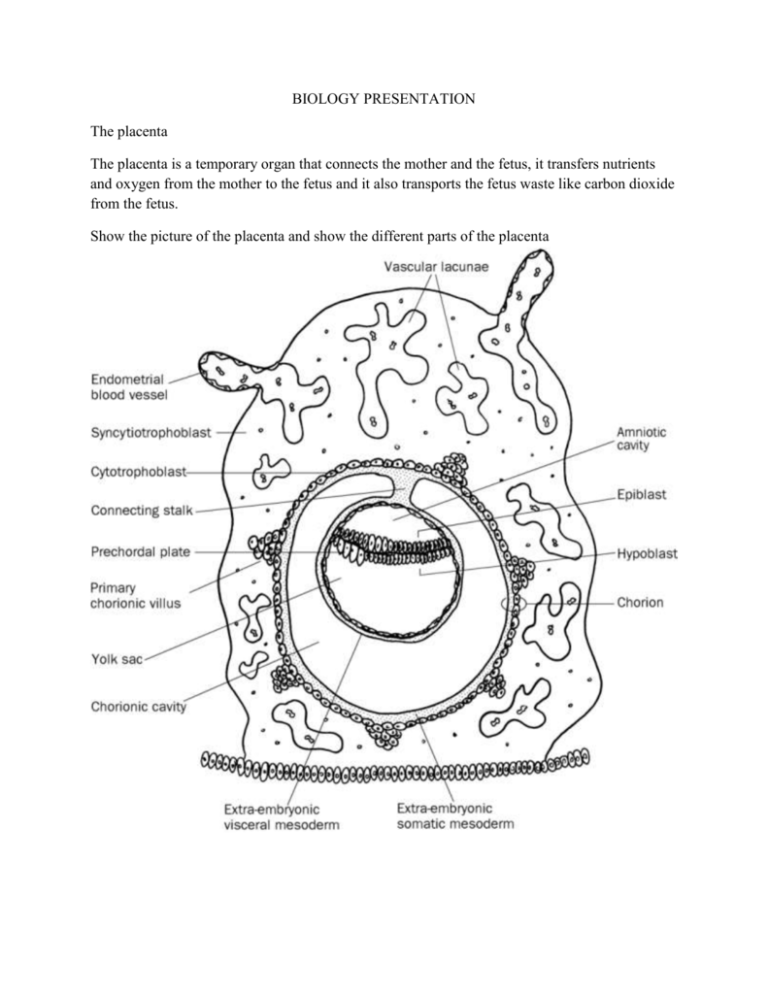
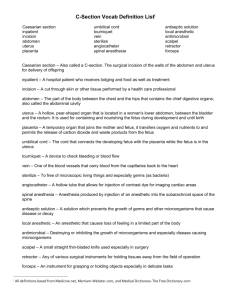
BIOLOGY PRESENTATION The placenta The placenta is a temporary organ that connects the mother and the fetus, it transfers nutrients and oxygen from the mother to the fetus and it also transports the fetus waste like carbon dioxide from the fetus. Show the picture of the placenta and show the different parts of the placenta Placental antigenecity Because it’s a foreign tissue the placenta has much specificity that permits it to stay in the uterus and not be rejected. For example It has been shown that the outer layer of the placenta that is close to maternal blood never expresses MHC class II it’s only normal because we know that MHC II causes causes the activations of CD8 cytotoxic T cells and that would be bad for the embryo. Induced expression of MHC class II in mice caused a 100% abortion. It was also shown that the trophoblast and the syncythiotrophoblast are MHC class I negative in order to evade some immune response. However we learned in class that NK cells not only kill the The MHC containing the wrong peptides, but they also kill cells that don’t express MHC. The reason the cell are still alive is because they express a type of polymorphic MHC I that found in human it’s called HLA-C (human leukocyte antigen) it’s the human MHC and HLA C is the less polymorphic of all the HLA just to keep the barrier as neutral as possible. Immunosuppresion is a way of suppressing the immune response to protect the fetus against rejection. Two scientists called Munn and Mellor have shown that trophoblast IDO (indoleamine 2-3 dioxygenase) prevents tryptophan catabolism of T cells and causes their inactivation and their death in the placenta. Neutralization of IDO in the placenta causes abortion. Injection of IL2 also can cause abortion because it activates CD8 cells and Nk cells. Good effect of father’s antigen After seeing the paternal antigen, NK cells and CD8 T cells express more rPG which is the receptor for progesterone and the high doses of progesterone present induce the secretion of regenrationa dn tolerance factors (RTF) and progesterone induced blocking factors (PIBF). Maternal recognition of paternal antigens is beneficial, because it introduces immune suppression. Immunotrophism Multiparous placentas are bigger and they have more implantation sites. It’s because colony stimulating factors (CSF) like Il-3 and granulocyte macrophages CSF (GM-CSF) produced by the maternal T cells are growth factors for trophoblasts. So the placenta forces the allorecognition (recognition of paternal antigens) by T cells to receive growth factors. The placenta also produces decay accelerating factors to prevent IgG2 from recognizing paternal alloantigens. When it comes to fetal maternal relationships the first question that comes in people’s mind is how does the fetus do to nestle in the uterus and not to be rejected? Because it’s semi allogeneic meaning it has not only antigens from the mother but also antigens from the father which are foreign. It’s even more important for ART (assisted reproduction techniques) where the fetus is totally allogeneic. To answer that question a scientist by the name of Medawar came up with four theories: First he says the uterus is an immunologically privileged site meaning any tissue can be grafted there without rejection. Some scientis have done experiment in which they implanted paternal skin graft in the uterus and it was rejected meaning not any tissue can be implanted on the uterus without rejection only the trophoblast can. Second he said that the fetus is antigenically immature meaning it doesn’t express histocompatibility antigens and the placenta is a neutral barrier between the mother and the fetus. Once again it was shown that indeed the fetus produces Third that there systemic immunosuppression The last theory is that after successive pregnancies, there will be a transferable tolerance to paternal grafts. NK cells and HLA G We talked earlier about HLA C and how it helped prevent killing by the NK cells. It has been found however that the syncytiotrophoblast expresses sHLA-G which is a quasi monomorphic MHC class I antigen and it causes activated T cells to undergo cell death and apoptosis and they can’t induce allorecognition because they are monomorphic. Because in some primates they found that HLA-G was not found in primates and they were still having normal pregnancies, it has been hypothesized that HLA-G is not an absolute requirement for successful pregnancies except for ART. It also has an important role in anti viral defenses because it presents viral peptides. Knocking out Nk cells causes impaired growth of the placenta so it produces growth factors necessary for functional and successful pregnancies. Th1 versus Th2 response During pregnancy, Th1 type cytokines produce proinflammatory responses and excessive proinflammatory responses can cause tissue damage. IFN γ is the main Th1 cytokine. In order to avoid that response there are more Th2 cytokines like IL-10 (anti inflammatory) that are produced during pregnancy that’s why they call it a Th2 phenomenon. In a paper they were trying to show the amount of Th2 cytokines produces show paper explain and they showed that the level of Il-10, Il-3 and GM-CMS increased. GM-CSF and Il-3 fortify placental barriers and help implantation. The Rhesus model The rhesus blood group is more complex than the ABO blood group, it comprises 54 different antigens but the most common is antigen D. We can use a simple model to predict the inheritance with two alleles one D and one small d which doesn’t have the D antigen. So individuals that are DD and Dd are Rh + and individuals that are dd are Rh negative. Rh group incompatibilies can cause serious problems during transfusion but the model that relates to my subject is the mother-fetus imncompatibility. It happens when an Rh negative mother carries and Rh positive baby. At some point during the pregnancy, the fetal red blood cells will enter the maternal circulation and that causes maternal immunization meaning the mother will produce antibodies against the Rh antigen and those IgG will cross the placental barrier and attack the fetal cell. During the first pregnancy, the consequences are pretty low because the mother wasn’t given enough time to produce enough antibodies but in subsequent pregnancies, the antibody titers will increases causing more risk of haemolytic diseases (destruction of the fetus blood cells by the mother’s antibodies). To prevent HDN there can be intrauterine transfusion of compatible blood or inducement of labor after the lungs have matured enough and the mother can also be given Rh immune globulin at 28 weeks of pregnancy and 72 hours after delivery so that the it binds any fetal red cells in the maternal circulation with the Rh antigen before the mother is able to produce an immune response. Anestrus in rodent is a period a sexual inactivity Eostrus: Right before ovulation Proestrus: period of ovarian maturation Irene athanassaki