eAppendix 1: PM2.5 mass and black carbon exposure assessment
advertisement

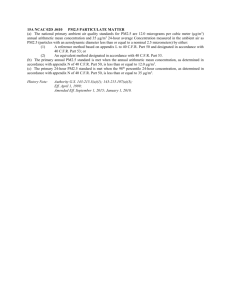
eAppendix 1: PM2.5 mass and black carbon exposure assessment Personal PM2.5 exposure We measured 24-hr personal integrated gravimetric exposure to fine PM (particles <2.5 microns in aerodynamic diameter; PM2.5) in all children using a personal pump (Apex Pro, Casella CEL, Kempston, Bedford, UK) placed inside a small backpack. The pump was connected to a 37 mm Slaton aluminum cassette (BGI Inc., Waltham, MA, USA) holding a 37 mm Teflon filter (SKC Inc., Eighty Four, PA, USA, 2.0 μm pore size) and attached downstream from a GK2.05 (KTL) cyclone with a 2.5 µm aerodynamic-diameter cut point (BGI Inc., Waltham, MA, USA). We attached the cyclone to backpack’s shoulder strap so that it was within the child’s breathing zone. We conducted 2 days of repeat 24-hr exposure measurements in a 10% random sample of study children. Field staff monitored compliance through daily visits to participants’ homes. Children were instructed by field staff to perform routine daily activities and wear the backpack at all times. However, they could place the backpack within 1 meter while sitting or sleeping and within 2 meters during activities when wearing it was impossible (i.e., washing). The Teflon filters were weighed pre- and post-sampling at the Wisconsin State Hygiene Laboratory after being conditioned in a temperature- and humidity-controlled environment (23°C and 40%) for at least 24hr and statically discharged using a polonium source. Filters were weighed in triplicate using a microbalance (MX-5; Mettler-Toledo, Columbus, OH, USA) with a readability of 1 μg. The average of the three closest weights was deemed the final weight for statistical analysis. Detailed information on the study design, data collection and quality control has been previously published.1 Personal black carbon exposure Following gravimetric analysis, we estimated personal 24-hr BC exposure based on reflectance analysis on the same Teflon filters using an optical transmissometer data acquisition system (Model OT21, Magee Scientific, Berkeley, CA, USA). This system provides measurements that are highly correlated with concentrations measured using thermal/optical methods.2 The optical method measures and compares the transmission intensity of light at 880 nm passing through an exposed Teflon filter with that of a blank filter. The resulting light absorption coefficient (ATN) was computed based on the amount of light transmitted through the exposed filter (I) and the amount transmitted through the blank filter (I0), where ATN = 100ln(I0/I). We determined BC density (μg/cm2) by dividing the ATN by the specific attenuation coefficient σ ATN, using the relationship, BC = ATN/σATN.3 We converted BC density to BC exposure concentration based on the total volume of air (m3) that passed through the exposed filter during 24-hr pollution measurement period. The instrument was re-zeroed with a blank filter between measurements. Empirical correction for BC at higher concentrations BC is defined as the fraction of carbonaceous aerosol absorbing light over a broad region of the visible spectrum, and is measured by determining the attenuation of light (ATN) transmitted through a sample filter. Previous studies have found that the relationship between ATN change and BC concentration is not linear.4-6 There are several reasons for this non-linear relationship, including that both scattering and absorbing particles collected on the filter alter the internal reflection of the filter such that it that changes the absorption of the aerosol/filter combination.5,7 As a result, an underestimation of measured aethalometer signals (ATN or BC mass concentrations) increases as the sample filter becomes darker and more loaded (i.e., the BC concentrations increase). To account for this underestimation of the ATN at higher BC concentrations, we applied an empirical correction using a previously derived formula. This formula is based on measured 24-hr ambient air pollution concentrations (n=334) in downtown Los Angeles, CA. To empirically derive the correction factor, we first estimated the empirical relationship between EC and BC using ambient air pollution samples in Los Angeles, for which a quadratic relationship was the best fit (R2=0.90). Knowing that the values of measured BC are underestimated at higher levels, we started with the estimated value of EC based on the observed quadratic relationship between EC and BC. Then, for any given level of BC, we estimated a corrected value of BC based on the linear relationship between EC and BC for BC values less than 4.07 μg/cm2 (Appendix Figure 1; data not published). We applied the correction factor to the original value of BC in our data set using the equation: BC=1.3*((0.1*BC02)+(0.5*BC0))+0.7 Eq. (1) Here, BC is the corrected BC exposure level and BC0 is the measured BC exposure level. We applied Eq. (1) to all measured BC concentrations in our study. Our results with the analysis using the corrected BC values were not different from the analysis using the uncorrected BC values (results not reported). Figure A1. The measured (blue diamond) and corrected (purple cross) values of BC using data from Los Angeles. The grey line is the predicted linear relationship between measured BC and EC based on the BC/EC relationship for BC values less than 4.07 μg/cm2 (n=287) and the black line is the predicted quadratic relationship between BC and EC based on all data (n=334). eAppendix 2: Measurement of blood pressure and other covariates Blood pressure measurement Children’s BP measurements were conducted at the village primary school between 8 and 10 AM using an automated device (Omron-705, Omron Corp) that has been validated against a mercury sphygmomanometer in normotensive children and adolescents according to the revised protocol of the British Hypertension Society.8 Following ≥5 min of quiet rest, three consecutive resting BP measures were taken, one minute apart, on the supported right arm of the seated child using an appropriate cuff size.9 We recorded the date, time and room air temperature during BP measurement. The average of the last two measures was used as the child’s average BP for that day. Questionnaires and other measurements We interviewed an adult in the child’s home and collected socio-demographic and health information for each child including age, gender, mother’s education, current medication use and physician-diagnosed diabetes. Passive smoking status was assessed by asking about the number of tobacco smokers who lived for 9 or more months per year in the child’s household. We used principal component analysis to derive a composite socioeconomic score for each household using data on the ownership of 17 household assets.10 We measured each child’s height (cm) and weight (kg) and calculated body mass index (BMI) as weight (kg) divided by squared-height (m2). Physical activity was assessed using 24-hr pedometer measurements, which may be a more valid and accurate measure of physical activity than selfreported activity patterns for young children.11 We estimated 24-hr salt and monosodium glutamate (MSG) intake by weighing the child's household salt and MSG containers at the beginning and end of a 24-hr period, taking the difference in weights and dividing it by the number of household residents. In a sub-sample of the study children (n=94; 40%), BP measurement was also performed on their mothers who were enrolled in a separate study.12 eAppendix 3: Statistical analysis Statistical analysis was conducted using Stata 11.0. We examined the distributions of all variables and calculated summary measures accordingly. Both PM2.5 and BC exposure concentrations were transformed to the natural log scale in order to account for their skewedness to high values.13 For children with more than one day of PM2.5 and BC exposure measurement, we used the mean exposure for all measurement days in the analysis. Multivariate linear regression models were used to quantify the association between PM2.5 and BC with SBP and DBP, while adjusting for potential confounders. Specifically, we controlled for child’s age, gender, height, BMI, physical activity (24hr pedometer/1000), grams of salt intake, whether or not MSG was consumed in the household, passive smoking (number of smokers in the household), mother’s years of education, household socioeconomic status, day of the week (weekday/weekend day), and the 24-hr average ambient air temperature during pollution monitoring. We conducted our regression models using the BP measurement taken after the 24-hr pollution measurement. We retained potential confounders in the final model if they were associated with BP at p<0.10 or if they changed the estimated effect of PM2.5 or BC exposure on BP by ≥10%.14 We used a robust variance estimation for cluster-correlated data in the regresion models to account for the fact that observations from children from the same household cannot be considered independent.15 eAppendix 4: Results and Sensitivity Analyses In univariate regression models, age (SBP: 1.4 mm Hg, 95% CI: 0.9, 1.8; DBP: 0.4 mm Hg, 95% CI: 0.1, 0.7), height (SBP: 0.2 mm Hg, 95% CI: 0.2, 0.3; DBP: 0.1 mm Hg, 95% CI: 0.0, 0.2), BMI (SBP: 1.8 mm Hg, 95% CI: 1.3, 2.2; DBP: 0.6 mm Hg, 95% CI: 0.2, 0.9) and gender (SBP: -2.1 mm Hg, 95% CI: -4.2, -0.1) were significantly associated with higher BP (P<0.05). Physical activity (i.e., number of steps/1000) was borderline significantly associated with lower SBP (-0.3 mm Hg, 95% CI: -0.6, 0.0) (results not presented). A 1-ln(µg/m3) increase in both PM2.5 and BC was associated with a decrease in SBP and DBP in the univariate models and after adjusting for known risk factors for higher BP in children, including age, gender, height and BMI (Appendix Table 2). Sensitivity analyses In an analysis restricted to the sub-sample of children with maternal BP information, we found that maternal DBP was significantly associated with a small but significant change in children’s SBP (0.2 mm Hg, 95% CI: 0.1, 0.3) and DBP (0.2 mm Hg, 95% CI: 0.1, 0.3) in the multivariate analysis. However, inclusion of maternal BP did not change the estimated effects of PM2.5 or BC exposure on BP and, therefore, we excluded maternal BP from our final models (results not presented). None of our pollution-BP associations were modified by gender or passive smoking status (all interaction pvalues>0.50). Also, while we adjusted for age and height, we did not have information on the children’s hormonal levels or age of puberty onset. BP is known to rise progressively with age and height, and may increase more rapidly during puberty.16 We examined this source of potential bias by limiting our analysis to girls ages 10-14 years old (n=73) and boys ages 12-14 years old (n=51). The effects of PM2.5 and BC in these groups were similar to those observed when all children were included in the analysis (data not shown). Therefore, our findings cannot be explained by different level of sexual maturity in exposed and non-exposed children. Further, it suggests that residual confounding by age does not explain our results when all study children (ages 5-14 years old) are included in the same analysis. As a final sensitivity analysis, we transformed SBP and DBP values into quantiles (10th, 25th, 50th, 75th and 90th), and re-conducted our single-pollutant multivariate regression models using (Appendix Table 3). Though the results with linear regression (i.e., continuous SBP or DBP) were an under- or over-estimate for some quantiles, the qualitative interpretation of our results using continuous SBP and DBP did not change. eAppendix 4: Discussion of possible mechanisms Although changes in BP in response to acute exposure to ambient PM could be explained by autonomic nervous system responses, persistent changes may take years to occur. The association between sodium intake and higher BP has been shown to strengthen with increasing age in a large meta-analysis, suggesting a possible cumulative burden over time.17 It is possible that BP effects of PM2.5 and BC exposure were not observed in our study because exposure for prolonged periods of time is required for persistent changes in the physiologic mechanisms involved in BP control, such as neurohormonal regulation of arterial tone and control of body fluids by the kidney. We have recently reported that the effect of PM2.5 exposure from biomass smoke on BP among adult women is dependent on age, with the strongest effects observed among women over 50 years old.12 Further, mechanisms that potentially mediate an effect of PM inhalation on prolonged increases in BP may need to occur over long periods of exposure.18 A persistent increase in BP among older adults occurs after a resetting to higher values of the level of BP that normally results in renal-pressure natriuresis, a process that is likely to occur only as a consequence of repeated acute increases in BP after PM inhalation. In contrast, children in our study were probably too young for developing an abnormal renal-pressure natriuresis despite persistent PM2.5 exposure. It is also a possible that the concentrations of PM2.5 and BC exposure among children were too low to induce a significant change in BP. The average personal PM exposure observed among children in our study (meanstandard deviation-SD: 5847 µg/m3) was lower than the personal exposures observed among adult women living in the same villages and during the same time period (meanSD: 8081 µg/m3).1 Nevertheless, personal PM2.5 exposure concentrations for children in our study were higher than those observed among ETS-exposed children in an urban setting (mean=37 µg/m3; range: 21-60)19, and ETS exposure has been associated with small increases in BP in preschool children.20 Though, the chemical composition of emissions from burning tobacco and wood differs, and studies in adult populations indicate that the composition of PM may affect its cardiovascular impacts.21 eTable 1. Socio-demographic characteristics of the study children by exposure Variable Age (years) 5-8 9-11 12-14 Gender Male Female BMI-for-age a Severe thinness (<-3 SD) Thinness (≥-3 SD – <-2 SD) Normal (≥-2 SD – ≤+1 SD) Overweight (>+1 SD – ≤+2 SD) Socioeconomic status Quartile 1 Quartile 2 Quartile 3 Quartile 4 Passive smoking status None 1 smoker 2+ smokers Salt intake (mean, SD; grams) Height (mean, SD; meters) Maternal education (mean, SD; years) Systolic blood pressure (mean, SD; mm Hg) Diastolic blood pressure (mean, SD; mm Hg) Below median PM2.5 exposure No. (%) (n=120) At or above median PM2.5 exposure No. (%) (n=120) All children 14 (12) 50 (42) 56 (47) 47 (39) 37 (31) 36 (30) 61 (25) 87 (36) 92 (38) 58 (48) 62 (52) 67 (56) 53 (44) 125 (52) 115 (48) 8 (7) 4 (3) 12 (5) 21 (18) 22 (18) 43 (18) 89 (74) 89 (74) 178 (74) 2 (2) 5 (4) 7 (3) 26 (22) 36 (30) 32 (27) 26 (22) 34 (28) 25 (21) 27 (23) 34 (28) 60 (25) 61 (25) 59 (25) 60 (25) 23 (19) 81 (68) 16 (13) 16 (13) 80 (67) 24 (20) 39 (16) 161 (67) 40 (17) 5.0 (1.8) 5.2 (1.9) 5.1 (1.9) 1.3 (0.1) 1.4 (0.1) 1.4 (0.1) 6.7 (2.7) 7.1 (2.6) 6.9 (2.7) 103.7 (8.2) 100.5 (8.2) 102.1 (8.4) 64.6 (6.5) 62.6 (6.5) 63.6 (6.5) No. (%) (n=240) BMI; body mass index as calculated by weight (kg) divided squared height (meters) No; number of children SD; standard deviation a Based on the WHO’s BMI-for-age growth charts for girls and boys ages 5-19 years.22 eTable 2. Effects of personal PM2.5 and BC exposure (ln(µg/m3)) on blood pressure in univariate single pollutant models (I, III), single pollutant models adjusted for age, height, BMI and gender (II, IV) and two pollutant models adjusted for age, height, BMI, gender (V)a I Systolic blood pressure PM2.5; ln(µg/m3) -3.5 (-5.5, -1.5) 3 BC; ln(µg/m ) Age; years Height; cm BMI; kg/m2 Female gender Difference in mm Hg, (95% CI) II III IV -2.1 (-3.9, -0.3) -4.4 (-8.2, -0.7) -0.6 (-1.5, 0.2) 0.2 (0.1, 0.4) 1.4 (0.8, 2.0) -1.3 (-3.1, 0.6) -2.6 (-5.8, 0.6) 0.5 (0.1, 0.4) 0.2 (0.1, 0.4) 1.3 (0.8, 1.9) -1.3 (-3.1, 0.6) V -1.7 -1.0 -0.6 0.2 1.4 -1.4 (-3.8, 0.3) (-4.6, 2.5) (-1.5, 0.3) (0.1, 0.4) (0.8, 1.9) (-3.2, 0.5) Diastolic blood pressure PM2.5; ln(µg/m3) -1.8 (-3.3, -0.3) -1.3 (-2.9, 0.2) -1.2 (-2.9, 0.7) 3 BC; ln(µg/m ) -2.2 (-4.9, 0.6) -1.7 (-4.5, 1.1) -0.6 (-3.9, 2.6) Age; years -0.6 (-1.3, 0.2) -0.6 (-1.4, 0.1) -0.6 (-1.4, 0.1) Height; cm 0.1 (0.0, 0.3) 0.1 (0.0, 0.2) 0.1 (0.0, 0.2) 2 BMI; kg/m 0.6 (0.1, 1.0) 0.5 (0.2, 1.0) 0.6 (0.2, 1.0) Female gender 1.6 (-0.1, 3.3) 1.6 (-0.1, 3.3) 1.6 (-0.2, 3.3) BC; black carbon BMI; body mass index CI; confidence interval PM; particulate matter a The “effect” is the estimated difference in blood pressure associated with a one-unit increase in the natural log of PM2.5 or BC. eTable 3. Comparison of the effects of personal PM2.5 and black carbon exposures (ln(µg/m3)) on blood pressure using linear and quantile regression (10th, 25th, 50th and 90th blood pressure quantiles)a Difference in mm Hg, (95% CI) Linear regression Systolic blood pressure PM2.5 Black carbon Diastolic blood pressure PM2.5 Black carbon 10th 25th 50th 75th 90th -1.8 (-3.6, 0.1) -0.7 (-2.9, 1.4) -0.5 (-2.3, 2.1) -1.8 (-4.0, 0.4) -1.3 (-4.2, 1.6) -2.9 (-6.3, 1.6) -2.2 (-5.4, 1.0) -1.1 (-4.9, 2.7) -2.7 (-7.3, 1.9) -2.5 (-6.7, 1.8) -1.5 (-7.6, 4.6) -2.3 (-10, 5.5) -0.5 (-2.1, 1.2) -0.1 (-1.8, 1.6) -0.4 (-3.3, 2.6) 0.9 (-2.8, 4.6) -0.5 (-2.0, 1.1) 0.8 (-2.4, 4.0) 0.2 (-2.2, 2.6) -0.1 (-2.1, 1.8) -1.2 (-3.8, 1.3) 0.8 (-4.1, 5.8) -0.4 (-5.9, 5.0) -0.4 (-5.8, 5.0) CI; confidence interval PM; particulate matter a The “effect” is the estimated difference in blood pressure associated with a one-unit increase in the natural log of PM2.5 or black carbon for each blood pressure quantile using single-pollutant models. References 1. Baumgartner J, Schauer J, Ezzati M, et al. Patterns and predictors of personal exposure to indoor air pollution from biomass combustion among women and children in rural China. Indoor Air. 2011; 21:479–488 2. Ahmed T, Dutkiewicz VA, Shareef A, et al. Measurement of black carbon (BC) by an optical method and a thermal-optical method: Intercomparison for four sites. Atmos Environ. 2009; 43:6305-6311 3. Magee Scientific Company. Dual-wavelength optical transmissometer data acquisition system manual. 2007 4. Reid JS, Hobbs PV, Liousse C, et al. Comparisons of Techniques for Measuring Shortwave Absorption and Black Carbon Content of Aerosols from Biomass Burning in Brazil. J Geophys Res. 1998, 103: 32031-32040. 5. Bond TC, Anderson TL, Campbell D. Calibration and Intercomparison of Filter-Based Measurements of Visible Light Absorption by Aerosols. Aerosol Sci Technol. 1999, 30: 582-600. 6. Arnott WP, Moosmuller H, Sheridan PJ, et al. Photo-acoustic and Filter-Based Ambient Aerosol Light Absorption Measurements: Instrument Comparisons and the Role of Relative Humidity. J Geophys Res. 2003, 108:4034 7. Clarke AD, Noone KJ, Heintzenberg J. et al. Aerosol Light Absorption Measurement Techniques: Analysis and Intercomparisons. Atmos. Environ. 1987, 21:1455-1465. 8. Stergiou G, Yiannes N, Rarra V. Validation of the Omron 705 IT oscillometric device for home blood pressure measurement in children and adolescents: The Arsakion school study. Blood Press Monit. 2006; 11:229-234 9. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004; 114: 555-576. 10. Filmer D, Pritchett LH. Estimating wealth effects without expenditure data-or tears: An application to educational enrollments in states of india. Demography. 2001; 38:115-132 11. Rowlands AV, Eston RG, Ingledew DK. Measurement of physical activity in children with particular reference to the use of heart rate and pedometry. Sports Med. 1997; 24:258-272 12. Baumgartner J, Schauer JJ, Ezzati M, et al. Indoor air pollution and blood pressure in adult women living in rural China. Environ Health Perspect. 2011; 119:1390-1395 13. Pope 3rd CA, Burnett RT, Krewski D, et al. Cardiovascular mortality and exposure to airborne fine particulate matter and cigarette smoke: Shape of the exposure-response relationship. Circulation. 2009; 120:941-948 14. Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989; 79:340-349 15. Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000; 56:645–646 16. Voors AW, Foster TA, Frerichs RR, et al. Studies of blood pressures in children, ages 5–14 years, in a total biracial community: The Bogalusa heart study. Circulation. 1976; 54:319-327 17. Law MR, Frost CD, Wald NJ. By how much does dietary salt reduction lower blood pressure? I–analysis of data from trials of salt reduction. BMJ. 1991; 302:819-824 18. Brook RD, Rajagopalan S, Pope 3rd CA, et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010; 121:2331-2378 19. Janssen N, Hoek G, Harssema H, et al. Personal exposure to fine particles in children correlates closely with ambient fine particles. Arch Environ Health: An Int J 1999; 54:95-101 20. Simonetti GD, Schwertz R, Klett M, et al. Determinants of blood pressure in preschool children: The role of parental smoking. Circulation. 2011; 123:292-298 21. Brunekreef B, Janssen NA, de Hartog JJ, et al. Personal, indoor, and outdoor exposures to PM2.5 and its components for groups of cardiovascular patients in Amsterdam and Helsinki. Res Rep Health Eff Inst. 2005; 127:1-70; discussion 71-79 22. World Health Organization. WHO Reference 2007: Growth reference data for 5-19 years. http://www.who.int/growthref/en/ Accessed October 15, 2011.