Urinary Catheter ()

SCOPE:
All clinical areas of Fort Sanders Regional, PNRC, TCU, and ancillary departments affiliated with Fort Sanders Regional. All Healthcare workers who insert and maintain indwelling urinary catheters are responsible for adhering to this policy.
PURPOSE:
To define the infection prevention and control standard for the insertion and maintenance of indwelling urinary catheters for patient care personnel. These guidelines are to aid in standardizing a patient care process. Specific care needs of the individual patient may warrant deviation from the guidelines.
POLICY STATEMENT:
This policy shall be approved by the Infection Control Committee and the Medical Executive
Committee of Fort Sanders Regional Medical Center. This policy outlines the responsibilities of the Medical Staff, Nursing Service, and other personnel who have direct or indirect contact with patients with indwelling urinary catheter.
PROCEDURE:
Provisions:
1. Personnel: Only healthcare workers who are competent in the correct technique of aseptic insertion and maintenance of urinary catheters shall handle urinary catheters.
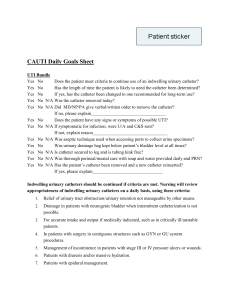
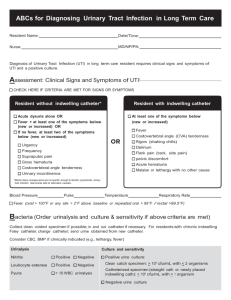
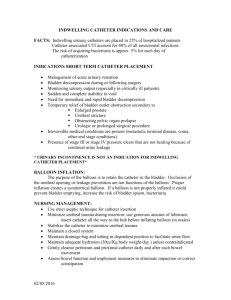
2. Utilization: Because the majority of nosocomial UTIs are associated with the use of an indwelling urinary catheter, careful evaluation of the initial indication of catheterization and the need for continued catheterization is necessary. Indwelling urinary catheters are inserted only when medically indicated and left in place only for as long as clinically needed due to the potential for complications.
The following are justifications for Foley catheterization: a. The patient requires hourly monitoring of urine output as determined by a physician. b. The patient requires the use of large dose diuretics. c. The patient requires the use of continuous or frequent paralytic agents, intravenous sedatives, and/or analgesics. d. The patient requires an indwelling urinary catheter to manage bladder outlet obstruction. e. The patient requires an indwelling urinary catheter as a comfort measure for the terminally ill patient. f. The patient requires an indwelling urinary catheter for the incontinent patient with perineal/ sacral skin breakdown, or the patient is at high risk for skin breakdown due to incontinence and has limited mobility or communication deficits (ex. Patricia Neal Rehabilitation). g. The patient is in the immediate (24-48 hour) post-op period. h. The patient requires has a
chronic history of indwelling or suprapubic catheter.
3. Hand Hygiene: Wash hands and wear gloves and before and after manipulating the catheter.
4. Insertion: a. Obtain the correct urinary drainage kit: i. Urometer for a patient admitted, to be admitted to critical care, or when the patient requires strict urine output measurement. ii. Coude kit for the patient who requires a coude catheter. iii. Latex free kit for the patient who has latex allergy.
b. Insert catheter using sterile technique and sterile equipment. c. Use gloves, drape, sponges, and appropriate antiseptic solution for periurethral cleaning and lubricant jelly for insertion. d. Use the smallest catheter consistent with good drainage, to minimize trauma. e. After insertion, secure indwelling catheter with a securement device or tape to the patient’s leg, to prevent movement and urethral traction. f. Label the collection device with the catheter insertion date.
5. Initiate the UTI Prevention Intervention Bundle: a. No dependent loops b. Drainage bag below bladder c. Drainage bag not touching floor d. Bag emptied when ½ full e. Catheter secured to leg f. Tubing to foley seal in intact g. Collection device labeled with insertion date
6. Catheter Drainage System Manipulation: a. Hand washing precedes and follows each manipulation. Exam gloves are worn if hand contact with urine is anticipated. A gown and protective eyewear are worn if splashing of urine is anticipated. b. Use a sterile, closed continuous drainage system. c. Do not disconnect the catheter from the drainage tube unless irrigation is necessary for diagnostic or therapeutic reasons or the catheter cannot be irrigated through the sampling port. d. Aseptic disconnection of the closed drainage system is permitted when intermittent irrigation is required for bleeding or clot obstruction. Alcohol preparation of the junction precedes disconnection. e. If the catheter becomes obstructed and can be kept open only by frequent irrigation, the catheter is changed if the catheter itself is likely to be contributed to the obstruction.
7. Specimen Collection: a. To examine small volumes of fresh urine, clean and disinfect the sampling port, and aspirate urine from the sampling port (urinary catheter tips should not be cultured and are not acceptable for the diagnosis of a urinary tract infection). i. Urine specimens for culture should be processed as soon as possible, preferably within 1 to 2 hours. ii. If urine specimens cannot be processed within 30 minutes of collection, they should be refrigerated or inoculated into primary isolation medium before transport, or transported in an appropriate urine preservative. iii. Refrigerated specimens should be cultured within 24 hours. b. Large volumes of urine for special analysis are aseptically obtained from drainage bags.
The drainage bag outflow spigot is not to contact the inside of the collection container. c. Disinfect t he spigot with alcohol before placing back into the drainage bag’s holder.
8. Urinary flow: a. Unobstructed urinary flow is maintained except for temporary obstruction of the catheter for specimen collection, or for other medical purposes as necessary. b. Attach the foley collection bag to the foot of the bed so as to achieve a free flow of urine and prevent the catheter and collection tube from kinking or from developing dependent loops. i. If the patient is reclined in the chair, hang the bag from the foot rest of the recliner
(the metal joint that raises the foot rest) or move the chair close enough to the bed so the catheter can hang on the bed, below the level of the bladder.
Note: The drainage bag will be kept below the level of the bladder at all times for patients when participating in rehabilitation activities. c. Irrigation, for any reason, must have a physician order and is performed using aseptic technique. i. Bottles of irrigation solutions are dated and timed when opened and discarded every 24 hours. ii. Syringes and solution container are discarded after each use. d. The drainage collection device is kept less than half full and emptied regularly using a separate container for each patient. e. The graduated urine measuring container is rinsed with tap water and stored in a manner that facilitates drying after each use. One graduated container is issued to each patient as needed, labeled with the patient’s name, and discarded when no longer in use. f. Always keep drainage bags below the level of the bladder.
9. Once bladder is empty, unless specifically ordered by the physician, a catheter should not be clamped. If ordered, the frequency and period of time the catheter is to be clamped should be clearly identified. Ureteral catheters are never clamped.
10. Perineal Care: The perineum is gently washed daily with soap and water and as needed unless otherwise ordered by Physician.
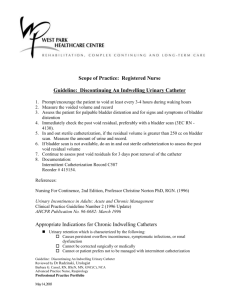
11. Indwelling catheters should not be changed at arbitrarily fixed intervals. Catheters should be changed when: a) Concretions can be felt at the lumen b) Contamination occurs c) Malfunctions or obstructions are suspected
12. Cultures: When ordered, urine cultures are aseptically obtained from the aspiration port.
13. Assessment Procedure: During the Nursing shift assessment if indwelling urinary catheter is present, ask the question “Does catheter fit criteria in #2 of this policy?” if answered with a “yes”, continue routine care and assessment daily, if answered with a “no”, request to remove catheter based on criteria in #2 above.
Place completed form in patient’s chart under the Nursing Documentation tab.
Ensure to fill out the date the catheter is discontinued and nurse signature.
References :
Mezey, M.D., Fulmer, T., & Abraham, I. (2003) Geriatric Nursing Protocols for Best Practice.
New York: Springer Publishing Co., Inc. p 83-98.
Smith, Duell, and Martin. Clinical Nursing Skills: Basic to Advanced Skills. Fifth Edition,
2000
Wong, E. (with Hooton, T. and Working Group). (n.d). Guideline for prevention of catheter-associated urinary tract infections. Retrieved from http://www.cdc.gov/ncdod/hip/guide/uritract.htm
CDC “Guideline For Prevention of Catheter-Associated Urinary Tract Infections 2009”
Healthcare Infection Control Practices Advisory Committee. http://www.cdc.gov/ncidod/dhqp/pdf/guidelines/CAUTI Guideline2009final.pdf
Willson, M., Wilde,M.,Webb, M.,Thompson,D.,Parker,d.,Harwood,J.,Callan,L.,Gray,M.,
Journal of Wound, Ostomy and Continence Nursing, March/April, 2009, Volume 36 Number
2, Pages 137-154.
Fundamentals of Nursing 7 th Edition. 2009. Potter/Perry-Mosby.