Applied capitalization as recommended by CAT (item # 14).
advertisement

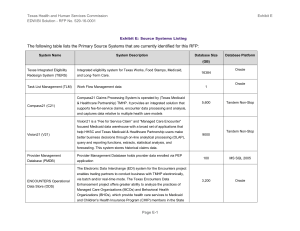
Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 Future Scope Future Scope: Enterprise Data Warehouse / Business Intelligence Solution The Enterprise Data Warehouse / Business Intelligence (EDW/BI) Solution will be designed with the flexibility to incorporate additional data sources and expand the capacity, performance, and functionality through services rendered to accommodate potential future scope, while still ensuring integrity of the long term architectural vision. This document provides information relating to potential additional Functional Requirements, Source Systems, Data Sources, and Services or Software intended to enhance EDW functionalities in the future. The Cost Proposal for the EDW/BI Solution for this RFP should not include any pricing for potential future scope. As specified in the Project Overview (Section 1.6.2.) of the EDW/BI Request for Proposal (RFP), the Respondent's Solution will have the capacity and flexibility to acquire additional data sources and perform all future functions and services as a part of the Future Scope. Table 1 Potential Additional Functional Requirements, within this document, lists the potential additional Functional Requirements that will be supported through the implementation of Future Scope functionality into the Solution. Future Scope additional services will include but may not be limited to buying additional hardware, software, adding additional data sources, enhancing the Solution's functionality, improving the system's scalability, and providing services that are within the scope of this RFP and any awarded Contract. Within the HHS Enterprise are additional source systems that are out-of-scope for the Solution's initial development but which offer data that can enhance views of health care services and histories. These systems typically contain transactions related to Medicaid clients (or services provided to them) but which are overseen by the following agencies outside HHSC: Texas Department of Aging and Disability Services (DADS) Texas Department of Assistive and Rehabilitative Services (DARS) Texas Department of Family and Protective Services (DFPS) Texas Department of State Health Services (DSHS) A list of potential additional source systems within the HHS Enterprise in provided in Table 2 Potential Additional Source Systems of this document. It should be noted that recommendations from the recent Sunset Advisory Commission Report (October 2014) are expected to create many requirements for additional data integration across current agency boundaries. In addition, the EDW will be able to obtain these additional sources of data and services in order to support and extend the comprehensiveness of data collections previously established. As the maturity of health care information increases across Texas, there will likely be opportunities to enhance Medicaid client history information with transaction data arising from clinical systems where Medicaid client receive treatment. Integrating clinically relevant data into the EDW that was previously unavailable within administrative data sets in HHSC (claims or encounter transactions) will offer new potential opportunities to measure and track Medicaid client outcomes. For example, supplementing the EDW data from electronic health records (EHRs) can fill information gaps related to services for Medicaid clients, both inside and outside their periods of Medicaid eligibility. Lists of potential additional data sources and additional services are provided in Table 3 – Potential Additional Data SourcesTable 3 and Table 4 – Additional Services or Software for Data Connectivity, respectively, in this document. 1 Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 Future Scope EDW Future Scope: Potential Additional Functional Requirements The following potential additional functional requirements, listed in Table 1 below, are provided to Respondents in order to provide information concerning the expected long term development strategy of the EDW. These requirements are outside the scope of this RFP. However, it is expected that the Solution should be able to be modified and enhanced to accommodate future objectives. Additional functional requirements assessment and alignment of EDW capabilities to business objectives are expected to be necessary before future projects can begin. Note that additional details about each requirement are included in Appendix A: Detailed Functional Requirements – Potential Future Scope in this document. Table 1 - Potential Additional Functional Requirements FR ID Functional Requirement Description FR015 Use Vital Statistics to notify business units of client life changes FR018 Integrate DSHS registries with client records. FR076 Implement enterprise view across agencies of case management portfolio. Determine availability in comparable programs (Medicaid). FR003 FR006 FR021 FR041 FR043 FR020 Monitor [cost] impact of migration between programs and services (including both internal and external as available). Integrate service data from the All Payers data (Texas Healthcare Information Collection (THCIC) Data). Expose streams of care episodes that cross programs or departments or agencies. Assess comparable services within and across all agencies. Incorporate public health strategy program data (e.g., immunizations, smoking cessation). Stage Topic/Domain Client, Provider, and Enrollment Visibility Client, Provider, and Enrollment Visibility Client, Provider, and Enrollment Visibility Client, Provider, and Enrollment Visibility Service Delivery Client Service Delivery Client Service Delivery Services Service Delivery Service Delivery (Episodes of Care) Services Client Client Case Program Program FR061 Provide a single view of Medicaid services across programs/agencies. Service Delivery (Episodes of Care) Continuity FR078 Compare client outcomes across case management programs. Service Delivery Services FR028 Identify people without health insurance. Client Historical Information Client FR066 Integrate Vendor drug by incorporating drugs prescribed through private insurance providers. Client Historical Information Continuity FR067b Integrate health data from private insurers. Client Historical Information Continuity FR068 Integrate data about veterans who are also clients from the Veterans Administration Client Historical Information Client 2 Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 Future Scope EDW Future Scope: Potential Additional Source Systems The following Table 2 lists the potential additional Source Systems for the EDW that are identified for future scope and are provided to Respondents in order to provide information concerning the expected long term development strategy of the EDW. These potential additional source systems are outside the scope of this RFP. However, it is expected that the Solution should be able to be modified and enhanced to accommodate future objectives. All of these data sources are within HHS agencies. Table 2 - Potential Additional Source Systems System Count Agency 1 DADS 2 3 EDW Source Systems Source System Name Source System Description CARES Compliance, Assessment, Reporting, and Enforcement System Supports regulation of long-term care facilities to ensure that all federal and state regulations are met. This is the primary state system used by regulatory services staff. The system includes Wafer and CARES Reporting interfaces. Sybase 7 DADS CMS ICF/MR PRV PMT Intermediate Care Facilities for Persons with Mental Retardation Provider Payment System DADS Claims Management System’s ICF/MR Provider Payment System– calculates provider payments and federal funds requests, performs HIPAA reconciliation, and retains supporting client-level claim data for audit and reporting purposes. Oracle 10 DADS CSIL Community Services Interest List Community Services Interest List (CSIL) is a web-based application for keeping track of individuals waiting to receive services in various Community Care programs. CSIL replaces the manual tracking systems used by different community care programs. Oracle 1 3 Database Type System Size (Gb, as of Jan 2014) Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 System Count Agency 4 5 Future Scope EDW Source Systems Source System Name Source System Description DADS HCS PRV PMT Home and Communitybased Services Provider Payment System Home and Community-based Services Provider Payment (HCS PRV PMT) system calculates provider payments and federal funds requests, performs HIPAA reconciliation, and retains supporting clientlevel claim data for audit and reporting purposes. Interfaces with HCS, MARS/G Accounts Payable, and General Ledger. Oracle 50 DADS HCSSA DADS licenses, certifies and surveys Home and Community Support Services Agencies (HCSSAs) for compliance with state and federal laws and regulations. Oracle 1 The Client Assignment and Registration System (CARE) system is the central client database for Mental Health (MH) and Mental Retardation (MR) (DSHS and DADS) components of HHSC. It contains MR Data (& MR History) along with MH Data (& History), including services provided in State Supported Living Centers (SSLCs). Also includes data for HCS, ICF/MR and TxHML programs. Mainframe MODEL 204 7 Home and Community Support Services Agencies 6 DADS MR CARE MR Client Assignment and Registration System 4 Database Type System Size (Gb, as of Jan 2014) Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 EDW Source Systems Future Scope System Count Agency Source System Name Source System Description 7 DADS SAS Service Authorization System Service Authorization System (SAS) accepts and maintains information about an individual’s authorization for services. State staff or a contracted provider authorizes specific service arrays for individual clients before a provider can successfully bill for services. An authorization provides service information such as: type of service, Level of Service (LOS), authorized service period (time frames), co-payment, and specific rates. Service Groups, Service Codes, and the authorized LOS drive system functionality, determining the programs and services for which an individual is authorized. DADS CMS Service Authorization System (SAS) database is the primary repository of service information for all individuals enrolled in DADS Long Term Care (LTC) programs. An electronic file of SAS data is transmitted to TMHP daily for claims adjudication processing. Oracle 8 DADS TxHML Texas Home Living This program provides selected essential services and supports to people with intellectual and developmental disabilities that live in their family homes or their own homes. Mainframe 5 Database Type System Size (Gb, as of Jan 2014) 220 7 Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 EDW Source Systems Future Scope System Count Agency Source System Name Source System Description 9 DARS TKIDS Texas Kids Intervention Data System Texas Kids Intervention Data System (TKIDS) is a consumer tracking system for Early Childhood Intervention (ECI). The system is used to collect data on services provided to children, birth to age 3 with disabilities or developmental delays, and their families. TKIDS also has a reporting application attached. Oracle 38 10 DFPS IMPACT Information Management Protecting Adults and Children in Texas IMPACT is a case management system that tracks Adult Protective Services (APS), Child Care Licensing (CCL) and Child Protective Services (CPS) program activities related to Reports of Abuse/Neglect, Investigations of Abuse/Neglect and Exploitation, delivery of services to clients including inhome services, foster care, eligibility determination, and billing. Oracle 1,126 6 Database Type System Size (Gb, as of Jan 2014) Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 System Count Agency 11 DSHS EDW Source Systems ASKIT Future Scope Source System Name Source System Description Automated System for Kidney Information Tracking Automated System for Kidney Health Information Tracking (ASKIT) provides patient and provider information for the Kidney Health Care Program (KHC) and their contracted providers. Checks client Medicaid information via both real-time and batch interfaces with the Centralized Billing System. Receives matching Medicare Part D data from U.S. Centers for Medicare and Medicaid Services (CMS); imports and exports files with contracted drug claims processor. 7 Database Type Sybase 5.3.2 System Size (Gb, as of Jan 2014) 25 Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 System Count Agency 12 DSHS EDW Source Systems CMBHS Future Scope Source System Name Source System Description Clinical Management for Behavioral Health Services Data Warehouse Clinical Management for Behavioral Health Services (CMBHS) is a web-based clinical record keeping system for statecontracted community mental health and substance abuse service providers. CMBHS is an electronic health record system that merges legacy automated health management systems from the former Texas Department of Mental Health and Mental Retardation (TDMHMR) and the former Texas Commission on Alcohol and Drug Abuse (TCADA). In addition to an electronic health record, CMBHS also serves as a clinical tool which includes diagnostic and treatment plan capabilities. CMBHS supports data exchange across contracted substance abuse service providers and between DSHS and other state agencies to coordinate care. The CMBHS system combines the electronic health recordkeeping requirements for both mental health and substance abuse treatment providers in a single system. 8 Database Type Oracle 10g System Size (Gb, as of Jan 2014) 328 Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 EDW Source Systems Future Scope System Count Agency Source System Name Source System Description 13 DSHS CMIS – CSHCN Case Management Information System – Children with Special Health Care Needs This system is used to determine and maintain client eligibility for the Children with Special Health Care Needs (CSHCN) program. Processes authorizations for services and payment of claims. Provides eligibility information to TMHP, TxDOT and the HHSCVendor Drug (VDP) Program’s contracted claims processor. Receives payment, provider, authorization, reconciliation and manifestation information from TMHP and the HHSC-Vendor Drug Program’s contracted claims processor. MS Access 2000 6 14 DSHS CPW Provider Children and Pregnant Women Provider Children & Pregnant Women (CPW) is a system that provides case management for children & pregnant women and where CPW providers complete and submit prior authorization requests for services. SQL SERVER 2008R2 1 15 DSHS CRS Client Record System Client Record System (CRS) is the primary client management system for State Supported Living Centers and Hospitals. It consists of admitting, discharge, transfer and billing functions as well as a full suite of electronic medical record modules for treatment planning, assessment, orders, dietary management, and incident tracking. Cache 16 DSHS IMD Institutions for Mental Diseases IMD MSIS Claims Processing. Medicaid claims documentation for state hospitals to be reported to HHSC MSIS System. Sybase ASE 12.5 9 Database Type System Size (Gb, as of Jan 2014) 250 1 Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 EDW Source Systems Future Scope System Count Agency Source System Name Source System Description 17 DSHS ImmTrac Texas Immunization Registry Texas Immunization Registry. ImmTrac is a central automated statewide immunization tracking registry that records immunizations administered to citizens in the State of Texas. Except for disaster-related information, consent must be obtained for records to be retained in the registry. SYBASE 15.0.3 71 18 DSHS NBS/LIMS Newborn Screening (NBS) / Laboratory Information Management System (LIMS) Newborn Screening (NBS) Laboratory Information Management System (LIMS) contains patient, provider & laboratory test results information for genetic & metabolic disease testing. – Microsoft SQL Server 2000 1,024 19 DSHS Orchard (Harvest) Harvest Harvest Laboratory operational information system for state hospitals contains patient information for the clinical chemistry portion of the laboratory. Tests include lead testing, hemoglobin red blood cell count, syphilis, glucose testing, cholesterol testing, and hemoglobinopathies Microsoft SQL Server 30 20 DSHS TER Texas Electronic Registrar Texas Electronic Registrar system tracks birth, death, and marriage certifications and customer service requests for vital records transactions. Oracle 11.0.2.3 266 21 DSHS THCIC Texas Health Care Information Council Health Care Data Collection System (HCDCS). Collection, auditing and warehousing of hospital discharge data and outpatient surgical and radiological procedure data. DSHS LINK 10 Database Type System Size (Gb, as of Jan 2014) Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 System Count Agency EDW Source Systems 22 DSHS THSteps 23 DSHS 24 25 Future Scope Source System Name Source System Description Database Type System Size (Gb, as of Jan 2014) Texas Health Steps Texas Health Steps (THSteps) is the Early Periodic Screening, Diagnosis, and Treatment (EPSDT) program for Texas Medicaid. THSteps provides preventive health care services at regular and periodic intervals to Medicaid clients who are from birth through 20 years of age. This system supports in part MMIS and is funded by Title XIX. SQL Server 2008, R2 85 TWICES Texas-Wide Integrated Client Encounter System Integrated case management across all DSHS program SQL SERVER 2008R2 50 HHSC ESSFDW(CAPPS Employee Data, HHSAS Financial Data) Enterprise Support Services Financial Data Warehouse Data Warehouse holds the CAPPS employees data and HHSAS Financial data for all HHS agencies Oracle 9.2.0 HHSC HEART HHS Enterprise Administrative Reporting and Tracking System –This system tracks external customer complaints, issues, and resolutions for compliance with SB 1563.‘ Sybase 11 102 Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 EDW Source Systems Future Scope System Count Agency Source System Name Source System Description 26 HHSC Medicare Buy-In Medicare BuyIn Medicare Buy-in system identifies and report individuals who are eligible for Medicare Buy-In to CMS. This would benefit individuals from saving a substantial amount of money on their income when they no longer pay for their Medicare premium. This also benefits the State when it buy-in an individual’s Medicare premium because Medicare will pay for their medical claims; therefore the State’s liability to pay Medicaid can be reduced. Oracle 95 27 HHSC MEHIS Medicaid Eligibility and Health Information Services The Medicaid Eligibility and Health Information System (MEHIS) replaced paper Medicaid identification forms with a permanent plastic card, automates eligibility verification, provides an electronic health record for all Medicaid clients, and establish a foundation for future health information exchange. Oracle 1,228 12 Database Type System Size (Gb, as of Jan 2014) Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 System Count Agency EDW Source Systems 28 HHSC NorthSTAR 29 HHSC NPPS Future Scope Source System Name Source System Description Database Type System Size (Gb, as of Jan 2014) NorthSTAR The NorthSTAR operational system provides for the identification and enrollment of consumers into the NorthSTAR behavioral managed care initiative. Custom developed Mainframe system. Interfaces with CARE and with Medicaid eligibility data. Sends enrollment and eligibility data to the enrollment broker (Maximus), to the NorthSTAR and Mental Retardation and Behavioral Health Outpatient Data Warehouse (MBOW) and to the managed care organization (Value Options). Mainframe 28 NorthSTAR Premium Payable System NPPS calculates provider payments and federal funds requests, and retains supporting client-level claim data for audit and reporting purposes. Oracle 100 13 Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 Future Scope EDW Future Scope: Potential Additional Data Sources The following Table 3 lists potential additional data sources currently considered relevant to potential future development and are provided to Respondents in order to provide information concerning the expected long term development strategy of the EDW. These potential additional data sources are outside the scope of this RFP. However, it is expected that the Solution should be able to be modified and enhanced to accommodate future objectives. This list includes reference data sources, data mapping/translation utilities, external system data (i.e. within Federal and commercial systems) and internal system data sources (i.e. additional HHS systems not previously integrated in earlier projects or listed above). Table 3 – Potential Additional Data Sources Purpose Name Category Provisioning Mode Stage Rationale External Data Automated Survey Processing Environment (ASPEN) Federal Data Client, Provider, and Enrollment Visibility Survey processing and data exchange between DADS and CMS (including deficiency plans for Medicaid providers). Internal Data Resiliency and Disease Management (RDM) State – DSHS Data Client, Provider, and Enrollment Visibility A primary aim of RDM is to ensure the provision of interventions with empirical support to eliminate or manage symptoms and promote recovery from psychiatric disorders Internal Data Supplemental Nutrition Assistance Program (SNAP) State – HHSC Data Client, Provider, and Enrollment Visibility Provides additional program information for Medicaid clients eligible for SNAP Internal Data Service Utilization and Review System (SURS) State - OIG Data Client, Provider, and Enrollment Visibility Utilization review of Medicaid providers by the HHSC Office of the Inspector General Internal Data Temporary Assistance for Needy Families (TANF) State – HHSC Data Client, Provider, and Provides additional program information for Medicaid clients 14 Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 Purpose Name Future Scope Category Provisioning Mode Stage Rationale Enrollment Visibility eligible for TANF Reference Case Management CrossReference State – Custom (BM) Data Client, Provider, and Enrollment Visibility Provides maintained descriptions and program attribution for all HHS case management programs. Reference Functional Assessment Codes and Descriptions State Data Client, Provider, and Enrollment Visibility Reference data for functional, medical, or psychiatric assessments across the enterprise. Internal / External Data Provider Structure with Employees Solution Data Client, Provider, and Enrollment Visibility Required for functions relating to provider facilities. Provider businessto-business and organization/group ownership information does not reside (or is incompletely described) in HHS systems. Reference Service Authorization Codes and Descriptions State Data Client, Provider, and Enrollment Visibility Reference data for authorizations across the HHS enterprise. External Data Outcome and Assessment Information Set (OASIS) Federal Data Service Delivery LTC assessment and incident data shared between Federal system and CARES. Reference Public Assistance Reporting Information System (PARIS) Federal Data Service Delivery Current use is within DADS to identify military veterans who are in both VA and Texas Medicaid 15 Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 Purpose Name Future Scope Category Provisioning Mode Stage Rationale systems. Reference Systematized Nomenclature of Medicine (SNOMED) (D Axis) Codes and Descriptions Solution Data Service Delivery Universal reference set expected to describe many healthcare service transactions available in the future via HIE. Not currently used in HHSC services or payment systems. External Data Prescription Drug Point-of-Sale Data Solution Data Drug Integration Point-of-sale data to supplement prescription data in Vendor Drug system. Internal Data Insurance Third Party Payer Data State Data Client Historical Information Existing third party payer information in Compass21 (TPR, etc.) External Data Insurance Brokerage Data Solution Data Client Historical Information Source(s) needed to supplement payer or coverage histories for Medicaid clients. Link HIX State Data Client Historical Information Source(s) needed to supplement payer or coverage histories for Medicaid clients. Internal Data DSHS Nutrition, Physical Activity, and Obesity Prevention (NPAOP) State Data Client Historical Information Program information and data for a DSHS program known to impact Medicaid clients Internal Data DSHS Tobacco Prevention and Control (TPC) State Data Client Historical Information Program information and data for a DSHS program known to impact Medicaid clients If the required data is not yet available in the EDW, the EDW may potentially be required to acquire the necessary data 16 Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 Purpose Name Future Scope Category Provisioning Mode Stage Rationale from sources specified by HHSC-OIG (current list of MFADS sources is listed below) for online inquiry access to these data via universes to be built by HHSC-OIG within the MFADS sandbox of the EDW. Internal Data HHSC Medicaid Claims Administrator Contractor Adjudicated acute care claims, adjudicated Medicare crossover claims, encounters, and code tables State Data MFADS Currently used by MFADS program. State Data MFADS Currently used by MFADS program. State – HHSC Data MFADS Currently used by MFADS program. Provider File – provider identification data and code tables Reference Files – To include but not limited to Diagnosis Related Group, Diagnosis Code, Procedure Codes, and code tables Client File – Client eligibility data and code tables (data originates from HHSC SAVERR or HHSC TIERS systems) HHSC Eligibility Recon Extract – Client eligibility reconciliation extract Adjudicated Claims data and code tables Provider/Vendor/contract data and code tables Reference files and code tables Internal Data HHSC Vendor Drug Claims Processing Contractor Adjudicated Claims data and code tables Reference data to include pharmacy, pharmacy address, pharmacy type, National Drug Code (NDC), and lock-in Internal Data HHSC Medical Transportation (provides non-emergency transportation services) Authorization data 17 Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 Purpose Internal Data Name DADS Long Term Care (LTC)/Claims Management System (CMS) LTC adjudicated claims data and code tables Future Scope Category Provisioning Mode Stage Rationale State Data MFADS Currently used by MFADS program. LTC authorizations data and code tables LTC facility assessment data and code tables LTC provider data from the LTC Provider Subsystem LTC facility data from the Long Term Care Regulatory Client Assessment Resident Evaluation System (CARES) which contains facility demographic, ownership, licensure, and certification, sanctions, and other similar data Internal Data HHSC SAVERR/TIERS Eligibility Recon Eligibility Recon Extract – Client eligibility reconsiderations extract State Data MFADS Currently used by MFADS program. Internal Data HHSC/DSHS Texas Health Steps (THSteps) THSteps medical screening laboratory data and code tables State Data MFADS Currently used by MFADS program. THSteps newborn screening data and code table Internal Data DSHS Bureau of Vital Statistics (BVS) BVS deaths data and code tables State Data MFADS Currently used by MFADS program. Internal / External Data Texas State Licensing Board (external data – currently obtained by MFADS from HHSC Medicaid Claims Administrator Contractor) Dental provider licensing data and code tables State Data MFADS Currently used by MFADS program. Medical Doctor/Doctor of Osteopathic Medicine (MD/DO) provider licensing 18 Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 Purpose Name Future Scope Category Provisioning Mode Stage Rationale data and code tables Board of Nurse Examiners Registered Nurse (RN) licensing data Board of Nurse Examiners Licensed Vocational Nurse (LVN) licensing data Board of Nurse Examiners Advanced Practice Registered Nurse (APRN) licensing data External Data SSA Death Master File – obtained via subscription, monthly download accessible through Social Security Death Master File Monthly Download Service (External Web Site) Federal Data MFADS Currently used by MFADS program. Definitions Purpose: Classification of data sources (Acquisition, Collections, Conformance, External Data, Identity, Internal Data, Link, Mapping, Reference, Translation) Category: Proposed method by which the reference data will be provisioned or generated when required in the future. Solution – Contractor’s Solution will incorporate The potential additional data source when required in the future through the EDW Change Order process. Federal, State, Other – HHSC will be responsible for subscription of the additional data sources that the Contractor will include in the Solution’s data acquisition, when required in the future through the EDW Change Order process. Provisioning Mode: Potential or expected format of data source (Data, Software) 19 Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 Future Scope EDW Future Scope: Potential Additional Services or Software for Data Connectivity The following Table 4 lists potential additional services or software for data connectivity requirement, currently considered relevant to potential future development and are provided to Respondents in order to provide information concerning the expected long term development strategy of the EDW. These potential additional services or software requirements are outside the scope of this RFP. However, it is expected that the Solution should be able to be modified and enhanced to accommodate future objectives. Table 4 – Additional Services or Software for Data Connectivity Purpose Name Category Provisioning Mode Stage Rationale Reference Dartmouth Atlas Solution Data/Software Service Delivery Medicare utilization measurement and reference via geographic regions for comparative benchmarking Mapping Drugs to Diagnosis [External] Solution Data/Software Drug Integration Required to relate diagnosis events available in HIE or other external systems within episodes of care. Mapping Drugs to Procedure [External] Solution Data/Software Drug Integration Required to relate diagnosis events available in HIE or other external systems within episodes of care. Acquisition Electronic Medical Records (EMR) Parser Solution Software Client Historical Information Needed to integrate transaction data from future HIE system(s) Link HIE Solution Data/Software Client Historical Information Needed to integrate transaction data from future HIE system(s) Mapping Alignment of I Data Elements Solution Software Client Historical Information Needed to integrate transaction data from future HIE system(s) Definitions Purpose: Classification of data sources (Acquisition, Collections, Conformance, External Data, Identity, Internal Data, Link, Mapping, Reference, Translation) 20 Texas Health and Human Services Commission EDW/BI Solution RFP No. 529-16-0001 Purpose Name Category Future Scope Provisioning Mode Stage Rationale Category: Proposed method by which the reference data will be provisioned or generated when required in the future. Solution – Contractor’s Solution will incorporate the potential additional services or software when required in the future through the EDW Change Order process. Provisioning Mode: Potential or expected format of data source (Data, Software) 21 Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 Future Scope Appendix A – Detailed Functional Requirements – Potential Future Scope FR ID FR015 Functional Requirement: Use Vital Statistics to notify business units of client life changes. Stage: Client, Provider, and Enrollment Visibility Description: This requires integrations to vital statistics records at DSHS or other external governmental entity records that track births, deaths or other major life changes. The intent is to pass data concerning these changes to the EDW to enable early identification of changes that may impact client eligibility for services. Potential User Groups: DADS Budget Analysts MH Inpatient Services DSHS Center for Health Statistics THSteps LTC Analysts HHSC Operations Support (Managed Care) People who need clean addresses for mailings MITA Business Processes: Determine Eligibility Disenroll Member Enroll Member Inquire Member Eligibility Manage Member Information Member Management (ME) Member Management (ME) Member Management (ME) Member Management (ME) Member Management (ME) FR ID FR076 Functional Requirement: Implement enterprise view across agencies of case management portfolio. Stage: Client, Provider, and Enrollment Visibility Description: The EDW will enable users to view the array of services available clients in the various programs funded by Medicaid. Potential User Groups: Strategic Decision Support DADS Budget Analysts MITA Business Processes: Develop and Maintain Benefits Package Develop and Maintain Program Policy Manage Program Information Manage Case 22 Program Management (PG) Program Management (PG) Program Management (PG) Program Integrity Management (PI) Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 Future Scope FR ID FR041 Functional Requirement: Expose streams of care episodes that cross programs or departments or agencies Stage: Service Delivery (Episodes of Care) Description: The Vendor will be able to identify episodes of care that involve more than one program, department or agency. For instance, if a long term care client receives acute care services. This requires Episodes of Care. Potential User Groups: Office of the Medical Director HHSC Operations Support (Managed Care) LTC Analysts Strategic Decision Support DADS Budget Analysts TMHP Vendor Drug Program MITA Business Processes: Manage Member Information Generate Financial and Program Analysis Manage Program Information Perform Population and Member Outreach Develop and Maintain Program Policy Establish Case Manage Medicaid Population Health Manage Registry Member Management (ME) Program Management (PG) Program Management (PG) Member Management (ME) Program Management (PG) Care Management (CM) Care Management (CM) Care Management (CM) FR ID FR003 Functional Requirement: Determine availability in comparable programs (Medicaid) Stage: Client, Provider, and Enrollment Visibility Description: Comparable programs are those programs with similar eligibility requirements and service offerings. This requirement supports analysis of comparable programs from several perspectives. This analysis may support case management activities by identifying comparable programs with interest lists or available openings for new clients. The requirements also support examination of any differences in access and utilization to determine causes and/or approaches to optimize service delivery. Potential User Groups: DADS Budget Analysts Strategic Decision Support THSteps LTC Analysts HHSC Operations Support (Managed Care) DFPS Analysts MITA Business Processes: Manage Program Information Maintain Benefits-Reference Information 23 Program Management (PG) Program Management (PG) Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 Future Scope FR ID FR006 Functional Requirement: Monitor cost impact of migration between programs and services (including both internal and external as available) Stage: Service Delivery (Episodes of Care) Description: Clients may move from one program or service to another throughout their tenure in HHS services. This migration makes it difficult to provide continuity of care to Medicaid clients and may lead to increased health risks. Further, frequent movement may add to the cost of client services. EDW will be able to track these movements and the costs associated with the move (i.e., costs for services in program A versus cost in program B). The EDW will support analysis of reasons for frequent migration, services authorized and received through each program and the costs for the service. Potential User Groups: HHSC Operations Support (Managed Care) DADS Budget Analysts Strategic Decision Support System Forecasting LTC Analysts HHSC Actuarial Analysis HHSC Rate Analysts Vendor Drug Program Office of the Medical Director MITA Business Processes: Disenroll Member Enroll Member Authorize Referral Authorize Service Price Claim-Value Encounter Prepare Capitation Premium Payments Member Management (ME) Member Management (ME) Operations Management (OM) Operations Management (OM) Operations Management (OM) Operations Management (OM) FR ID FR021 Functional Requirement: Integrate service data from the All Payers database (THCIC). Stage: Service Delivery (Episodes of Care) Description: DSHS manages the Health Care Information Council and its All Payers database. The Vendor will identify tables and elements from the All Payers database and include these into episodes in the EDW. This specifically includes items such as hospital discharge data, including present-on-admission indicators. Potential User Groups: DSHS Center for Health Statistics Office of the Medical Director MITA Business Processes: Price Claim-Value Encounter Operations Management (OM) 24 Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 Future Scope Prepare Home and Community Based Services Payment Operations Management (OM) FR ID FR043 Functional Requirement: Assess comparable services within and across all agencies Stage: Service Delivery (Episodes of Care) Description: In the current environment, there is little visibility from program to program, particularly when these programs are managed by separate agencies. The EDW will support the ability to identify programs that are comparable, both within an agency and across the enterprise of five separate agencies. This functionality gives the HHS enterprise the ability to compare programs to identify unnecessary duplication of services, exam disparity in reimbursement rates and make appropriate referrals for clients. This requires Episodes of Care. Potential User Groups: Office of the Medical Director Strategic Decision Support DADS Budget Analysts LTC Analysts DSHS Center for Health Statistics ECI Analysts HHSC Operations Support (Managed Care) Vendor Drug Program TMHP MH Inpatient Services THSteps MITA Business Processes: Develop and Maintain Benefits Package Develop and Maintain Program Policy Manage Program Information Program Management (PG) Program Management (PG) Program Management (PG) FR ID FR061 Functional Requirement: Provide a single view of Medicaid services across programs/agencies. Stage: Service Delivery (Episodes of Care) Description: This functionality requires access to claim, encounter and provider data necessary to track all of the programs and HHS agencies that provide a particular service. For each agency or program, the EDW will be able to aggregate all services provided to create a comprehensive view of all services within the agency or program. This requires Episodes of Care. Potential User Groups: Strategic Decision Support 25 Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 Future Scope DADS Budget Analysts System Forecasting LTC Analysts HHSC Rate Analysts HHSC Actuarial Analysis HHSC Operations Support (Managed Care) Vendor Drug Program Office of the Medical Director THSteps MH Inpatient Services DFPS Analysts MITA Business Processes: Manage Member Information Manage Provider Information Price Claim-Value Encounter Prepare Capitation Premium Payments Prepare Home and Community Based Services Payment Member Management (ME) Provider Management (PM) Operations Management (OM) Operations Management (OM) Operations Management (OM) FR ID FR067b Functional Requirement: Integrate health data from private insurers Stage: Client Historical Information Description: HHS agencies have some data related to private insurance coverage for Medicaid clients. External sources of coverage and treatment data (e.g. HIX, HIE, insurance and claims clearinghouses) can be integrated to provide more complete data regarding continuity of care and continuity of coverage for periods when clients were outside Medicaid. Potential User Groups: DADS Budget Analysts System Forecasting Strategic Decision Support TMHP THSteps LTC Analysts HHSC Operations Support (Managed Care) Office of the Medical Director DFPS Analysts ECI Analysts MITA Business Processes: Manage Member Information Establish Business Relationship Manage Business Relationship 26 Member Management (ME) Business Relationship Management (BR) Business Relationship Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 Future Scope Management (BR) FR ID FR068 Functional Requirement: Integrate data about veterans who are also clients from the VA Stage: Client Historical Information Description: A new interface will need to be built to bring in data from external systems (such as PARIS) with the VA for sharing data related to individuals who receive both VA and HHS services. The VA data will be integrated to the EDW to enable identification of clients receiving both types of service and improve coordination of services. Potential User Groups: System Forecasting Strategic Decision Support DADS Budget Analysts LTC Analysts HHSC Operations Support (Managed Care) Office of the Medical Director MITA Business Processes: Manage Member Information Establish Business Relationship Manage Business Relationship Member Management (ME) Business Relationship Management (BR) Business Relationship Management (BR) FR ID FR018 Functional Requirement: Integrate DSHS registries with client records. Stage: Client, Provider, and Enrollment Visibility Description: DSHS maintains several public health registries (i.e., cancer registry). Integration of registry data with the EDW will enable identification of public health trends in the Medicaid client population and ensure more accurate reporting of Medicaid client status to the appropriate registry. Potential User Groups: DSHS Center for Health Statistics Office of the Medical Director LTC Analysts MITA Business Processes: Determine Eligibility Inquire Member Eligibility Manage Member Information Member Management (ME) Member Management (ME) Member Management (ME) 27 Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 Future Scope FR ID FR020 Functional Requirement: Incorporate public health strategy program data, e.g., immunizations, smoking Stage: Service Delivery (Episodes of Care) Description: The Vendor shall integrate to source systems that track public health strategies such as the immunization tracking system. The intent is to ensure that both the public health strategy programs and the EDW contain current, accurate information for Potential User Groups: DSHS Center for Health Statistics Office of the Medical Director MITA Business Processes: Develop Agency Goals and Objectives Develop and Maintain Program Policy Manage Member Information Perform Population and Member Outreach Program Management (PG) Program Management (PG) Member Management (ME) Member Management (ME) FR ID FR066 Functional Requirement: Integrate Vendor drug by incorporating drugs prescribed through private insurance providers. Stage: Client Historical Information Description: The Vendor will integrate with subscription services that provide visibility to drug prescribed through private insurance. This will provide a complete view into a cli’nt's drug history. This will require Episodes of Care. Potential User Groups: Vendor Drug Program MH Inpatient Services Office of the Medical Director MEHIS Analysts MITA Business Processes: Manage Member Information Authorize Service Member Management (ME) Operations Management (OM) FR ID FR028 Functional Requirement: Identify people without health insurance. Stage: Client Historical Information Description: This functionality requires integrate to HIXs and is a future requirement. The intent is to obtain prior health insurance coverage spans through HIXs and/or insurance brokerage subscription data once these are implemented state-wide. Potential User Groups: Office of the Medical Director System Forecasting 28 Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 Future Scope MITA Business Processes: Perform Population and Member Outreach Member Management (ME) FR ID FR078 Functional Requirement: Compare client outcomes across case management programs. Stage: Client Historical Information Description: HHS agencies need to be able to assess the efficacy and effectiveness of case management programs. As outcomes for comprehensive case management is identified and tracked, the EDW will include outcome data to support this analysis. This requires Episodes of Care. Potential User Groups: LTC Analysts HHSC Operations Support (Managed Care) Office of the Medical Director Strategic Decision Support MITA Business Processes: Develop and Maintain Benefits Package Develop and Maintain Program Policy Manage Program Information Manage Case Manage Member Information Inquire Member Eligibility 29 Program Management (PG) Program Management (PG) Program Management (PG) Program Integrity Management (PI) Member Management (ME) Member Management (ME) Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 Future Scope Appendix B – Glossary for Additional Future Scope Acronyms and Terms The following Table 5 lists the additional expansion of Acronyms within this Future Scope document that is not previously provided in Exhibit A – Glossary document of the Procurement Library. Table 5 - Additional Acronyms Acronym Expansion APRN Advanced Practice Registered Nurse APS Adult Protective Services ASKIT Automated System for Kidney Health Information Tracking ASPEN Automated Survey Processing Equipment BR Medicaid Information Technology Architecture acronym for Business Relationship Management Business Process BVS Bureau of Vital Statistics CARE Client Assignment and Registration System CARES Compliance, Assessment, Reporting, and Enforcement System CCL Child Care Licensing CM Medicaid Information Technology Architecture acronym for Care Management Business Process CMBHS Clinical Management for Behavioral Health Services Data Warehouse CMIS Case Management Information System CPS Child Protective Services CPW Children and Pregnant Women CRS Client Record System CSHCN Children with Special Health Care Needs CSIL Community Services Interest List DADS Texas Department of Aging and Disability Services DARS Texas Department of Assistive and Rehabilitative Services DFPS Texas Department of Family and Protective Services DO Doctor of Osteopathic Medicine DSHS Texas Department of State Health Services ECI Early Childhood Intervention EHR Electronic Health Records 30 Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 Future Scope Acronym Expansion EMR Electronic Medical Records EPSDT Early Periodic Screening, Diagnosis, and Treatment HCDCS Health Care Data Collection System HCS Home and Community-based Services HCSSA Home and Community Support Services Agencies HEART HHS Enterprise Administrative Reporting and Tracking System HHSAS Health and Human Services Accounting System HIE Health Information Exchange HIT Health Information Technology HIX Health Insurance Exchange ICF-MR or Intermediate Care Facilities for Persons with Mental Retardation ICF/MR IMD Institutions for Mental Diseases ImmTrac Texas Immunization Registry IMPACT Information Management Protecting Adults and Children in Texas KHC Kidney Health Care Program LIMS Laboratory Information Management System LOS Level of Service LVN Licensed Vocational Nurse MARs Medication Administration Records MBOW Mental Retardation and Behavioral Health Outpatient Data Warehouse MD Medical Doctor ME Medicaid Information Technology Architecture acronym for Member Management Business Process MEHIS Texas Medicaid Eligibility and Health Information Services MH Mental Health MR Mental Retardation MR CARE Mental Retardation Client Assignment and Registration System MSIS Medicaid Statistical Information System NBS Newborn Screening 31 Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 Future Scope Acronym Expansion NDC National Drug Code NPOAP Nutrition, Physical Activity, and Obesity Prevent NPPS NorthSTAR Premium Payment System OASIS Outcome and Assessment Information Set OM Medicaid Information Technology Architecture acronym for Operations Management Business Process PARIS Public Assistance Reporting Information System PG Medicaid Information Technology Architecture acronym for Program Management Business Process PM Medicaid Information Technology Architecture acronym for Provider Management Business Process PRV PMT Provider Payment RDM Resiliency and Disease Management RN Registered Nurse SAS Service Authorization System SAVERR System of Application, Verification, Eligibility, Referral and Reporting SNOMED Systematized Nomenclature of Medicine SSLCs State Supported Living Centers SURS Service Utilization Review System TCADA Texas Commission on Alcohol and Drug Abuse TDMHMR Texas Department of Mental Health and Mental Retardation TER Texas Electronic Registrar THCIC Texas Health Care Information Collection THSteps Texas Health Steps TKIDS Texas Kids Intervention Data System TPC Tobacco Prevention and Control TWICES Texas Wide Integrated Client Encounter System TxDOT Texas Department of Transportation TxHML Texas Home Living VDP Vendor Drug Program 32 Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 Future Scope The following Table 6 lists the additional brief definition of Terms within this Future Scope document that is not previously provided in Exhibit A – Glossary document of the Procurement Library. Table 6 - Additional Term Definitions Term Brief Definition Dartmouth Atlas Refers to the Dartmouth Atlas of Health Care organization that provides benchmark for geographic mapping of how medical resources are distributed and used in the United States, assisting policymakers, the media, health care analysts and others improve their understanding of health care systems. Electronic Health Records (EHR) Means a collection of electronic health information about an individual patient. It is a record in digital format that is theoretically capable of being shared across different health care settings. Electronic Medical Record (EMR) Means a computerized medical record created in an organization that delivers care, such as a hospital or physician's office. Electronic medical records tend to be a part of a local stand-alone health information system that allows storage, retrieval and modification of records. Health Information Exchange (HIE) Means the mobilization of healthcare information electronically across organizations within a region, community or hospital system. Health Information Technology (HIT) Means the umbrella framework to describe the comprehensive management of health information across computerized systems and its secure exchange between consumers, providers, government and quality entities, and insurers. Health Insurance Exchange (HIX) Means the set of state-regulated and standardized health care plans in the United States, from which individuals may purchase health insurance eligible for federal subsidies. Medicaid Eligibility and Health Information Services (MEHIS) Refers to the application system that positions HHSC to respond to the emerging and anticipated health information technology initiatives that will foster improved continuity of care, increased communication with clients and providers, expanded data for healthcare analytics, and better health outcomes over time. Medicaid Statistical Information System (MSIS) Prior to Federal fiscal year 1999, the Medical Statistical Information System (MSIS) were a voluntary program and those states participating in the MSIS project provided data tapes from their claims processing systems to the Centers for Medicare & Medicaid Services (CMS) in lieu of the hard-copy statistical 2082 tables. However, in accordance with the Balanced Budget Act (BBA) of 1997, all claims processed are submitted electronically through MSIS. 33 Texas Health and Human Services Commission EDW/BI Solution - RFP No. 529-16-0001 Future Scope Term Brief Definition Supplemental Nutrition Assistance Program (SNAP) Means the program that provides financial assistance for food purchasing to low- and no-income people and families in Texas. Temporary Assistance for Needy Families (TANF) Means the federal assistance program administered by HHSC that provides temporary assistance for needy families in Texas. 34