Lap LAR - JGA
advertisement
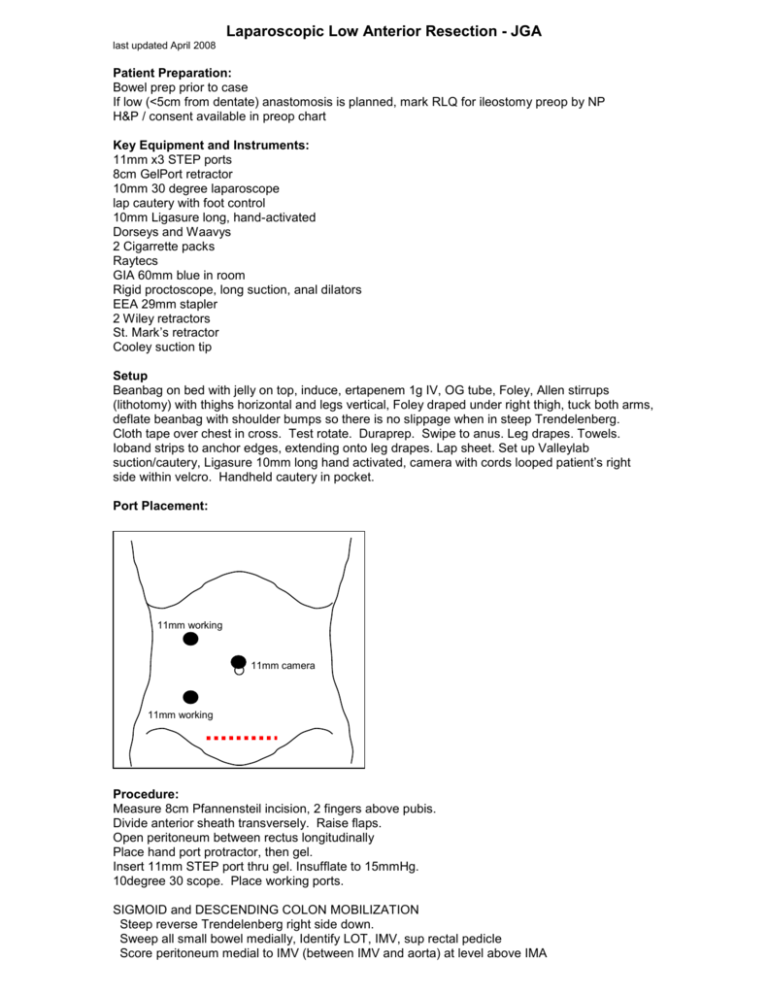
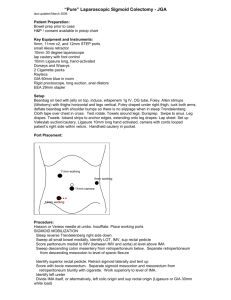
Laparoscopic Low Anterior Resection - JGA last updated April 2008 Patient Preparation: Bowel prep prior to case If low (<5cm from dentate) anastomosis is planned, mark RLQ for ileostomy preop by NP H&P / consent available in preop chart Key Equipment and Instruments: 11mm x3 STEP ports 8cm GelPort retractor 10mm 30 degree laparoscope lap cautery with foot control 10mm Ligasure long, hand-activated Dorseys and Waavys 2 Cigarrette packs Raytecs GIA 60mm blue in room Rigid proctoscope, long suction, anal dilators EEA 29mm stapler 2 Wiley retractors St. Mark’s retractor Cooley suction tip Setup Beanbag on bed with jelly on top, induce, ertapenem 1g IV, OG tube, Foley, Allen stirrups (lithotomy) with thighs horizontal and legs vertical, Foley draped under right thigh, tuck both arms, deflate beanbag with shoulder bumps so there is no slippage when in steep Trendelenberg. Cloth tape over chest in cross. Test rotate. Duraprep. Swipe to anus. Leg drapes. Towels. Ioband strips to anchor edges, extending onto leg drapes. Lap sheet. Set up Valleylab suction/cautery, Ligasure 10mm long hand activated, camera with cords looped patient’s right side within velcro. Handheld cautery in pocket. Port Placement: 11mm working 11mm camera 11mm working Procedure: Measure 8cm Pfannensteil incision, 2 fingers above pubis. Divide anterior sheath transversely. Raise flaps. Open peritoneum between rectus longitudinally Place hand port protractor, then gel. Insert 11mm STEP port thru gel. Insufflate to 15mmHg. 10degree 30 scope. Place working ports. SIGMOID and DESCENDING COLON MOBILIZATION Steep reverse Trendelenberg right side down. Sweep all small bowel medially, Identify LOT, IMV, sup rectal pedicle Score peritoneum medial to IMV (between IMV and aorta) at level above IMA Sweep descending colon mesentery from retroperitoneum below. Separate retroperitoneum from descending mesocolon to level of splenic flexure Identify superior rectal pedicle. Retract sigmoid laterally and tent up with hand Score with bovie mesorectum. Separate sigmoid mesocolon and mesorectum from retroperitoneum bluntly. Work superiorly to level of IMA. Identify left ureter Divide IMA itself, or altermatively, left colic origin and sup rectal origin (Ligasure or GIA 30mm white load) Divide descending mesocolon, including left colic vein and IMV, to level of LOT. Preserve marginal artery. Retract sigmoid medially and divide lateral attachments with bovie or metzembaum scissors, completely mobilizing sigmoid colon. SPLENIC FLEXURE TAKEDOWN Retract descending colon medially, and bovie lateral attachments. Reposition. Patient head up. Flip omentum towards head and open lesser sac from right to left with bovie / ligasure. Take down splenic flexure right to left. Omentum stays with stomach. In some cases, JGA will take down flexure left to right if the patient’s torso is not too long and JGA’s tennis elbow is not acting up. Continue onto transverse colon and COMPLETELY separate gastrocolic with bovie to about the falciform (i.e. midline). Divide mesocolon to level of LOT (close to left branch of middle colic) Lap portion of case complete. RECTAL DISSECTION Clean fat off planned resection line with bovie. Divide proximal sigmoid ensuring enough length to reach pelvis is present. Divide colon with GIA 60 blue. Divide marginal vessels with Ligasure. Pack descending colon and small intestines superiorly, exposing rectum. Perform rectal dissection. Develop plane posteriorly and use it to guide you anteriorly. Tricks: St. Mark’s to retract rectum anteriorly and develop posterior space Wiley’s (renal vein retractors) to retract sidewalls and bladder flap Cooley sucker tip is long enough to retract deep in pelvis Sponge sticks also help provide lateral retraction. Once below tumor and at level of levators, divide rectum with TA 30 blue or green (depending on thickness) Open specimen on back table. PREPARE DESCENDING COLON Use soft bowel clamp to clamp distal colon Cut colon 2-0 prolene double armed pursestring. Place EEA 29 anvil (black stapler). Tie pursetring. Leave one needle on initially Clean off fat. If diverticulum within staple line, use suture to tuck in. Dunk colon into abdomen Use Alexis and clamp off with a peon to maintain pneumoperitoneum MAKE ANASTOMOSIS Surgeon goes between legs. Dilate anus to 31mm EEA 29mm. Trocar should pass just anterior to staple line. If low anastomosis, make sure vagina/bladder out of stapler. (on black stapler, only ½ twist needed after firing to release. On white stapler, 2 full rotations needed) Submerge anastomosis in saline. Insert rigid proctoscope. Insufflate and look for air leak. Inspect suture line Inspect donuts Leave #19 round Blake drain in pelvis if dissection was below peritoneal reflections. OTW none. If very low anastomosis or tension -> consider diverting loop ileostomy CLOSE No peritoneal closure #1 maxon running for anterior sheath No fascial closure for port sites 3-0 dexon scarpas 4-0 biosyn running skin Indermil only Postoperative Care: Heparin SQ in am POD1 after surgery ADAT when passing flatus