WBC Hematology - Leukemia
advertisement

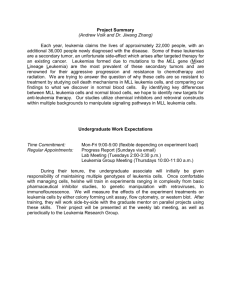
©2009 Mark Tuttle Leukemia Name Mutation Acute Lymphoblastic - L1: Small blasts (Tdt+) Leukemia - L2: Large blasts (Tdt+) (ALL) - L3: Peripheral B, Burkitt leukemia/lymphoma o Tdt negative Children <15 yrs o Multiple vacuoles o t(8;14), t(2;8), t(8;22), always 8 c-myc oncogene Symptoms/Labs - More than 20% blasts in marrow - Lymphadenopathy - CNS involvement (meningeal signs, headache, vomiting) more common in ALL than AML - t(9:22) has worse prognosis than in CML Histology Treatment - Acute Myelogenous Leukemia (AML) - More than 20% blasts in marrow - Neutropenia: bact infections, fever - Anemia - Thrombocytopenia: bleeding, petechiae, epistaxis - Maybe hepatosplenomegaly, lymphadenopathy(in ALL) - Bone pain - Can be asymptomatic - Auer rods clumps of azurophilic granular materia - 15-20% cure rate 15-40 year olds Myelodysplastic Syndrome - M0: stem cells - M1: w/o maturation, >90% blasts - M2: with maturation, 20-90% blasts o t(8;21) or t(16;16) CFB blocks differentiation - M3: acute promyolocytic leukemia APL, Auer rods ↑ o t(15;17) PML blocks differentiation o Treat with ATRA to promote differentiation o Severe DIC due to dying PMN granules - M4eo: eosinophils o t(16;16) same PML mutation as M2 - M4/5: Acute monocytic leukemia o t(11q23;v) same PML mutation as M2 - M6: Erythroleukemia - M7: Megakaryocytic o Myelofibrosis common o Increased in kids w/down syndrome - Commonly deletions - Less than 20% blasts “pre- Pseudo Perger-Huet leukemia” neutrophils (2 nuclear lobes) - 2-8 years post radiation or chemo is common scenario] - Also can be idiopathic - Ringed Sideroblasts - 1/3 die from unrelated - 1/3 die from MDS complications - 1/3 die from progression to AML - 1-3 yr prognosis Name Chronic Myeloblastic Leukemia (CML) Polycythemia vera Essential Thrombocytosis Primary Myelofibrosis Chronic Lymphocytic Leukemia (CLL) / Small lymphocytic leukemia (SLL) The most common leukemia in adults Hairy Cell Leukemia (HCL) Multiple Myeloma Waldenstrom’s Macroglobulinemia Mutation Symptoms/Labs - t(9;22) Philly chromosome in - Hypercellular marrow 100% of cases - WBC > 50,000 - Basophils ↑, >20% in accelerated phase - Massive splenomegaly - LAP low (High in leukemoid rxn) - Can be very high platelets - Can transform to acute leukemia (blast crisis) (2/3 transform to AML, 1/3 transform to ALL) - Jak2 mutation in 95% - Increased RBC mass, high Hb & Hct - Low or undetectable EPO - Need to rule out CO poisoning - Increased blood viscosity - Bleeding + thromboses with infarctions, DVD, strokes, Budd-Chiari - Transforms to myeolfibrosis frequently with massive splenomegaly - Jak2 in 50% - Bleeding & thromboses - MPL in 10% - Erythromelalgia (throbbing burning in hands & feet) (Myeloproliferative - Splenomegaly leukemia gene) works with thrombopoitin gene - Marrow fibrosis due to megakaryocytes cytokines - Extramedullary hematopoisis - Massive splenomegaly - Immature myeloid cells in blood - Dx by flow cytometry - Nonspecific or asymptomatic - CD5+, CD10-, CD23+ - Generalized lymphadenopathy frequent - High WBC, absolute lyphocytosis - Coombs+ hemolytic anemia = spherocytes - Transform to prolymphocytic leukemia (in blood) or large cell lymphoma (Richter syndrome in lymph node) - Dx by flow cytometry - Triad: Older male, massive splenomegaly, pancytopenia - Bone marrow dry tap - TRAP+ cells - IL-6 driven proliferation Bone resorption - Usually IgG (not filtered by kidney, no kidney problems) - Need >10% Plasma cells in marrow or is MGUS (uncertain signif) - Hypercalcemia - Bence-Jones proteinuria - Can get primary amyloidosis if chains depositing in organs - IgM always kidney problems - No bone lesions - Lymphadenopathy, Reynaud’s phenomenon, Hyperviscosity Histology - Teardrop RBCs Treatment ©2009 M.T. - Gleevac (imatinib) targets abnormal tyrosine kinase - - - Giant platelets - - Teardrop RBCs - - Smudge cells - - Fuzzy cytoplasm - - Blood rouleaux - Poor prognosis - -