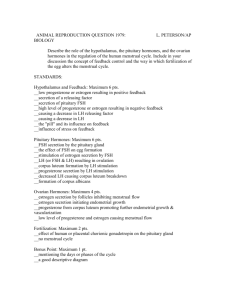
HPO Axis
advertisement
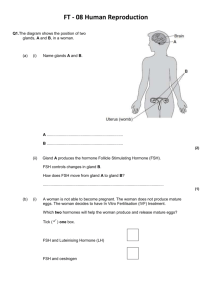
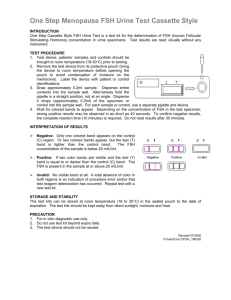
Hormones are involved in the control of all of these processes by a complex interaction between different controlling structures known as the The Hypothalamus – Pituitary – Gonadal Axis. In both male and female the major controlling structures are located in the brain (the hypothalamus), the pituitary gland, (particularly the anterior pituitary), and the gonads. In the pregnant female important control is also exerted by the placenta. Each structure interacts with the others primarily by secretion of hormones. The Pituitary Gland The anterior pituitary gland is not nervous tissues. It arises embryologically from Rathke’s Pouch. It has a number of cell types secreting different hormones, most of which are involved in, or affected by reproduction. Many pituitary hormones are trophic hormones, which act on other endocrine tissues to promote the secretion of further hormones. Hypothalamus and Pituitary Each secretory cell type in the anterior pituitary is controlled by releasing hormones, produced by nerve cells in the hypothalamus, which pass to the anterior pituitary in the Hypophyseal portal system . The main reproductive anterior pituitary hormones, the gonadotrophins, FSH ( follicle stimulating hormone) and LH( luteinising hormone) are produced by one cell type – the gonadotrophs, and controlled by one releasing hormone – Gonadotrophin Releasing Hormone (GnRH). Several groups of hypothalamic neurones secrete GnRH under the influence both of other structures in the brain (and hence the environment via sensory input) and circulating hormones. All secrete GnRH in a pulsatile fashion – a burst of secretion about once an hour. Gonadotrophs in the anterior pituitary secrete gonadotrophins in response to these pulses of GnRH. In the absence of GnRH no LH or FSH is secreted. FSH and LH act primarily on the gonads to influence the production of gametes and to promote the secretion of gonadal steroids – oestradiol and progesterone in the female and testosterone in the male. In the absence of LH and FSH no gonadal steroids are secreted. Control of the hypothalamus – pituitary – gonadal axis occurs at all levels The Hypothalamus Gonadal steroids influence GnRH-secreting neurones. They are also affected by their connection to other parts of the brain influenced by factors such as body weight and changes in the environment. In the male: In the female: Testosterone inhibits secretion of GnRH Oestrogen at moderate concentration inhibits secretion of GnRH Progesterone enhances the inhibitory effect of oestrogen Reproductive System Module – Tutors Handbook 9 Moderate oestrogen reduces the amount of GnRH secreted per pulse, progesterone the frequency of pulses Oestrogen at high LH ‘surge’ concentration promotes the release of GnRH producing an Progesterone prevents high levels of oestrogen producing a GnRH surge thus blocking the LH surge The Anterior Pituitary Gonadotrophs: Secrete both FSH and LH in response to pulsatile secretion of GnRH by the hypothalamus The amount of FSH and LH secreted in response to each pulse is affected by: - Oestrogen at moderate concentration which reduces it - Oestrogen at high concentration which promotes it The amount of FSH secreted in response to GnRH is reduced by inhibin ,a protein hormone produced by developing follicles in the ovary and seminiferous tubules in the testis. The Gonads In the testis LH stimulates the secretion of testosterone by Leydig Cells. Men secrete 4-10 mg each day. The amount of testosterone secreted at a given LH level is relatively constant. In the Ovary During the early phase of follicular development: - theca interna cells bind LH and are stimulated to produce androgens(principally androstenedione) Granulosa cells bind FSH and are stimulated to produce enzymes which convert these androgens to oestrogens - As the follicle grows more oestrogens are produced for a given gonadotrophic stimulation In the pre-ovulatory phase - LH receptors develop in outer layers of granulosa cells - The oestrogen concentration is now high and triggers a ‘surge’ of LH which will stimulate ovulation After ovulation - LH stimulates the corpus luteum to secrete progesterone and oestrogen - As the corpus luteum grows more steroids ( oestrogen and progesterone) are produced at a given LH concentration In the female therefore, the events of the ovarian cycle influence the response to gonadotrophins. This variation produces a so-called ‘ovarian’ or ‘pelvic’ ‘clock’, which is important in controlling the reproductive cycle of the female. + Pregnenolone DHEA Basement Membrane LH Capillary Cholesterol Cholesterol + LH Pregnenolone Progesterone Androstenedione + Androstenedione Testosterone Thecal Cell Testosterone FSH + Oestradiol Oestrone Granulosa Cell The Testis LH acts upon Leydig cells to promote the secretion of testosterone. The effects of LH are enhanced by prolactin and inhibin FSH maintains Sertoli cells and makes them responsive to testosterone Testosterone acts on Sertoli cells to promote spermatogenesis . Testosterone acts elsewhere in the body to maintain the male reproductive system So long as LH and FSH are appropriate both spermatogenesis and testosterone secretion (and hence the rest of the reproductive system) will be maintained. Operation of the Whole System in the Male The male must produce sperm constantly, and be ever ready to deliver them to the female. This requires constant, appropriate levels of FSH, LH and testosterone. These are achieved by negative feedback: If testosterone levels tend to rise this will inhibit GnRH secretion, so reducing production of LH and FSH Levels are reduced further by testosterone reducing sensitivity of gonadotrophs to GnRH So testosterone levels fall back If spermatogenesis proceeds too rapidly inhibin levels rise Inhibin reduces secretion of FSH by acting on gonadotrophs in the pituitary Reproductive System Module – Tutors Handbook 11 4.1 Complete these flow charts showing hormonal feedback control mechanisms. Add the names of the hormones released and the feedback control mechanisms to the anterior pituitary and hypothalamus. In the male: (-) Hypothalamus GnRH (-) (FSH only) (-) (LH only) Anterior Pituitary FSH LH Sertoli Cells Leydig Cells Testes Inhibin Testosterone (-) Negative Feedback control Effects in Reproductive Tract and other organs 4.2 In the female the picture is complex as hormone levels, function and control vary according to the phase of the menstrual cycle. Complete this flow chart for middle follicular phase; i.e., before ovulation has occurred. (-) Hypothalamus (?) GnRH (-) (FSH only) (-) Anterior Pituitary FSH LH Granulosa Cells Theca Cells Ovaries Androgens Inhibin Oestrogen Effects in Reproductive Tract and other organs (-) Negative Feedback control Reproductive System Module – Tutors Handbook 13 4.3 Complete this flow chart, again for the female, but now as is occurring at ovulation showing positive feedback. (+) Hypothalamus GnRH (+) Anterior Pituitary (Hormone) LH surge Ovaries Ovulation (Effect on ovary) (Hormone) Oestrogen (+) Positive Feedback 4.4 Discriminate between the roles of oestrogen in the early follicular phase and its role at ovulation. In the early follicular phase, ( which is dominated by oestrogen) oestrogen at low levels exerts a negative (inhibitory) feedback on gonadotrophin release. As the follicle grows and ovulation approaches at mid cycle, the rising levels of oestrogen have become such that a positive (stimulatory) feedback occurs producing a surge of LH release. 4.5 At the menopause the ovary contains dwindling number of follicles. What will happen to: Oestrogen secretion o plasma FSH o the secretion of GnRH from the hypothalamus? Oestrogen secretion wanes FSH levels will rise considerably GnRH levels will rise Because Feedback from gonadal steroids much reduced 4.6 In pregnancy, once the placenta has developed it begins to secrete oestrogen and progesterone. The secretion is independent of LH and FSH. What will happen to: o Plasma levels of FSH o Plasma levels of LH o Hypothalamic secretion of GnRH in a pregnant woman? FSH levels will fall LH levels will fall GnRH levels will fall Because placental oestrogen & progesterone exert negative feedback inhibition at both hypothalamus and pituitary Reproductive System Module – Tutors Handbook 15 4.7 The drug clomiphene is an oestrogen antagonist sometimes used in the treatment of infertility. It is given for 5 days at the start of the menstrual cycle What will be the effects on: o GnRH secretion o Plasma levels of FSH and LH GnRH secretion will rise as clomiphene antagonises feedback inhibition LH & FSH secretion will also rise, with a larger increase in LH levels as FSH is suppressed by inhibin 4.8 What would be the effects on gonadotrophin secretion of a constant moderately high dose of a progesterone like drug? Progesterone enhances negative feedback of oestrogen At moderate / high doses this will reduce LH and FSH secretion And it will block positive feedback effect of high oestrogen, so no LH surges So ovulation is suppressed (you’ll see this when we talk about progesterone implants for contraception) 4.9 Would a constant low dose of a progesterone like drug have the same effect? In this case which parts of the reproductive system might still be affected? At lower doses, progesterone does not reliably block the effect of high oestrogen so does not reliably prevent an LH surge and ovulation will probably still occur But low dose progestogens will affect cervical mucus, making it acidic and inhibiting sperm transport ( you’ll see this when we talk about the mini-pill ) 4.10 If the anterior pituitary gland is transplanted to another site in the body the secretion of LH, FSH, TSH, GH and ACTH falls to negligible levels. Why? Releasing hormones are diluted to ineffective concentrations in the general circulation. The portal nature of the hypophyseal vessels normally ensures that releasing hormones reach the pituitary at relatively high concentration 4.11 The transplanted anterior pituitary, however, hypersecretes prolactin. Why? A major part of control of prolactin secretion is inhibition by dopamine. This is removed if the anterior pituitary is transplanted and the dopamine is diluted in the general circulation 4.12 The major hypothalamic hormone inhibiting prolactin secretion is dopamine (prolactin inhibitory hormone). The actions of dopamine are mimicked by the drug bromocriptine and antagonised by drugs like haloperidol, metoclopramide and domperidone. What will happen to prolactin levels if a woman is given bromocriptine? They should fall, as it mimics the inhibitory effect of dopamine on lactotrophs 4.13. Prolactin, and particularly hyperprolactinaemia, suppresses fertility by disturbing the pulsatile release of GnRH. What do you think might happen to the fertility of a woman given metoclopramide? Fertility may be reduced, as prolactin levels rise because the inhibitory effects of dopamine are themselves inhibited since metoclopramide inhibits dopamine (Steroidal synthesis figures have been adapted from Medical Physiology, 2nd Edition, Rhoades, RA and Tanner, GA. Lippincott and Wilkins) Reproductive System Module – Tutors Handbook 17