Medicaid Application for Intensive Outpatient
advertisement
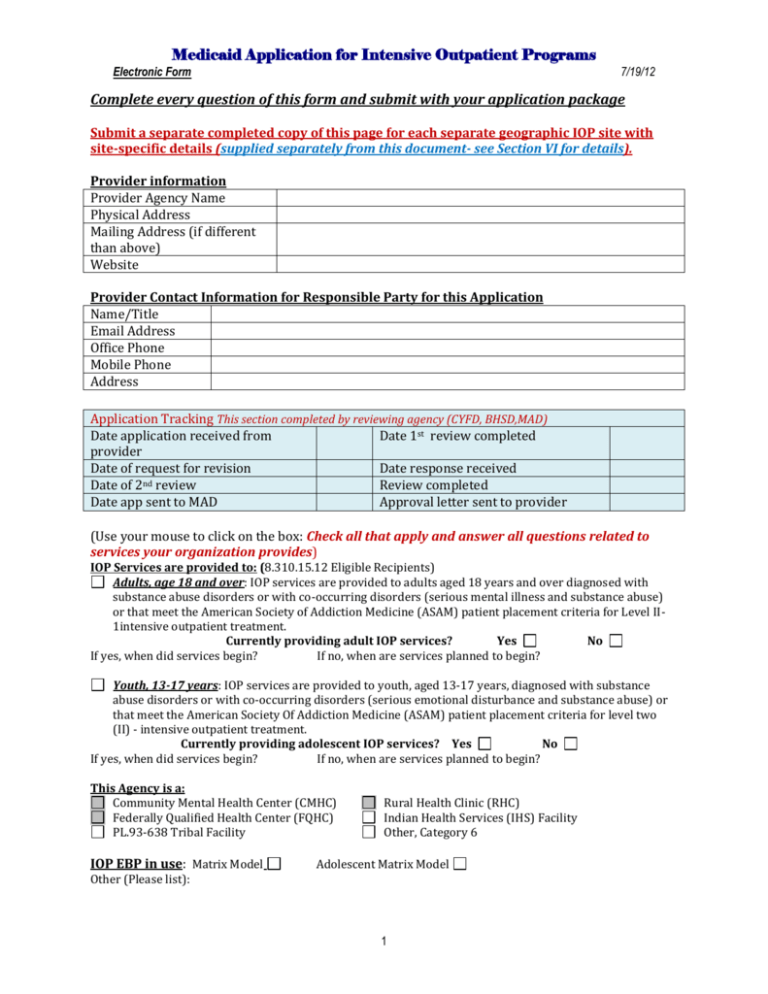
Medicaid Application for Intensive Outpatient Programs
Electronic Form
7/19/12
Complete every question of this form and submit with your application package
Submit a separate completed copy of this page for each separate geographic IOP site with
site-specific details (supplied separately from this document- see Section VI for details).
Provider information
Provider Agency Name
Physical Address
Mailing Address (if different
than above)
Website
Provider Contact Information for Responsible Party for this Application
Name/Title
Email Address
Office Phone
Mobile Phone
Address
Application Tracking This section completed by reviewing agency (CYFD, BHSD,MAD)
Date application received from
Date 1st review completed
provider
Date of request for revision
Date response received
Date of 2nd review
Review completed
Date app sent to MAD
Approval letter sent to provider
(Use your mouse to click on the box: Check all that apply and answer all questions related to
services your organization provides)
IOP Services are provided to: (8.310.15.12 Eligible Recipients)
Adults, age 18 and over: IOP services are provided to adults aged 18 years and over diagnosed with
substance abuse disorders or with co-occurring disorders (serious mental illness and substance abuse)
or that meet the American Society of Addiction Medicine (ASAM) patient placement criteria for Level II1intensive outpatient treatment.
Currently providing adult IOP services?
Yes
No
If yes, when did services begin?
If no, when are services planned to begin?
Youth, 13-17 years: IOP services are provided to youth, aged 13-17 years, diagnosed with substance
abuse disorders or with co-occurring disorders (serious emotional disturbance and substance abuse) or
that meet the American Society Of Addiction Medicine (ASAM) patient placement criteria for level two
(II) - intensive outpatient treatment.
Currently providing adolescent IOP services? Yes
No
If yes, when did services begin?
If no, when are services planned to begin?
This Agency is a:
Community Mental Health Center (CMHC)
Federally Qualified Health Center (FQHC)
PL.93-638 Tribal Facility
IOP EBP in use: Matrix Model
Rural Health Clinic (RHC)
Indian Health Services (IHS) Facility
Other, Category 6
Adolescent Matrix Model
Other (Please list):
1
Medicaid Application for Intensive Outpatient Programs
Electronic Form
7/19/12
SECTION I: INSTRUCTIONS
Please read all instructions before you proceed.
Exclusions, omissions, and poor organization are likely to result in requests for more
information or resubmission of the entire application packet and will cause the review
process to proceed more slowly.
You must submit applications for adult IOP to HSD/BHSD, and applications for adolescent
IOP to CYFD. Do not submit applications directly to HSD/MAD.
1. The following application is to provide guidance for you to assemble the required
materials for a complete IOP application to hasten approval for service. Please carefully
review the accompanying Medicaid Assistance Division (MAD) Application Tool
(separate from this document) and this list to make sure that you respond to all the
listed components here and specifically as noted in the Application Tool.
2. Your finished document should NOT include EBP manuals, descriptions of practices ,
training materials, philosophical discussions, or any other sort of practice, other than
those embedded in the policy and procedures (P&P). P&P is not a forum for practice
discussion, but are concise policy statements and concise procedural statements. We
MUST know your policy, and how you implement your policy as a procedure. Please do
not send extraneous materials. (an example P&P is available by request)
3. It is mandatory that the CYFD/HSD/MAD application document cover-sheet be
completed, with all names, locations, dates, check boxes checked, and each item listed
included in your packet and reviewed and checked for accuracy and completeness prior
to submission.
4. You must construct a table of contents for ALL documents (P&P, forms, org chart,
releases, other policies or Standard Operating Procedures, etc).
5. TAB YOUR APPLICATION RESPONSE so that each item listed on the MAD IOP Application
can be easily located or found in your submission. The purpose for doing this thoroughly
is to make certain that the reviewers actually locate what you have included rather than
return your application as incomplete.
6. Submit the agency general policy and procedures. Also, submit any IOP specific Policy or
Procedure, or IOP procedural and IOP guidance documents that address all IOP specific
issues listed in the MAD Audit Tool- Do Not Submit EBP manuals, curricula, or workbooks
The following outline for a complete P&P manual is listed for your review and to aid your
application development. A complete P&P manual is available upon request:
A.
Organization Description
1. Organization Overview
2. Organization Management & Governance
3. Organizational Chart
4. Mission Statement
5. Statement of Values, Principles, and Ethics
a. Confidentiality Related to HIPAA and 42 CFR Part 2
6. Consumer Rights & Grievance Policy
2
Medicaid Application for Intensive Outpatient Programs
Electronic Form
B.
C.
D.
E.
F.
G.
7/19/12
7. Organization Non-Clinical Policies
a. Other Standard Operating Procedures
8. Links to other organizations, consortiums, or information related to intended
mergers, service area expansions, and changes or additions to geographic
locations, etc
9. Community Collaboration
Hazard Plan/Emergency Management
a. Hazard
b. Fire Plan
Funding and Financial Management
Human Resource Management
a. Human Resource Policy
b. Agency Non-discrimination Policy
c. Employees
d. Contract Staff
e. Personnel File Management Plan
f. Job Descriptions
g. All forms related to the preceding P&P
Overview AND Clinical Policies of Services Provided (LIST ALL, such as)
a. Outpatient Counseling Services
b. School-based Counseling Services
c. Intensive Outpatient Program
d. Case Management
e. Trauma-informed Work
f. Justice System/Drug Court Engagement & Services
g. Related forms
Philosophy of Approach & Principles of Practice
1. Engagement, Alliance and Rapport
2. Guiding Principles of Recovery
3. Cultural Competency
4. Gender Competency
5. Stage-Wise Interventions
6. Motivational Approaches
7. Trauma-Informed System of Care
8. Related forms
Initial Procedures of Care & Planning
1. Initiation of and Retention Into Behavioral Health Services
2. Intake Processes
3. Assessment
4. Individualized, Comprehensive, Integrated Service Plan
a. Safety Planning
b. Crisis Planning
c. Suicidality
d. Relapse prevention
e. Aftercare/discharge planning
5. Individual Case Files
6. Related forms
Personnel, Team and Systems Competencies
1. Staff Competencies
2. Co-Occurring Disorders Competencies
3. Organization Supervision
4. Service Teams/Multi-Disciplinary Teams
3
Medicaid Application for Intensive Outpatient Programs
Electronic Form
H.
7/19/12
5. Quality Management
6. Electronic Systems Competencies and Records Keeping (if applicable)
7. Related forms
Treatment Implementation Practice Standards
1. Research and Evidence-based Treatment Approaches (EBP)
2. EBP Adaptations for Particular Populations Served
3. Life and Prosocial Skills
4. Encouraging and Monitoring Abstinence
5. Medication Management and Medically Assisted Treatment Services
6. Multifamily Group Engagement Practices
7. Service Integration
8. Related forms
7. Clearly state in your appropriate P&P that you:
a. adhere to all appropriate billing and coding requirements related to municipal,
county, Tribal, state, and federal requirements,
b. comply with all applicable Medicaid IOP regulations related to billing, licensure and
scope of practice regulations
c. have specific P&P related to MAD requirements for supervision related to license
level and comply with hiring practices related to these.
d. know and understand the scope of various licenses as they pertain to Medicaid billing
and services,
e. and strictly adhere to the appropriate regulations related to limitations of licensure.
SECTION II: Check List for items to be included in the application submission
The following check list is provided to help you make sure that you have included all necessary
elements for the IOP Application.
Check each box as completed or included in your application packet:
Provider general Policy and Procedures
IOP specific Policy and Procedure as appropriate
Blank supervision logs and forms (examples) related to individuals receiving IOP services
Multi-disciplinary team meeting/IOP service team meeting schedules, and roster of types of
positions held (supervisor, CSW, primary clinician, IOP clinician, etc) by the persons who will be
attending each team meeting. In actual use, documents with the names and positions of persons
attending team meetings should be maintained by the Supervisor.
Check one only (these items are listed and defined in the MAD Application. Choose one only based
on what best fits what you do related to the definition. Specifically include the statement of
team leadership by the Clinical Supervisor in your supervision P&P)
IOP Service Team
Multi-disciplinary Team
Staff training schedule and attendee roster of planned and previously conducted training
events
Staff one time training events and attendee roster, or as identified by need
Annual or regular/recurrent training and attendee roster; please note timeline
Statement of Client Rights to be provided to each Medicaid consumer with line for signatures;
include both OHNM and Medicaid rights to administrative (fair) hearings,
http://www.hsd.state.nm.us/oig/
HSD Fair Hearing Bureau;
https://www.optumhealthnewmexico.com/provider/pdf/RightsPosterENG_dec17.pdf
4
Medicaid Application for Intensive Outpatient Programs
Electronic Form
7/19/12
Vision, Mission, Values, or other statements of organizational intent (may include brochures
and/or brief statements about services offered)
IOP staff job descriptions (see personnel files to avoid duplication)
SECTION III: Make certain the following are included in your application packet.
Check each box related to completion:
The IOP EBP of choice has been identified on the cover sheet. The following are specifically
addressed in the P&P:
IOP Schedules
P&P statement related to Service Intensity
P&P statement related to Service duration
P&P statement related to plans for step down or up related to intensity of services
Agency level Quality Management and evaluation plans for your organization (if part of
General P&P, there is no need to duplicate separately.
Quality Management and evaluation plans related to IOP (if part of P&P, do not duplicate as
long as IOP is specifically listed as part of the QA process)
SECTION IV: Checklist of forms to submit with your application packet:
F3. Before engaging in an IOP program, the eligible recipient must have a treatment file that
contains a diagnostic evaluation (Assessment H0031-U8) or a Diagnostic/Evaluation (90801) or other
diagnostic evaluation as approved by MAD) and an individualized service plan that includes IOP as an
intervention.
(8.310.15.12-C)
1. An Individual Service Plan that allocates space to address all issues/domains
identified during intake and the Assessment/Diagnostic evaluation
2. A form that specifically addresses all assessed co-occurring disorders, or a
specifically labeled section of the service plan document for COD.
3. A narrative summary (by whatever name) that succinctly describes the interaction of cooccurring disorders, as well as can be described at the time of intake and assessment
4. A relapse and/or crisis plan form, or section in the treatment plan (may be the same
document)
5. A designated place on service plans and progress notes for each treatment session
including:
o IOP group sessions and related services, and
o Individual counseling, and
o Psycho-education, family counseling, or other services as specified in the IOP EBP (as
appropriate to issues related to confidentiality and privacy), and,
o Stage of Change/Treatment Readiness, and,
o Other co-morbid issues identified during intake, assessment or service planning
6. A place on records and notes pertaining to how all other domains of service identified in the
assessment/evaluation have been addressed in the service plan
7. A place for the consumer and/or parent/guardian, as appropriate, to identify and agree to
specific, personal goals of treatment on service planning documents and sign documents
appropriately
8. Copies of the Release of Information forms specific to treatment needs (may include
individuals or other agencies providing services or oversight)
SECTION V: Documents that must be provided by agency if applying for enrollment as an IOP
agency requesting approval from MAD. Please submit blank example documents as appropriate. The
following list is excerpted from the MAD Application Tool:
5
Medicaid Application for Intensive Outpatient Programs
Electronic Form
7/19/12
1. Client rights and grievance procedures (with signature spaces for inclusion in the
Case File) that include the Single Entity’s and FFS rights for fair hearings.
2. Client Contract with agency (a guardian signature line for appropriate adolescent
clients)
3. Discharge planning documentation that:
a. Reflects recovery and resiliency efforts
b. Is developed at the start of services and is updated as necessary to reflect the
growth and needs of the consumer so the treatment plan and discharge plan are
consistent and cohesive
c. Includes evidence of planning and follow-up for family and community supports
and collaboration
d. Reflects the developmental level/stage of readiness and any unique
circumstances for the identified consumer to continue a successful sobriety
e. Includes concrete steps that support the consumer in recovery and resiliency
f. Includes service step-up or step-down, and exit criteria from ASAM Level II.1
services: IOP services or diagnosed with substance abuse disorders or with cooccurring disorders as specified by the diagnostician documented in Assessment
(H0031-U8) or a Diagnostic/Evaluation (90801) or other diagnostic evaluation as
approved by the Medical Assistance Division that is current, (within 12 months)
completed, signed and dated by a licensed clinician under the supervision of a
licensed Independent Clinician
Organization Chart (if included as part of P&P, do not duplicate){see Multiple Site application
instructions for multiple sites}
Other attachments and addendums (may include staff policy manuals, staff guidelines for
dealing with crises/suicide/client and staff safety, crisis planning documents, critical incident
management and documentation, suicidality response, assessment and reporting, violence and
threats of harm to self or others response/management, and other documentation as specified
in the Application Tool, etc.)
Clinical Policies (if not included in General P&P)
HR Policies (if not included in General P&P)
Supervision forms and logs for individual, group, team, including attendance records, schedules,
rosters, etc, that specifically record subjects addressed, follow-up from session to session, and
regularity of occurrence.
Evidence of how fidelity to evidence-based practices and programs is maintained/monitored
through training and supervision
SECTION VI: Multiple geographic IOP sites application procedures
A. It is mandatory that you submit a separate cover sheet for each site (the electronic
application cover sheet, included) with the site specific address and contact person at
that site.
B. All other information specific to the site may be included in a letter if it does not require
amending policy and procedure, or other specific guidance documents, and must include
all of the following pertaining to the site:
1. Site specific statement of service needs and intended target population, and links to other
community service agencies that may be providing similar or the same services
2. All site-specific changes to policy and procedures and standard operating procedures
3. Clinical practices and staffing if there are differences
6
Medicaid Application for Intensive Outpatient Programs
Electronic Form
4.
5.
6.
7.
8.
9.
10.
11.
7/19/12
Cultural adaptations as appropriate to location
Funding sources other than Medicaid that are used to serve the identified population
HR and personnel, job descriptions
An organization chart inclusive of multiple IOP sites illustrating how they fit with
your central agency
Crisis management/crisis lines/availability
How oversight from the main agency is conducted; links and on-site management
All changes in supervisory practices, including:
a. Qualifications for employment or contract services hired for supervision
b. Schedules, logs, records maintenance and review
c. Team composition and schedules
d. EBP fidelity supervision that meets Medicaid IOP requirements
e. Coverage and duties specific to site, crisis line access, etc
Site specific hazard/emergency management (does not need to modify the general P&P, but
must specify how site specific safety planning, fire escape planning, etc, is managed)
C. You must complete a separate MAD Provider Participation Agreement (MAD PPA 335) for
each site. Each site will be enrolled with an unique MAD provider number. Please submit the
completed MAD PPA with this application. BHSD or CYFD will forward to HSD/MAD so
that once the application is approved, your MAD PPA will be processed. Please use the
corresponding MAD provider number of each site when requesting credentialing from
OHNM and when submitting claims. The PPA can be found at:
http://www.hsd.state.nm.us/mad/PEnrollmentPolicy.html
SECTION VII: Application Processes
Audit Process: Once you submit your application and your agency is given a preliminary
approval letter by HSD/MAD, you will receive a site visit from either BHSD or CYFD within 180
days as the last step in approving your IOP program. The attached MAD IOP Audit tool is
provided as a guide to prepare your agency for that visit, as well as future site visits. This tool
will provide you with the foundation for developing and implementing a stable and sustainable
IOP program. BHSD and CYFD are ready to assist you in all phases of this process to help you
succeed.
If your application is denied, you will be provided with documentation of the areas with
deficiencies and will have the opportunity to resubmit an application. It is strongly
recommended that you utilize the instruction and the audit tools and obtain technical
assistance from BHSD and CYFD staff.
7
Medicaid Application for Intensive Outpatient Programs
Electronic Form
7/19/12
All items listed in bold-faced, underlined text in the “Assessment Criteria” column are pass/fail. The Provider must demonstrate that these items
have been adequately supported in the documents submitted in their application. If any one of these items fails, then the application as a whole
fails. It is MAD’s intent that upon approval of this application, the Provider will implement their MAD IOP program in accordance with the approved
policies and procedures as submitted. The use of the clinical practice standards, evidence-based practices, and the most current Service Definition
provide guidance to the Provider of the information necessary to be approved as a MAD IOP provider. The Provider must comply with all sections of
MAD 8.310.15 NMAC, Intensive Outpatient Services rule.
If the Provider is proposing multiple sites, the responses, documents, policies/procedures must specifically address how the agency will coordinate
and collaborate between the sites. In particular, how staffing, supervision, and training will be managed. Each site will be individually provisionally
and fully enrolled.
If the Provider is proposing to serve both adolescents and adults, the application must specifically detail the uniqueness of each population in its
policies/procedures, documents and responses.
A. Agency Policies and Procedures/Standard Operating Procedures (SOP)/IOP Guidelines
Item
Audit Activity (Desk)
Yes
No
Comments (identify comment by number)
All Items Underlined and in Bold Font Are
Pass/Fail
Regulation: “The IOP services are provided through an integrated multi-disciplinary approach or through coordinated, concurrent services with behavioral health
providers, with the intent that the IOP shall not exclude consumers with co-occurring disorders”. In order to meet this requirement a provider must have in place
either an IOP Service Team (AKA Treatment Team) when the approach is through coordinated concurrent services; or, a Multidisciplinary Team (MDT) when the
approach is through an integrated multi-disciplinary approach.
Description:
1. IOP service team (AKA treatment team): The IOP Service Team is comprised of the agency behavioral health providers and is led by the IOP supervisor. IOP team
members are expected to maintain documented communication linkages with the consumer’s primary mental health providers and other critical service linkages as identified
in the assessment and treatment plan (e.g. HIV health care; criminal justice and so forth). Teams are in place to serve individuals or families that have service needs
identified in multiple domains, such as co-occurring substance and mental health disorders, and specifically assure that services are coordinated and consistent across
domains. The clinical supervisor maintains responsibility that staffing for all individuals meets requirements and addresses the needs identified by assessment and service
planning on a case-by-case basis during regularly scheduled staffing meetings.
2. Multi-disciplinary team (MDT): As possible and appropriate to the individuals needs and community capacity, the team will consist of the consumer and family/guardian,
natural supports, CCSS workers, psychiatrist, nurses, counselors and clinicians, case managers, CYFD staff, other ancillary providers (vocational, residential, housing,
criminal justice, hospital liaison), school, law enforcement, and courts, who all work collaboratively on the team and meet face-to-face led by the clinical IOP supervisor. The
MDT develops the initial treatment plan and then monitors the consumers’ progress in meet established goals and outcomes. Based on the documented period reviews by
the MDT, changes in approaches, goals, outcomes and linkages with other services across domains should occur.
8
Medicaid Application for Intensive Outpatient Programs
Electronic Form
7/19/12
A. Agency Policies and Procedures/Standard Operating Procedures (SOP)/IOP Guidelines
Item
3.
A1. The IOP services are provided through an
integrated multi-disciplinary approach or through
coordinated, concurrent services with behavioral health
providers, with the intent that the IOP service shall not
exclude consumers with co-occurring disorders.
(8.310.15.13)
Audit Activity (Desk)
All Items Underlined and in Bold Font Are
Pass/Fail
Yes
No
Comments (identify comment by number)
1. Provide Policies and Procedures that
specifically support an integrated
multidisciplinary team or IOP service
team.
2. Policies and Procedures specify the
frequency and regular scheduling of team
meetings.
1.
1.
1.
2.
2.
2.
Description: provision of services: The intent of IOP services is to enable providers to make available high quality, comprehensive, evidence-based behavioral healthcare
that maximizes integration of mental health and substance services related to medical necessity determined during assessment and evaluation. Due to the structure of current
evidence-based program as primarily substance disorder related curricula, many mental health issues may need to be addressed during individual counseling or psychoeducational groups.
A2. Provision of substance, mental health, or COD
1. Provide Policies and Procedures that
1.
1.
1.
services (8.310.15.14-D)
support the provision and integration of
mental health and substance abuse
services, inclusive of co-occurring
disorders, high-risk situations and crisis
planning and intervention.
Description: Time-limited and multi-faceted services: Each current evidence-based program specifies the dosage and duration of services. For persons with severe
mental illness, dosage may be reduced and duration increased as appropriate as determined in the service plan. Services are provided through IOP groups, individual
counseling, and psycho-education groups.
Description: The duration of IOP intervention is typically from three to six months; the amount of weekly services is directly related to the goals and objectives specified in the
eligible recipient’s treatment or service plan. (8.310.15.14.E) Ongoing eligibility will be effectively established through 90 day updates to the service plan document if
the IOP course of treatment is longer than 90 days duration. The evidence-based curriculum specifies intensity and duration of the normal course of treatment. In
addition, persons experiencing severe mental illness with substance related disorders may need adjustments to the mix between intensity and duration, such that
intensity may be reduced with duration of treatment service increased. This must be addressed on a case-by-case basis with sufficient and definitive
documentation supporting medical necessity and appropriateness of IOP treatment.
IDDT best practice course of treatment: The approved IDDT model incorporates a course of treatment IOP curriculum that specifies intensity and duration of treatment, and
9
Medicaid Application for Intensive Outpatient Programs
Electronic Form
7/19/12
A. Agency Policies and Procedures/Standard Operating Procedures (SOP)/IOP Guidelines
Item
Audit Activity (Desk)
Yes
All Items Underlined and in Bold Font Are
Pass/Fail
demonstrates medical necessity at 90 day intervals through updates to the individual’s service plan document.
No
Comments (identify comment by number)
A3. IOP services provide a time-limited, multi-faceted
1. Provide Policies and
approach to treatment service for eligible recipients who
Procedures/SOP/IOP guidelines that
require structure and support to achieve and sustain
specify time-limit (duration) of IOP
recovery. (8.310.15.13) (8.310.15.14-E)
services (as recommended by the EBP
utilized).
2. Specify the IOP guidelines that the
intensity of weekly services will be
directly related to the goals and
objectives specified in the
treatment/service plan and are aligned
with the IOP EBP curriculum.
3. IOP guidelines specify service plan updates
at 90 days.
4. Policies and Procedures specify that IOP
services are integrated with other services
at provider agency.
1.
1.
1.
2.
2.
2.
3.
3.
3.
4.
4.
4.
A4. Research-based model specific to IOP services
(8.310.15.14-F)
IOP services must be rendered through a researchbased model:
(1) Matrix Model Adult Treatment Model
(2) Matrix Model Adolescent Treatment Model
(3) Minnesota Treatment Model
(4) Integrated Dual Disorder Treatment
(5) any models other than those identified above must
be approved by HSD or its authorized agents.
G.
Services not provided in accordance with the
conditions for coverage as specified in 8.327.0.10 and
8.327.0.14 NMAC, Intensive Outpatient Program
Services, are not considered covered services and are
subject to recoupment
1a.
1a.
1a.
1b.
1b.
1b.
2.
2.
2.
3.
3.
3.
1a. The provider uses one of the EBP
models specified in the regulations.
1b. If not, specify (in comments section)
what curriculum is used and if it is
approved.
2. Provide Policies and Procedures that
specify formal training in the provider’s
EBP IOP curriculum for IOP supervisor.
3. Policies and Procedures specify training in
the provider’s EBP IOP curriculum for IOP
clinicians. (Note: training does not have to
be formal and can be conducted by clinical
supervisor.)
10
Medicaid Application for Intensive Outpatient Programs
Electronic Form
7/19/12
A. Agency Policies and Procedures/Standard Operating Procedures (SOP)/IOP Guidelines
Item
Audit Activity (Desk)
All Items Underlined and in Bold Font Are
Pass/Fail
Yes
No
Comments (identify comment by number)
Description: Co-occurring disorders: The term co-occurring disorders (COD) refers to co-occurring substance-related and mental/emotional disorders. Persons said to
have COD have one or more substance related disorders as well as one or more mental disorders. At least one disorder of each type can be established independent of the
other and is not simply a cluster of symptoms resulting from a single disorder. When assessment is carefully conducted, the symptoms of each diagnosis that contribute to the
functional impairment(s) will be clearly ascertained, communicated, and addressed. What this means in practical terms is that a simple diagnosis of SMI, SED/At Risk or
substance use patterns will not suffice to present a clear picture of how an individual experiencing COD will manifest symptoms; that the presentation of impairment may be
powerfully increased or decreased based upon the persons constitution and susceptibility and the specific interactions between substance use and the mental illness. It is
likely that the symptoms of one disorder will have effect on the other disorder. (the New Mexico COD Competent Intensive Outpatient Program Manual)
A5. Treatment services should address co-occurring
1. Provide Policies and Procedures that
1.
1.
1.
mental health disorders, as well as substance use
specify an assessment protocol for COD
disorders, when indicated. (8.310.15.13)
consumers.
2. Policies and Procedures specify that an
2.
2.
2.
integrated summary describing the
interactions or the interrelated effects of the
disorder dynamic for the co-occurring
diagnoses is included in the assessment.
Description: Cultural sensitivity and recovery/resiliency: A workable definition of culture is: a shared system of symbols, beliefs, attitudes, values, expectations, and norms
of behavior. Recovery-oriented care is what clinical mental health, addiction treatment, and integrated service practitioners offer in support of the individual/family’s own
recovery efforts. The recovery process refers to how persons with or impacted by a mental and/or substance disorder actively manage the disorders and reclaim their lives in
the community.
A6. Services must be culturally sensitive and
1. Provide Policies and Procedures that
1.
1.
1.
incorporate recovery and resiliency values into all
support recovery and resiliency values,
service interventions. (8.310.15.13)
or as evidenced in a Bill of Client Rights,
Vision, Values, or other statements of
organizational intent.
2. Provide Policies and Procedures that
2.
2.
2.
support culturally sensitive values, or as
evidenced in Vision, Mission, or other
statements of organizational intent.
11
Medicaid Application for Intensive Outpatient Programs
Electronic Form
7/19/12
A. Agency Policies and Procedures/Standard Operating Procedures (SOP)/IOP Guidelines
Item
Audit Activity (Desk)
All Items Underlined and in Bold Font Are
Pass/Fail
Yes
No
Comments (identify comment by number)
Description: Medication management services: Pharmacotherapy and medication management includes the use of appropriate medications to manage substance, mental
health or co-occurring disorders and use of a recovery-based approach including shared decision making, informed consent, and an active role on multi-disciplinary teams.
A7. Medication management services are available to
1. Provide Policies and Procedures that
1.
1.
1.
oversee use of psychotropic medications. (8.310.15.14specify that medication management
D)
services specific to substance-related,
mental and emotional, or co-occurring
disorders COD are available for IOP
service recipients (either in-house or
by referral), and that there how the
provider will document linkage to the
service team personnel.
A8. Documents that must be provided by agency if
applying for enrollment as an IOP agency requesting
approval from MAD.
1. Organizational Chart
2. Clinical IOP Employee Training Plan that
specifically includes IOP model training
including protocols when dealing with
disruptive or potential suicidal client
behavior)
3. Protocol for referring recipients to a 24hour Crisis Line
1.
2.
1.
2.
1.
2.
3.
3.
3.
4. If the agency is conducting drug
screenings, Urinalysis Collection Protocol
and accompanying form utilized
5. If agency does medicine administration,
Medication Administration Protocol and
accompanying form utilized
4.
4.
4.
5.
5.
5.
12
Medicaid Application for Intensive Outpatient Programs
Electronic Form
B.
7/19/12
Quality Management Documentation
Item
Audit Activity (Desk)
Yes
No
Comments (identify comment by number)
Description: Evaluation: quality management processes ensure that the review, evaluation, editing, changes or adaptations of all policies and procedures, SOP’s, etc, occur
on an annual or as needed basis to ensure that they are current with all other applicable change and modifications to the organization business stance, funding changes,
service implementation changes, staff changes, etc. Professional and clinical supervision processes are reviewed and evaluated to ensure that all required supervisory
practices are adequately accomplished and implemented. QA monitors, evaluates and assesses outcome measures identified by the consumer, the provider or by the
purchaser of services. Quality management reviews record keeping and data management, HIPAA, 42 CFR Part 2, etc, the QA officer and committee review records and
record keeping processes to assess that satisfactory records and documentation are maintained and protected adequately.
B. IOP providers are required to develop and implement 1. Provide the IOP-specific program
1.
1.
1.
a program evaluation system. (8.310.15.10-F)
evaluation (quality management) to be
utilized.
2. Describe how the IOP program will track
2.
2.
2.
fidelity to the model.
3. Describe quality management meetings
3.
3.
3.
that are regularly scheduled.
4. Describe how the IOP-specific program
4.
4.
4.
evaluation system will be used to track
and/or evaluate client outcomes. (Client
Outcomes may include customer
satisfaction surveys, retention into service
rates, drop-out rates, re-admittance/relapse
and lapse rates, incarceration or
hospitalization data, or readily identifiable
information and data specific to the IOP that
may be contained in the quality
management reports.)
B1. Documents that must be provided by agency if
applying for enrollment as an IOP agency requesting
approval from MAD.
1. Description of how program success
will be measured, such as:
Demographics of recipients serve; any
effect on the utilization of criminal justice
system by enrolled recipients; changes in
recipient employment; numbers and
reasons why recipients did not complete
IOP program.
2. IOP policies and forms to gather and
how this information will be internally
analyzed concerning recipient program
13
1.
1.
1.
2.
2.
2.
Medicaid Application for Intensive Outpatient Programs
Electronic Form
7/19/12
satisfaction and their beliefs of the
effectiveness of their services.
3. IOP policies and forms that will
summarize program successes and areas
of improvement and how this information
will be implemented by agency.
3.
3.
3.
C. Agendas, schedules, logs and related systems documentation
Item
Audit Activity (Desk)
Yes
No
Comments (identify comment by number)
Assessment Criteria
Description: Agendas, schedules, logs, and rosters: Provide evidence of meetings, training, service provision, case reviews, and supervisory scheduling.
Documents that must be provided by agency if applying 1. Specific to the agency IOP program –
1.
1.
1.
for enrollment as an IOP agency requesting approval
Supervision forms:
from MAD.
a. that reflect follow-up from
1a.
1a.
1a.
previous meetings
b. that document planned training
1b.
1b.
1b.
and follow-up those trainings
were attended and improvements
made in performance
c. schedule of individual
1c.
1c.
1c.
supervision dates and time
2. Ongoing employee training plan that
2.
2.
2.
specifically includes relevant
opportunities for staff to learn more
about IOP model fidelity and compliance
3. Training plan for staff on how to handle
potentially disruptive or unruly client
behavior
3.
3.
3.
Audit Activity- On Site
Assessment Criteria
1. Provide a job description for the IOP
clinical supervisor.
2. Specifically the job description details that
Yes
1.
No
1.
Comments (identify comment by number)
D. Supervision
Item
D1. Each IOP program must have a clinical supervisor.
The clinical supervisor may also serve as the IOP
program supervisor. Both clinical services and
14
1.
Medicaid Application for Intensive Outpatient Programs
Electronic Form
7/19/12
D. Supervision
supervision by licensed practitioners must be conducted
in accordance with respective licensing board
regulations. An IOP clinical supervisor must meet all the
requirements listed in column 2.
(8.310.15.10-E)
the supervisor:
a. Has an active licensure as an
independent practitioner
b. Has two years relevant experience with
IOP eligible recipients.
c. Has one year documented supervisory
experience.
d. Has education, formal, or staff
development in both mental health and
substance abuse treatment.
e. Has formal training and/or certification
for EBP IOP curriculum.
2a.
2a.
2a.
2b.
2b.
2b.
2c.
2c.
2c.
2d.
2d.
2d.
2e.
2e.
2e.
3. Provide the supervisory policies that
specify how supervision is to be provided
in high-risk or crisis situations.
3.
3.
3.
4. Provide the policies that specify
supervision for the provision of mental,
substance or co-occurring services
4.
4.
4.
Item
Assessment Criteria
1. Provide the forms that demonstrate that
recovery and resiliency values are
embedded in the job descriptions and
administrative and supervisory guidelines.
2. Provide training plans that cover recovery
and resiliency values for IOP staff.
3. Provide training plans that cover cultural
competency for IOP staff.
4. Provide documentation that the agency has
a plan to match linguistic facility to the
needs of the community served when
appropriate.
5. Provide documentation that the program will
No
1.
Comments (identify comment by number)
E1. Services must be culturally-sensitive and
incorporate recovery and resiliency values into all
service interventions. (8.310.15.13)
Yes
1.
2.
2.
2.
3.
3.
3.
4.
4.
4.
5.
5.
5.
E.
MAD Reviewer comment
Personnel Files
15
1.
Medicaid Application for Intensive Outpatient Programs
Electronic Form
E.
7/19/12
Personnel Files
E2. ELIGIBLE PROVIDERS: Services must be provided
within the scope of the practice and licensure for each
provider and must be in compliance with the statutes,
rules and regulations of the applicable practice act and
must be eligible for reimbursement as described in
8.310.8B-E NMAC Behavioral Health Professional
Services. (8.310.15.10-E)
E3, Documents that must be provided by agency if
applying for enrollment as an IOP agency requesting
approval from MAD.
attempt to have staff employed who are
representative of the community served.
6. Provide the plan on how translation
services to be made available to persons
with limited English proficiency.
7. Provide a plan on how services will be
made available to persons who are
communication impaired (blind, deaf, etc)
1. Provide policies to ensure that IOP
clinicians have active New Mexico
licensure that match the scope of
services they are providing.
2. Provide the program’s plan for the
education, formal training, or the staff
development specific to co-occurring
disorders for IOP clinicians. (Note: training
can include staff development and/or
training from clinical supervisor)
3. Provide the policy that will enforce that
IOP clinicians are trained in EBP IOP
curriculum in compliance with State of
NM MAD Rule. (training may be
conducted in-house by supervisory staff
who have attended formal EBP training)
4. Describe how staff will receive COD, EBP,
and other appropriate training as indicated
by their supervisor in either policy or
procedure.
1.Employee Performance Evaluation for
IOP program
6.
6.
6.
7.
7.
7.
1.
1.
1.
2.
2.
2.
3.
3.
3.
4.
4.
4.
1.
1.
1.
MAD Reviewer comment
F. Client Files
Item
F1a. IOP services are provided to youth, aged 13-17
Assessment Criteria
1. Provide the eligibility policies that
16
Yes
No
Comments (identify comment by number)
1.
1.
1.
Medicaid Application for Intensive Outpatient Programs
Electronic Form
7/19/12
years, diagnosed with substance abuse disorders or
with co-occurring disorders (serious emotional
disturbance and substance abuse) or that meet the
American Society Of Addiction Medicine (ASAM) patient
placement criteria for level two (II) - intensive outpatient
treatment.
F1b.
IOP services are provided to adults aged 18
years and over diagnosed with substance abuse
disorders or with co-occurring disorders (serious mental
illness and substance abuse) or that meet the ASAM
patient placement criteria for level two (II) - intensive
outpatient treatment.
(8.310.15.12-A and B)(See next row for a list of ASAM
criteria)
F2. ASAM: Levels of Care: (8.310.15.12-A)
Level 0.5: Early Intervention Services - Individuals with
problems or risk factors related to substance use, but for
whom an immediate substance -related disorder cannot
be confirmed
Opioid Maintenance Therapy (OMT) - Criteria for Level
I Outpatient OMT, but OMT in all levels
Level I Outpatient Treatment
Level II.1 Intensive Outpatient Treatment
Level II.5 Partial Hospitalization
Level III.1 Clinically-Managed, Low Intensity Residential
Treatment
Level III.3 Clinically-Managed, Medium Intensity
Residential Treatment (Adult Level only)
Level IV Medically-Managed Intensive Inpatient
Treatment
determine that an individual meets the
eligibility criterion of ASAM level II.1
services: IOP services or diagnosed with
substance abuse disorders or with cooccurring disorders as specified by the
diagnostician documented in
Assessment (H0031-U8) or a
Diagnostic/Evaluation (90801) or other
diagnostic evaluation as approved by the
Medical Assistance Division that is
current, (within 12 months) completed,
signed and dated by a licensed clinician
under the supervision of a licensed
Independent Clinician.
2. Provide the level of care specified in the
individualized service plan that specifies
the level of care and will address the
domains of service identified in the
Assessment/Diagnostic evaluation
appropriate to IOP services.
F3. Before engaging in an IOP program, the eligible
recipient must have a treatment file that contains a
diagnostic evaluation and an individualized service plan
that includes IOP as an intervention.
(8.310.15.12-C)
1. Provide the Individual Service Plan that
will address all issues identified in the
Assessment/Diagnostic evaluation
appropriate to IOP services.
2. Form does assess co-occurring
disorders addressed.
3. There is a relapse and/or crisis plan (may
be the same document).
4. There is place for progress note for each
Individual case files contain evidence of culturallysensitive and recovery and resiliency-based treatment.
(8.310.14.13)
17
2.
2.
2.
1.
1.
1.
2.
2.
2.
3.
3.
3.
4.
4.
4.
Medicaid Application for Intensive Outpatient Programs
Electronic Form
7/19/12
treatment session including:
IOP services, and/or
individual counseling, and/or
psycho-ed.
5. There is a place for records and notes
pertaining to how all other domains of
service identified in the
assessment/evaluation have been
addressed in the service plan.
6. There is a place for the consumer and/or
parent/guardian, as appropriate, to identify
and agree to specific, personal goals of
treatment, and signed documents
appropriately.
7. Provide a copy of the Release of
Information forms specific to treatment
needs (may include individuals or other
agencies providing services).
8. Provide a copy of the Client Bill of Rights
that will be signed and located in the
client’s chart.
9. Provide a copy of the note to be utilized
related to input from the IOP service team
or MDT.
10. Provide a copy of the treatment
schedule/attendance document. It should
have the ability to track and match the
recommended EBP service intensity
specific to client needs and capability as
documented in the Assessment (H0031U8) or a Diagnostic/Evaluation (90801) or
other diagnostic evaluation as approved by
the Medical Assistance Division.
11. Provide the policy or procedure that
directs that a Diagnostic Evaluation
(90801) Assessment (H0031-U8) or
other diagnostic evaluation as
approved by the Medical Assistance
Division is to be current, (within 12
18
5.
5.
5.
6.
6.
6.
7.
7.
7.
8.
8.
8.
9.
9.
9.
10.
10.
10.
11.
11.
11.
Medicaid Application for Intensive Outpatient Programs
Electronic Form
7/19/12
months) stating it must be completed,
signed and dated by a licensed clinician
under the supervision of a licensed
Independent Clinician.
12. If applicable and appropriate, provide a
copy of the policy or procedure detailing
medication management services provided
to the client either in-house or by referral,
and are all medication services and how
the referrals will be adequately
documented.
12.
12.
12.
Certification –individual(s) completing application:
Provider Representative
Print name
Date
Signature
Print name
Date
Signature
Provider Representative
19