Medicines Purchasing for Safety Policy
advertisement
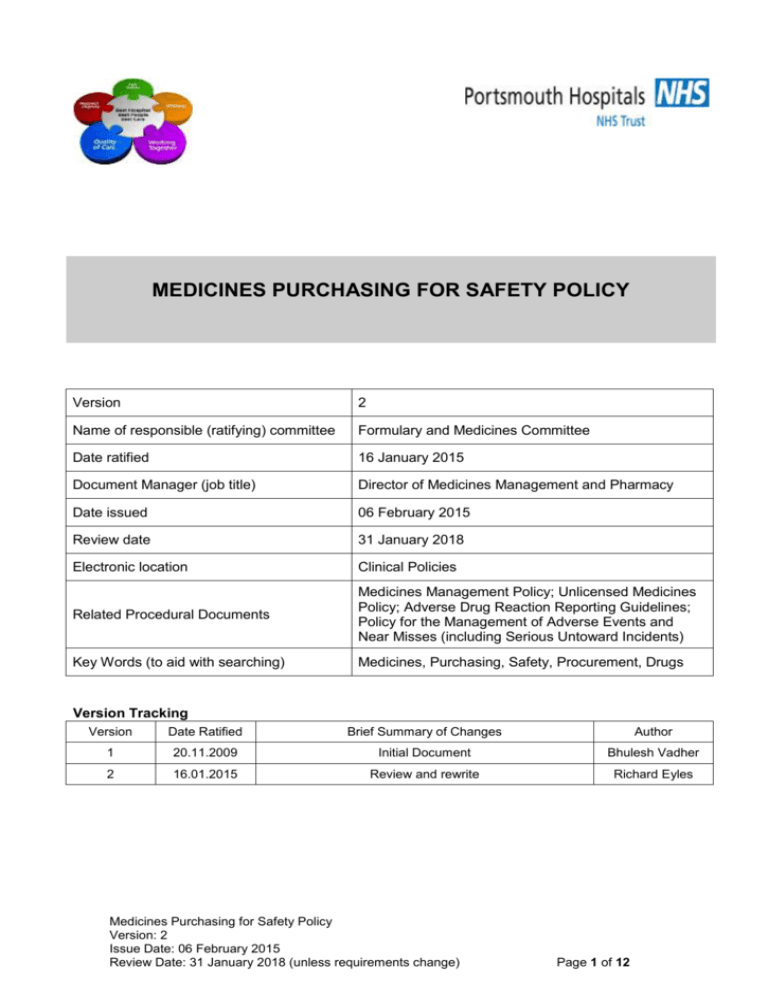
MEDICINES PURCHASING FOR SAFETY POLICY Version 2 Name of responsible (ratifying) committee Formulary and Medicines Committee Date ratified 16 January 2015 Document Manager (job title) Director of Medicines Management and Pharmacy Date issued 06 February 2015 Review date 31 January 2018 Electronic location Clinical Policies Related Procedural Documents Medicines Management Policy; Unlicensed Medicines Policy; Adverse Drug Reaction Reporting Guidelines; Policy for the Management of Adverse Events and Near Misses (including Serious Untoward Incidents) Key Words (to aid with searching) Medicines, Purchasing, Safety, Procurement, Drugs Version Tracking Version Date Ratified Brief Summary of Changes Author 1 20.11.2009 Initial Document Bhulesh Vadher 2 16.01.2015 Review and rewrite Richard Eyles Medicines Purchasing for Safety Policy Version: 2 Issue Date: 06 February 2015 Review Date: 31 January 2018 (unless requirements change) Page 1 of 12 CONTENTS QUICK REFERENCE GUIDE ............................................................................................................. 3 INTRODUCTION ................................................................................................................................ 4 PURPOSE .......................................................................................................................................... 4 SCOPE ............................................................................................................................................... 4 DEFINITIONS ..................................................................................................................................... 4 DUTIES AND RESPONSIBILITIES ..................................................................................................... 6 PROCESS .......................................................................................................................................... 7 MEDICATION ERROR / RISK REPORTING SYSTEM ....................................................................... 8 TRAINING REQUIREMENTS ............................................................................................................. 8 REFERENCES AND ASSOCIATED DOCUMENTATION ................................................................... 8 EQUALITY IMPACT STATEMENT ..................................................................................................... 9 MONITORING .................................................................................................................................. 10 APPENDIX 1 - MEDICINE ERROR, INCIDENT AND DEFECT REPORTING SYSTEMS ................. 11 APPENDIX 2 - PURCHASING OPIOID MEDICINES FOR SAFETY ................................................. 12 Medicines Purchasing for Safety Policy Version: 2 Issue Date: 06 February 2015 Review Date: 31 January 2018 (unless requirements change) Page 2 of 12 QUICK REFERENCE GUIDE For quick reference the guide below is a summary of actions required. This does not negate the need for the document author and others involved in the process to be aware of and follow the detail of this policy. 1. PHT will endeavor to purchase licenced products rather than unlicenced alternatives as the first choice to treat patients 2. If possible medicines will be purchased using a CMU or Regional contract. 3. Where possible all contracted medicines will be assigned a MEPA score by QA specialists 4. All purchases of medicines must be from an approved pharmaceutical supplier 5. Products purchased will be reviewed in light of any incidents reported where the product itself was a contributory factor. 6. Use of unlicensed products will be reviewed annually to assess the appropriateness of their use and the existence of satisfactory licenced alternatives. Medicines Purchasing for Safety Policy Version: 2 Issue Date: 06 February 2015 Review Date: 31 January 2018 (unless requirements change) Page 3 of 12 1. INTRODUCTION The use of all medicines may not only incur a risk of an adverse drug reaction (ADR) but also of a clinical incident such as an inappropriate reconstitution or administration error. These types of medication error risks can and should be minimised by “Purchasing for Safety” in the first instance. All NHS pharmacy staff assume a duty of care when supplying a medicine. In order to reduce the number/frequency of incidents caused by medication errors it is essential that all risks are identified and assessed. Following risk identification and assessment action must be taken to minimise the possibility of a patient safety incident Effective procurement of the right medicine is an important tool in the risk reduction process. This includes Clinical Pharmacists not only assessing a product's clinical effectiveness and ADR potential but also it's safety in use when responding to a request for a new medicine. Medicines should only be purchased if they are of a suitable quality, safe to use and fit for purpose. Moreover it is essential that the procurement process assesses the capabilities of the supply chain to the hospital to ensure that products are genuine, have been correctly stored and are available when required. 2. PURPOSE The purpose of this policy is to provide a consistent trust-wide approach to the safe and timely procurement of medicines including opioids (as a result of NPSA 2008 RRR05 Reducing Dosing Errors with Opioids – see Appendix 2) and any subsequent alerts which include specific Purchasing for Safety guidance which ensures the timely provision of medication and that relevant legislation and government guidance is adhered to. 3. SCOPE This policy applies to all medicines purchased for Portsmouth Hospitals NHS Trust and all staff involved in medicines management from the decision to purchase to the point of administration. ‘In the event of an infection outbreak, flu pandemic or major incident, the Trust recognises that it may not be possible to adhere to all aspects of this document. In such circumstances, staff should take advice from their manager and all possible action must be taken to maintain ongoing patient and staff safety’ 4. DEFINITIONS Adverse Drug Reaction (ADR) Any noxious, undesired, or unintended response to a drug, which occurs at dosages used for prophylaxis, diagnosis, therapy, or modification of physiologic functions CE Mark a symbol applied to products to indicate that they conform with relevant EU directives regarding health and safety or environmental protection Commercial Medicines Unit (CMU) Part of the Department of Health responsible for National and Regional contracting for Medicines. Duopoly A situation in which two companies owns all or nearly all of the market for a given type of product or service. Medicines Purchasing for Safety Policy Version: 2 Issue Date: 06 February 2015 Review Date: 31 January 2018 (unless requirements change) Page 4 of 12 Generic Medication A term to identify non-brand name medications. Typically, a generic medication is a pharmaceutical equivalent to a branded medication product and has identical strength, dosage form, and concentration. JAC The PHT Pharmacy Medicines Management and Electronic Prescribing Solution Licensed Medicine Medicinal product for human use, which has been determined by the MHRA to be industrially produced for marketing purposes, have required efficacy, reliability and quality for human use. Medicines legislation (specifically The Medicines for Human Use Regulations 1994/SI 3144) requires that medicinal products are licensed before they are marketed in the UK. Medecator A web-based pharmaceutical e-procurement solution provided by AAH Medication Error Potential Assessment (MEPA) A risk score that reflects a product's suitability for use, based upon a wide number of factors e.g. clarity of labelling, packing, availability of patient information Medicines and Healthcare products Regulatory Agency (MHRA) The UK government agency responsible for ensuring that medicines and medical devices work, and are acceptably safe. Monopoly A situation in which a single company owns all or nearly all of the market for a given type of product or service. National Reporting and Learning System (NRLS) The world’s most comprehensive database of patient safety information, the successor to the National Patient Safety Agency Pharmaceutical Market Support Group (PMSG) An operational sub-committee of the National Pharmaceutical Supply Group Pharmacy Manufacturing Unit (PMU) PHT's MHRA licenced pharmaceutical manufacturing unit based at Farlington Powergate Independent commercial e-procurement software Quality Assurance (QA) A system under which it is ensured that all products and services are of high quality and will satisfy the expectations of patients, carers and health care professionals. Reconstitution The preparation of a drug using a diluent for administration to a patient. Regional Drug Purchasing Centre (RDPC) The PHT Pharmacy Procurement and Distribution Hub The Trust (PHT) Portsmouth Hospitals NHS Trust Unlicensed Medicine A medicinal product not licensed for use with the UK by the MHRA; but may be used by Medicines Purchasing for Safety Policy Version: 2 Issue Date: 06 February 2015 Review Date: 31 January 2018 (unless requirements change) Page 5 of 12 individual patients on the direct personal responsibility of a doctor or dentist registered in the UK. 5. DUTIES AND RESPONSIBILITIES 5.1 Regional and National Quality Control 5.1.1 Assesses contracted products according to an assessment tool developed by the National NHS QA Committee and attributes a MEPA score to each product. All medicines included onto a NHS CMU contract have a product licence or are CE marked. 5.1.2 Will upload product assessments onto the PharmaQC database which is accessible by the Pharmacy Department. 5.2 Pharmaceutical Market Support Group 5.2.1. Ensures that all awards made for CMU contracted lines do not introduce any additional risk into the supply chain. 5.2.2. Utilises supplier performance measurement as undertaken by NHS CMU when adjudicating awards. Where possible, those suppliers who provide not only the highest quality product but also the best price and service are awarded contracts. 5.2.3. Ensures that National guidance such as that from the NRLS and MHRA is taken into consideration at the adjudication stage. 5.2.4. Ensures that market management is delivered by ensuring monopoly or duopoly markets are not created as part of the adjudication process for critical pharmaceutical products. 5.3. Regional Procurement Lead 5.3.1. Is responsible for representing the views of the Wessex & Thames Valley Region at PMSG in relation to preferred suppliers for generic awards. 5.3.2. Leads tenders for the region for products not covered by CMU contracts. 5.3.3. Feeds back concerns and general procurement issues from the region's members to relevant National committees. 5.4. Formulary and Medicines Committee 5.4.1. Is the ratification forum for this policy and is responsible for ensuring that the safety considerations are taken into account for any new product requests. 5.4.2. Provides feedback to the author of the document. If amendments are required these must be completed and the document re-submitted to the Committee. 5.5. Director of Medicines Management and Pharmacy 5.5.1. Has responsibility for ensuring processes are in place to support this policy 5.5.2. Will ensure that all the medicines management systems in the Trust are efficient and robust. 5.5.3. Will ensure that systems to reduce the risk of medication errors are built into medicine management processes and so safety will occur as a matter of course. Medicines Purchasing for Safety Policy Version: 2 Issue Date: 06 February 2015 Review Date: 31 January 2018 (unless requirements change) Page 6 of 12 5.5.4. Will ensure that National best practice will be utilised to develop systems to limit the risk of medication errors. 5.6. Clinical Pharmacists 5.6.1. Will ensure that the appropriate level of clinical/pharmaceutical scrutiny is carried out when presented with a request to provide a new drug for a patient. 5.7. The Pharmacy Department Procurement Lead 5.7.1. Will endeavour to purchase licenced products rather than unlicenced alternatives as the first choice to treat patients. 5.7.2. Will ensure that where feasible that all orders for pharmaceuticals are placed for lines contracted by NHS CMU or Regional Contracts where available. 5.7.3. Will ensure that where feasible ‘ready to use’ products are purchased. 5.7.4. Will report products which are deemed not suitable for use within the Trust to CMU. 5.7.5. When purchasing generic products off-contract, will obtain as first line, products assessed by QA and listed on the PharmaQC database as suitable alternatives. Where overlabelled or pack-down products are required this work will be placed with PHT PMU. Where PMU is unable to undertake this work e.g. due to capacity or capability issues, the requesting pharmacist will undertake a risk assessment exercise in conjunction with the Pharmacy Risk Team to consider alternatives e.g. other drugs, dispensary pack-down etc. 6. PROCESS 6.1. All purchases for medicinal products will be made from trusted sources of supply to ensure the suitability of products purchased and minimise the possibility of counterfeit medicines. 6.2. Suppliers and wholesalers are required to hold an appropriate licence from the MHRA and this will be checked for authenticity by the pharmacy procurement staff. 6.3. The government holds a list of inspected suppliers who hold or have successfully held a public sector contract; this data base (SID) is held on their website at https://sid4gov.cabinetoffice.gov.uk/. This may be utilised by the pharmacy procurement staff to check the status of any new suppliers prior to including the supplier onto the pharmacy system. 6.4. Any concerns with a supplier will be raised with CMU and if deemed necessary audit reports undertaken to access the supplier performance. 6.5. Safe and secure methods of procurement (e.g. e-procurement via Powergate/Medecator) should be utilised to minimise the potential for error during the process. Telephone orders should be used as a last resort or in an emergency. The trading status of suppliers not set up on JAC to trade electronically should be reviewed annually. Suppliers should only be moved to e-procurement if they can show that the chosen method feeds directly into their stock control system and therefore eliminates re-keying errors. 6.6. New products, including unlicenced manufactured products and unlicenced imports, should be entered on JAC by the Pharmacy IT Team upon receipt of an appropriately completed form to ensure that all products are described to the same standards. Medicines Purchasing for Safety Policy Version: 2 Issue Date: 06 February 2015 Review Date: 31 January 2018 (unless requirements change) Page 7 of 12 7. MEDICATION ERROR / RISK REPORTING SYSTEM 7.1. Systems for reporting patient safety incidents and defects in medicine and medical devices will integrate with the Trust clinical governance reporting streams. 7.2. External reporting schemes as outlined in Appendix 1 will be actioned where relevant by pharmacy staff. 8. TRAINING REQUIREMENTS Training of staff will occur at induction, and during appropriate update training. On-call pharmacists will be trained prior to commencing their on-call duties. A copy of this policy should also be available to consult if guidance is needed 9. REFERENCES AND ASSOCIATED DOCUMENTATION Alert 20. Safer Practice with injectable medicines. 2007. National Patient Safety Agency http://www.nrls.npsa.nhs.uk/resources/?entryid45=59812 Reducing Dosing Errors with Opioids 2008 National Patient Safety Agency http://www.nrls.npsa.nhs.uk/resources/?entryid45=59888 Ensuring safer practice with high dose ampoules of diamorphine and morphine - Safer Pratice Notice 2006 National Patient Safety Agency http://www.nrls.npsa.nhs.uk/resources/?entryid45=59803 Pharmaceutical Market Support Group (PMSG) http://nww.cmu.nhs.uk/Medicines/Strategicgroups/pages/PharmaceuticalMarketSupportGroup. aspx Quality Assurance And Risk Assessment Of Licensed Medicines For The NHS NHS Pharmaceutical Quality Assurance Committee http://www.qcnw.nhs.uk/docs/QA%20&%20Risk%20Assessment%20of%20licensed%20Medici nes%20for%20the%20NHS.pdf PharmaQC Database http://nww.cmu.nhs.uk/Medicines/pharmaQCdatabase/LandingPage.htm Purchasing for Safety Project: Injectable Medicines CMU http://nww.cmu.nhs.uk/Purchasingforsafetyinjectablemedicines/Pages/LandingPage.aspx Duthie Report Royal Pharmaceutical Society http://www.rpharms.com/supportpdfs/safsechandmeds.pdf Medicines Management Policy PHT http://www.porthosp.nhs.uk/Downloads/Policies-AndGuidelines/Clinical-Policies/Medicines_Management.doc Adverse Drug Reaction – Drug Therapy Guideline PHT http://pht/Departments/Pharmacy/Drug%20Therapy%20guidelines/Adverse%20Drug%20Reacti on%20Reporting.doc Policy for the Management of Adverse Events and Near Misses PHT http://www.porthosp.nhs.uk/Downloads/Policies-And-Guidelines/ManagementPolicies/Adverse_Incidents_and_Near_Misses_Management_Policy.doc Medicines Purchasing for Safety Policy Version: 2 Issue Date: 06 February 2015 Review Date: 31 January 2018 (unless requirements change) Page 8 of 12 10. EQUALITY IMPACT STATEMENT Portsmouth Hospitals NHS Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds. This policy has been assessed accordingly Our values are the core of what Portsmouth Hospitals NHS Trust is and what we cherish. They are beliefs that manifest in the behaviours our employees display in the workplace. Our Values were developed after listening to our staff. They bring the Trust closer to its vision to be the best hospital, providing the best care by the best people and ensure that our patients are at the centre of all we do. We are committed to promoting a culture founded on these values which form the ‘heart’ of our Trust: Respect and dignity Quality of care Working together No waste This policy should be read and implemented with the Trust Values in mind at all times. Medicines Purchasing for Safety Policy Version: 2 Issue Date: 06 February 2015 Review Date: 31 January 2018 (unless requirements change) Page 9 of 12 11. MONITORING COMPLIANCE This document will be monitored to ensure it is effective and to assurance compliance. Minimum requirement to be monitored Lead Tool Frequency of Report of Compliance Suppliers have the appropriate MHRA licence to supply medicines Specialist Pharmacist IT & Procurement Website Annual Supplier electronic trading status reviewed for appropriateness Specialist Pharmacist IT & Procurement Medecator & Powergate Annual Medication Errors related to issues identified in this policy Risk Pharmacist Datix Annual Unlicenced Products Review Risk Pharmacist JAC Reporting arrangements Lead(s) for acting on Recommendations Policy audit report to: Specialist Pharmacist IT & Procurement Pharmacy Procurement Operations Manager Director of Medicines Management and Pharmacy Policy audit report to: Director of Medicines Management and Pharmacy Policy audit report to: Director of Medicines Management and Pharmacy Medicines Purchasing for Safety Policy Version: 2 Issue Date: 06 February 2015 Review Date: 31 January 2018 (unless requirements change) Annual Policy audit report to: Director of Medicines Management and Pharmacy Page 10 of 12 Pharmacy Procurement Operations Manager Specialist Pharmacist IT & Procurement Pharmacy Procurement Operations Manager Clinical Pharmacy Leads APPENDIX 1 - MEDICINE ERROR, INCIDENT AND DEFECT REPORTING SYSTEMS What systems are there and when to use them When to Use Reporting System MHRA Defective Medicines Reporting Centre Suspected or actual product defect where patient safety clearly at risk. Guidance from the MHRA here http://www.mhra.gov.uk/home/group s/islic/documents/publication/con00757 2.pdf Examples (not exhaustive list) Serious unexpected reaction. Severe, visible microbial or particulate contamination. Suspected counterfeit product Report Sent To Contact Information MHRA Defective Medicines Reporting Centre Telephone: 020 3080 6574 (08:45 - 16:45 weekdays) 07795 641532 for urgent calls outside of normal working hours, at weekends or on public holidays. Email: dmrc@mhra.gsi.gov.uk Quality Assurance Defect Reporting Scheme Product defects which are quality assurance in nature, with no immediate severe risk to patient safety. Defects reported to the MHRA should also be copied to CMU for contract lines ProMS (Potential Risk of Medication Selection) Incidents where products have been selected or supplied incorrectly, where issues relating to packaging design and presentation are felt to be contributory factors. CMU Issues relating to supply of medications purchased through CMU contracts. Empty blister in strip. Missing batch number or expiry date, particulate contamination. Defective unlicenced medicines should also be reported. Selection of lookalike and sound-alike drugs. Manufacturer's packaging has poor differentiation between different products or strengths. Change in manufacturer of product supplied. Financial and contractual issues. Medicines Purchasing for Safety Policy Version: 2 Issue Date: 06 February 2015 Review Date: 31 January 2018 (unless requirements change) Inform manufacturer. If necessary send sample to an NHS Regional QA service Send to an NHS Regional QA Service As for minor defects above. Relevant CMU buyer for Trust concerned. See contact details for individual buyers. https://www.gov.uk/gov ernment/collections/co mmercial-medicinesunit-cmu In addition these must be reported via the Trust Incident Reporting process via Datix Page 11 of 12 APPENDIX 2 - PURCHASING OPIOID MEDICINES FOR SAFETY Introduction This procedure for purchasing opioids safely is based on the NPSA Safer Practice Notice 12 “Ensuring safer practice with high dose ampoules of diamorphine and morphine” and NPSA/2008/RRR05 “Reducing dosing Errors with Opioid Medicines” This procedure covers the procurement of: Buprenorphine,diamorphine, dipipanone, fentanyl, morphine, oxycodone, papaveretum and pethidine hydromorphone, meptazinol, methadone, Procedure There are significant and potentially fatal risks associated with the procurement, prescribing, supply and administration of opioid medicines, particularly when there are: a) b) c) d) e) different concentrations of an opioid e.g. injections, oral solutions e.g. Oramorph oral solution 10mg/5ml and 100mg/5ml different brands of the same opioid e.g. MST and Zomorph different formulations of an opioid e.g. once a day or twice a day controlled release morphine preparations e.g. MST and MXL similar packaging of different strengths or concentrations of the same opioid similar names of the same opioid e.g. Oxynorm and Oxycontin For these reasons the following steps are taken to ensure safe procurement of opioid medicines: 1. The procurement of the majority of opioids for the Trust is driven by NHS CMU via Regional or National contracts. Contracts for opioids are awarded following advice from Quality Control and senior pharmacy representatives from all Trusts at adjudication meetings. Locally the representative for PHT is the RDPC Operations Manager. 2. a) b) Contracts for opioids are awarded taking into account the following criteria: the quality and clarity of labelling and packaging presentation and appropriateness to clinical practice e.g. ampoules, vials or pre-filled syringes c) d) e) bio-equivalence between different brands supplier performance cost 3. The impact of the awarding of these contacts on PHT is assessed by the Specialist Pharmacist for IT & Procurement. 4. Responsibility for the procurement of opioids outside of CMU contracts rests with the Specialist Pharmacist for IT & Procurement or the Chief Pharmacist. 5. If there are communication or clinical safety issues to consider due to a change in contract or the requirement to purchase off-contract then these are either referred to the Area Prescribing Committee or Medicines Safety Committee, as appropriate 6. The range of epidural opioid/local anaesthetic infusion products procured by pharmacy is agreed by the Clinical Director of Anaesthetics and ratified by Medicines Safety Committee. 7. All requests for new opioids or new presentations of existing opioids must be made via the Area Prescribing Committee following the New Drugs Application procedure Medicines Purchasing for Safety Policy Version: 2 Issue Date: 06 February 2015 Review Date: 31 January 2018 (unless requirements change) Page 12 of 12