Test:
advertisement

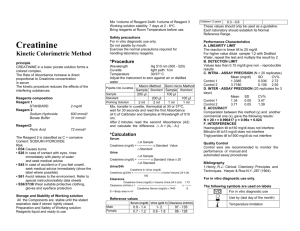
C604 Pathology Course – Useful Renal Pathology Tests –Phillips, Carrie 1. Serum creatinine (renal function test) a. Elevations may reflect a substantial decline in renal function. b. Reported as mg/dL c. Production: i. Creatinine is produced in muscle from creatine non-enzymatically ii. ~2% of total body creatine is converted to creatinine daily d. Excretion: determined by renal function since creatinine is not further metabolized e. Used as a broad-based screening test for any reduction in renal function. An elevation above baseline creatinine is believed to be sensitive for a reduction in glomerular filtration, but with a low specificity for any particular etiology f. Provides a rough estimate of GFR by using the following MDRD (Modification of Diet in Renal Disease) equation: IDMS (isotope-dilution mass spectrometry)-traceable method: GFR (mL/min/1.73 m2) =175*(Serum Cr) ^ (-1.154) * (age in years) ^ (-0.203) * (0.742 if female) * (1.212 if African American) Where Serum Cr is serum/plasma creatinine in mg/dL measured by an IDMS-traceable enzymatic creatinine method. Creatinine Clearance: Cockcroft-Gault (CG) equation: GFR (mL/min/1.73 m2) = [(140-age in years) / (Serum Cr)] * (weight in kg/72) * (0.85 if female) The CG equation is often used by pharmacologists for drug dosing. Much of the research on drug clearance was performed before the MDRD equation was developed. There are other equations that include cystatin C, which are not in wide use yet. Testing for cystatin C is very expensive; testing for creatinine is very cheap. In children, there is not a single formula recommended for all ages. However, the Schwartz formula is frequently used and appropriate for most ages, but should be used with caution or avoided in premature infants in the first several months of life. In the premature infant population, more specialized equations are often used. The pediatric Schwartz equation: GFR (mL/min/1.73 m2) = (0.413 * Height in cm) / (serum Cr) Formulas are not accurate in acute renal failure or early stage kidney disease. g. If interpreted strictly within a reference range, the test is relatively insensitive for small decrements in renal function. However, the test is highly sensitive for changes in renal function with respect to the patient's baseline creatinine. 2. Blood Urea Nitrogen (renal function test) a. Detection of nitrogen-rich urea in blood (the major product of protein catabolism) b. Reported as mg/dL c. Azotemia is an abnormal amount of urea in blood. d. Most urea is produced in the liver and excreted by the kidney. Urea is freely filtered by glomeruli and passively diffuses through tubules into interstitium. Urea is not actively secreted or reabsorbed by tubules. Back-diffusion of urea is inversely proportional to urine flow rate. e. In conjunction with serum creatinine, BUN provides a rough estimate of glomerular filtration rate because urea levels fluctuate with dietary protein intake, hepatic dysfunction, hypercatabolic states (infection, hyperthermia, steroid therapy), and tubular reabsorption. Prepared by C. Phillips/M. Zimmerman. For more information, go to the IU Health Laboratory Portal: https://www.iuhealth.net/portal/pathlab C604 Pathology Course – Useful Renal Pathology Tests –Phillips, Carrie f. If interpreted strictly within a reference range, the test is relatively insensitive for small decrements in renal function. However, the test is highly sensitive for changes in renal function with respect to the patient's baseline BUN. g. BUN:serum creatinine ratio < 15:1 is normal; ratio >20:1 indicates intravascular volume depletion (hypovolemia) 3. Urine dipstick or reagent strip (a variety of absorbent pads attached to a plastic strip) a. “Point of care” testing with visual interpretation or automated detection by laboratory (with or without microscopy) b. Exposure of urine to pads on test strip results in potential detection of nitrites, pH, protein (particularly albuminuria), leukocytes (pyuria), blood (hematuria), glucose (glucosuria), ketone bodies, urobilinogen, bilirubin and/or specific gravity c. Does not distinguish myoglobin from hemoglobin d. Not a reliable method to detect Bence-Jones proteins (kappa and lambda immunoglobulin light chains) e. Requires confirmation by urine microscopy if blood is detected 4. Urine microscopy a. A drop of centrifuged urine sediment (pellet) is placed on a glass slide and examined by light microscopy for possible cellular elements (leukocytes, erythrocytes and epithelial cells), casts, crystals or infectious organisms such as bacteria. b. Hematuria: red blood cells (RBCs) in urine i. RBCs lack nuclei and normally have a smooth, biconcave shape. ii. RBC casts are molded in the tubules of the nephrons and implicate the glomerulus as the origin of hematuria (excludes lower urinary tract bleeding, e.g., bladder or prostate). iii. Presence of dysmorphic RBCs implicates glomerulus as the source of hematuria c. Granular casts: Sloughed necrotic tubular epithelial cells are shed into the urine as free epithelial cells, or molded into cellular or coarse granular casts (e.g., “muddy brown casts” are seen in acute tubular necrosis). d. Pyuria: white blood cells (WBCs) in urine indicate inflammation of the urinary tract and infection should be ruled out. WBC casts originate in renal tubules. 5. 24 hour timed urine collection for protein (or albumin) quantification (to confirm and quantify urine dipstick). If creatinine is also measured in the same specimen, this permits an estimate of the accuracy of urine collection. Measurement of total protein in urine is standardized for albumin. 6. Random Urine Albumin (or Protein):Creatinine Ratio (spot urinary protein/creatinine ratio) a. Measured in a single “spot” urine specimen b. Reliable reflection of 24 hour excretion rate of albumin c. Protein:creatinine ratio of > 3.5 is suggestive of nephrotic range proteinuria. A ratio of < 0.2 is suggestive of normal protein excretion 7. Plasma or Serum Albumin a. Low in nephrotic syndrome due to massive loss of albumin in urine. Some people with nephrotic range proteinuria may have normal serum levels. b. Profoundly low is <2 mg/dL. c. Increase in albumin during the course of disease often indicates remission, improvement in proteinuria, or response to therapy. 8. Cholesterol and triglycerides a. Elevated in nephrotic syndrome due to increased hepatic production b. Patients with nephrotic syndrome require lipid monitoring and often, pharmacological therapy. Prepared by C. Phillips/M. Zimmerman. For more information, go to the IU Health Laboratory Portal: https://www.iuhealth.net/portal/pathlab C604 Pathology Course – Useful Renal Pathology Tests –Phillips, Carrie 9. Others: glucose, serum electrolytes (Na+, K+, CO2, Cl-) 10. Tests used to help diagnose and monitor multiple myeloma. a. Serum protein electrophoresis (SPEP) and urine protein electrophoresis (UPEP) are laboratory tests that examine proteins in the blood and urine. The proteins are separated into five major fractions by electrical charge: serum albumin, alpha-1 globulins, alpha-2 globulins, beta globulins, and gamma globulins. In most people with multiple myeloma, large amounts of an abnormal immunoglobulin protein (M-protein) will show up as a large band on the electrophoresis gel usually in gamma region, though it may migrate in other regions. b. Immunofixation electrophoresis is done to identify the specific type of monoclonal protein that is being produced by the malignant plasma cells, typically the heavy chains IgG, IgM, IgA and light chains Kappa and Lambda are evaluated. IgD and IgE can also be assessed, if needed. Prepared by C. Phillips/M. Zimmerman. For more information, go to the IU Health Laboratory Portal: https://www.iuhealth.net/portal/pathlab