TEMPLATE FOR POSITION PAPER
advertisement
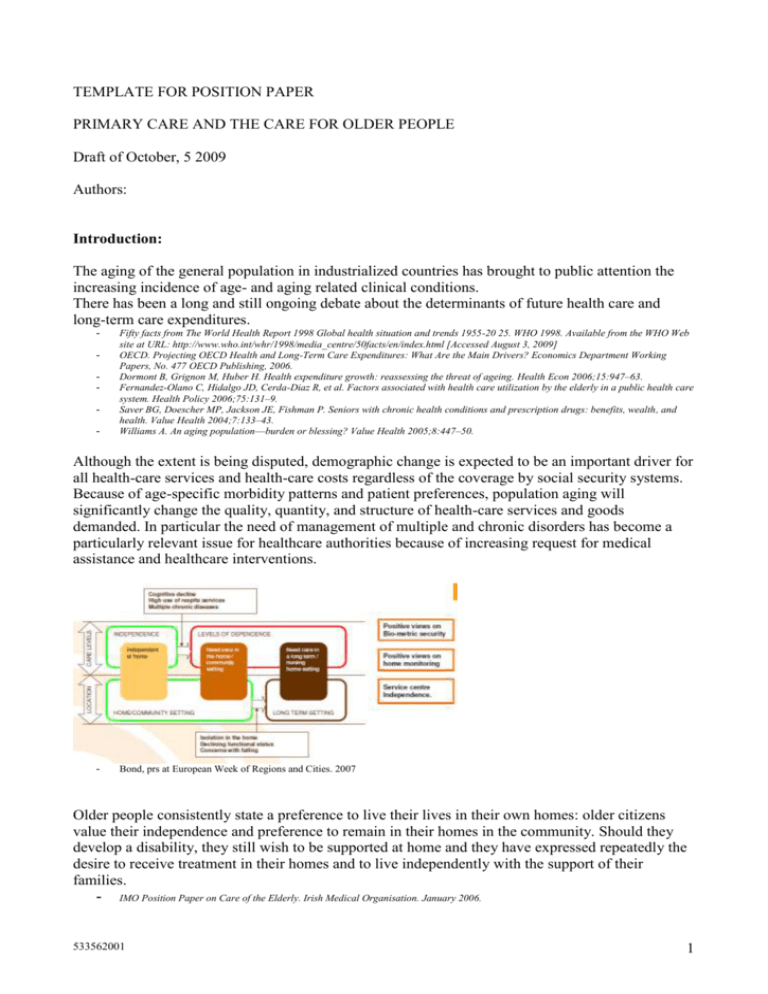
TEMPLATE FOR POSITION PAPER PRIMARY CARE AND THE CARE FOR OLDER PEOPLE Draft of October, 5 2009 Authors: Introduction: The aging of the general population in industrialized countries has brought to public attention the increasing incidence of age- and aging related clinical conditions. There has been a long and still ongoing debate about the determinants of future health care and long-term care expenditures. - Fifty facts from The World Health Report 1998 Global health situation and trends 1955-20 25. WHO 1998. Available from the WHO Web site at URL: http://www.who.int/whr/1998/media_centre/50facts/en/index.html [Accessed August 3, 2009] OECD. Projecting OECD Health and Long-Term Care Expenditures: What Are the Main Drivers? Economics Department Working Papers, No. 477 OECD Publishing, 2006. Dormont B, Grignon M, Huber H. Health expenditure growth: reassessing the threat of ageing. Health Econ 2006;15:947–63. Fernandez-Olano C, Hidalgo JD, Cerda-Diaz R, et al. Factors associated with health care utilization by the elderly in a public health care system. Health Policy 2006;75:131–9. Saver BG, Doescher MP, Jackson JE, Fishman P. Seniors with chronic health conditions and prescription drugs: benefits, wealth, and health. Value Health 2004;7:133–43. Williams A. An aging population––burden or blessing? Value Health 2005;8:447–50. Although the extent is being disputed, demographic change is expected to be an important driver for all health-care services and health-care costs regardless of the coverage by social security systems. Because of age-specific morbidity patterns and patient preferences, population aging will significantly change the quality, quantity, and structure of health-care services and goods demanded. In particular the need of management of multiple and chronic disorders has become a particularly relevant issue for healthcare authorities because of increasing request for medical assistance and healthcare interventions. - Bond, prs at European Week of Regions and Cities. 2007 Older people consistently state a preference to live their lives in their own homes: older citizens value their independence and preference to remain in their homes in the community. Should they develop a disability, they still wish to be supported at home and they have expressed repeatedly the desire to receive treatment in their homes and to live independently with the support of their families. - IMO Position Paper on Care of the Elderly. Irish Medical Organisation. January 2006. 533562001 1 But, also, informal care (cheapest) would be likely to decline in all the countries as a result of a downward trend in co-residence of older people with their children, an upward trend in older people living alone, a decline in female care-giving potential and rising female employment rates. Reduction in informal care would generate greater demand for formal care, thereby inflating healthcare and long term care expenditures. An emerging European trend exists in attempting to reduce the rise in the level of institutionallybased care (residential and nursing home care) whilst promoting care provided at home or home environment in a primary care setting, where General Practitioner (GP) has a key leadership role in the delivery of care to the older people: as stated 50%+ of older people visit their General Practitioner regularly. To meet the primary care needs of the aging population, it’s important that not only GP but also researchers and policy makers do understand, evaluate and respond to this phenomenon. The focus of the present Position Paper would address key themes for primary healthcare provided to older people by GP (or Family Doctor – FD) and by non medical professionals (such as care provided by nurses) within the community and would discuss policy issues which may raise in this area. This document will not include the discussion of care for older people in nursing homes or secondary care provided in hospitals. The social care system level will be also not discussed in this paper. Terms and Definitions: OLDER PEOPLE Subjects 65 years or older, who cannot be managed as younger people even when “in good health”. The concept of grading the definition of older people would be introduced by defining the vulnerable subjects then the frail individuals/frailty until complex conditions where the subject cannot be managed at home and requires e.g. institutionalization, secondary care, etc PRIMARY CARE: In order to describe the primary care setting, various definitions have been considered. As examples: 533562001 2 - - - - Primary care is the provision of integrated, accessible healthcare services by clinicians who are responsible for addressing a large majority of personal healthcare needs, developing a sustained partnership with patients, and practicing in the context of family and community (Vanselow 1995) Primary care is the setting within a healthcare system, usually in the patient’s own community, in which the first contact with a health professional occurs (excluding major trauma or emergencies) (WONCA 2002), encounters related to services and treatment of illnesses/conditions and/or preventive and health promotion activities. There are many different healthcare providers working in primary care. Primary care as first contact care, accessible by all, guaranteeing a sustained and trustworthy partnership between providers and patients, comprehensive, coordinated care for a predetermined population, activated by patient choice, plays an essential role in improving health care systems altogether (Goodwin, presentation at The Future of Primary Health Care in Europe II, University of Southampton, UK, 17th September 2008) Others refs. for definitions The primary care setting would be considered as the initial point of contact which integrates into healthcare system – as a sort of focal point – and outside the healthcare system towards the social care interventions. Demographics: Because of changes in fertility and mortality rates during the 20th century, demographic structure in industrialised countries will change substantially within the coming decades. In Europe, for example, the population of the present 27 countries is projected to become older with the median age projected to rise from 40.4 years in 2008 to 47.9 years in 2060. The share of people aged 65 years or over in the total population is projected to increase from 17.1% to 30.0% and the number is projected to rise from 84.6 million in 2008 to 151.5 million in 2060. The number of people aged 80 years or over is projected to almost triple from 21.8 million in 2008 to 61.4 million in 2060, underlining the importance of the advanced elderly among senior citizens. Similarly, the US is an ageing society: between 2000 and 2050, the number of older people is projected to increase by 135%. Moreover, the population aged 85 and over is projected to increase by 350%. Over this time period, the proportion of the population that is over the age of 65 will increase from 12.7% in 2000 to 20.3% in 2050; the proportion of the population that is age 85 and older will increase from 1.6% in 2000 to 4.8% in 2050. - - Eurostat, Statistics in Focus, 72/2008 "Ageing characterises the demographic perspectives of the European societies". Available from the Eurostat Web site at URL: http://epp.eurostat.ec.europa.eu/cache/ITY_OFFPUB/KS-SF-08-072/EN/KS-SF-08-072-EN.PDF [Accessed August 3, 2009] Wiener JM and Tilly J. Population ageing in the United States of America: implications for public programmes. International Journal of Epidemiology 2002;31:776-781 Discussion of refs. for demographics and census The influx of older patients into the office-based primary care setting is a demographic reality for most General Practices (GP) and older patients are representing an increasing proportion of the caseload of general practitioners into the future: as the rapid ageing of the population continues, healthcare providers, in general, and GP will be called upon to provide primary care to an increasing volume of older patients. - Discussion of refs. for GP access data European Scenario: Short description on how the different European countries currently approach the primary care process given by GPs towards aging people - Literature review Sharing of experiences/best practices as examples 533562001 3 Addressing the key themes for care of older people in the primary care setting: Comprehensive assessment of older people in primary care Aging people present some particular challenges to GPs. Even when manageable in the primary care setting, the older patients often have multiple illnesses with associated disability and dependence on others. Assessment of medical problems in isolation, without consideration of patient functional abilities, cognitive aspects and their interaction with family members and their living environment, may yield suboptimal results. Yet comprehensive assessment is difficult to achieve in traditional office practice - considering also that many older people struggle to visit the office – but many evidences show the role of comprehensive assessment (using different tools in different settings) in the management of older patients.. - Literature review for selected assessment tools relevant in “primary care and older/aging people” Providing preventive services for a healthy aging/lifestyle - Targeting common risk factors: smoking, physical inactivity and unhealthy nutrition, … Controlling (cardiovascular) risk factors Health promotion interventions in later life require a different focus than those at younger ages, with an emphasis on reducing age-associated morbidity and disability and the effects of cumulative disease co-morbidities. Primary care practitioners should have the opportunities to alter risky behaviours. Lack of time and skills are key barriers. Since the common risk factors, smoking, physical inactivity and unhealthy diet are risk factors that contribute to most of the health conditions among older adults, modifying these and keeping healthy lifestyles are key components of good health practice in older age. - Age-friendly Primary Health Care Centres Toolkit. WHO. 2008 Key clinical management approaches Older people often have multiple complex health and social conditions and may also present with vague complaints such as dizziness. These intertwining symptoms are difficult to diagnose and treat in the limited time available at most primary care settings. Many of these conditions are chronic and must be screened, early detected and managed to prevent avoidable complications and disability. As the population ages, an increasing number of older patients is presenting with multiple medical problems and multiple prescribed medications inducing a relevant burden and associated costs for inappropriate prescribing, lack of adherence and compliance, adverse drug events. It is not possible to include all geriatric assessment and treatment approaches in this paper, which therefore has a focus on: - memory loss/dementia - depression - chronic pain - geriatric syndromes (incontinence, falls) - diagnosis and key management of hypertension and diabetes (as the two major chronic diseases which account for a high portion of illness and disability) - medications use 533562001 4 Conclusions: Presenting “experiences” and lessons learned and the conditions (policies) under which they can function Recommending structured health comprehensive assessment in Primary Care Recommending policy measures Recommending research activities to fill the gap of knowledge on older/aging condition 533562001 5