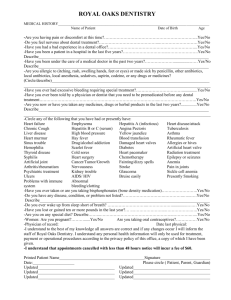
New Patient Health History
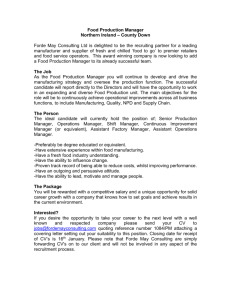
advertisement

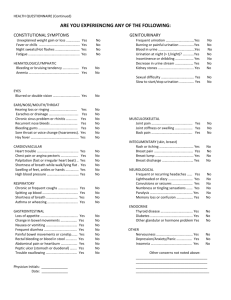
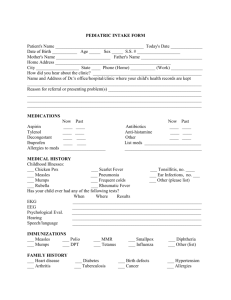
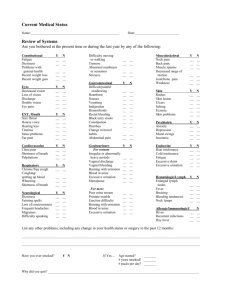
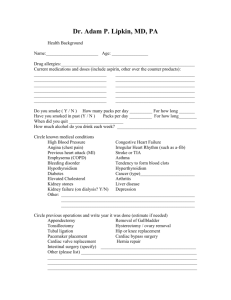
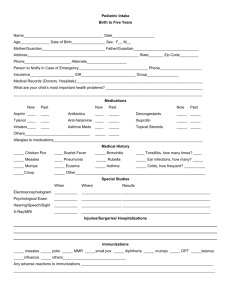
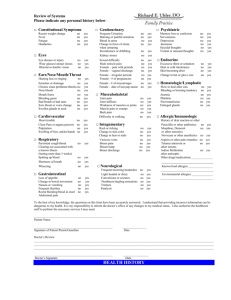
Name________________________ History, New Patient Health History Today’s Date: NAME_____________________________________________ 1 ___/___/______ Date of Birth ____/____/______ Address________________________________________________________________________ Current Phone Number(s) W__________________ H_______________ C_________________ Single Married Divorced Widowed Partnered // Live Alone__ With Others__ If you have children, please list their ages: ________________________ MEDICATIONS, VITAMINS, NUTRITIONAL SUPPLEMENTS List name, dose, and number taken each day ____________________________________ _____________________________________ _____________________________________ _____________________________________ ____________________________________ _____________________________________ _____________________________________ _____________________________________- _____________________________________ _____________________________________ _____________________________________ _____________________________________ MEDICATION ALLERGIES or SENSITIVITIES (please describe briefly what happens) ___________________________________________________________________________ _____________________________________________________________________________ _____________________________________________________________________________ OTHER ALLERGIES _____________________________________________________________________________ _____________________________________________________________________________ PAST MEDICAL PROBLEMS/SURGERY/HOSPITALIZATIONS ____________________________________ _____________________________________ _____________________________________ ____________________________________ _____________________________________ _____________________________________ _____________________________________ _____________________________________ _____________________________________ _____________________________________ _____________________________________ _____________________________________ _____________________________________ _____________________________________ Name________________________ History, Have you had : Chicken Pox Y/N Hepatitis Mumps Y/N Measles Y/N Y/N (if yes, what kind?____) When was your last: tetanus booster ____ flu shot____ 2 German Measles Y/N Tuberculosis Y/N pneumovax (pneumonia shot)_____ Have you had immunizations against (when): Measles/mumps/rubella ____ Hepatitis B____ Hepatitis A___ Polio____ FAMILY HISTORY: Problem Which Relative(s) At What Age(s)? Depression________________________________________________________________________ Alchoholism________________________________________________________________________ Other Psychiatric____________________________________________________________________ Melanoma_________________________________________________________________________ Colon Cancer_______________________________________________________________________ Breast Cancer______________________________________________________________________ Ovarian Cancer_____________________________________________________________________ Prostate Cancer_____________________________________________________________________ Heart Attack/Coronary Artery Disease___________________________________________________ Diabetes__________________________________________________________________________ Osteoporosis_______________________________________________________________________ Dementia/Alzheimer’s________________________________________________________________ Other_____________________________________________________________________________ _________________________________________________________________________________ OTHER HISTORY Ever smoked? No Yes If Yes: How many packs/day________ How many years?___________ When did you quit?________ Smoking Currently? No Yes If Yes: How much?________________ Do you drink Alcohol? No Yes If Yes: How many drinks/day (average)___ If Yes: Do you ever think you should cut down? Y Do you ever feel guilty about drinking? Y Do you get annoyed if others criticize your drinking? Y Do you ever drink an “eyeopener”? Y N N N N Name________________________ History, -Have you had sex in the last 3 months? Yes 3 No -How many sexual partners have you had in the last 5 years? _______ -Your sexual partner(s) are/have been -Do you use contraception? Yes / No men____ women____ both_____? If Yes, what?____________________________________ -Have you ever had a sexually transmitted disease? Yes /No If Yes, what?_____________________ -Do you use protection against sexually transmitted disease? Yes/ No -Have you ever used “recreational drugs”? yes/ no -Have you ever had a blood transfusion? Yes/ No -Do you exercise regularly? Yes / No If Yes, what?_____________ If Yes, have you used needles? Yes / No When?________________ If Yes, What and How often?_________________________ -Do you drink 4 8-oz glasses of milk, or the equivalent, daily? Yes / No Do you take calcium? Yes/ No -When did you last see a dentist? _________________ eye doctor?__________________ -Please list the name and specialty of any other health care professionals you see: _____________________________________ _____________________________________ _____________________________________ _____________________________________ _____________________________________ _________________________________ Have you completed a Living Will or other Advance Directive? Yes / No If you were unable for some reason to make medical decisions for yourself, who would you want to make those decisions for you? (for example, if you were unconscious after a bad auto accident, or had had a major stroke) Not Sure_________ (1) Name:___________________________ Relationship to you____________________ Address __________________________________________________ Phone number _________________________ Comments_________________________________________________________ __________________________________________________________________ Is this person aware that s/he would be responsible for decision making under such circumstances? Y/ N Name________________________ History, PLEASE CHECK ANY OF THE FOLLOWING THAT APPLY TO YOU Hayfever__ Decreased Hearing__ Nasal Congestion__ Hypothyroid__ Snoring__ Hyperthyroid__ Nose Bleeds__ glaucoma__ Goiter__ New weight gain___ New weight loss___ Unusual fatigue____ Diabetes___ Cough__ Wheezing__ Asthma__ Shortness of Breath__ Past Pneumonia__ Positive TB Skin Test__ Chest Pains__ Sleep Apnea__ Angina__ Palpitations__ Irregular Heart Beat__ New Fatigue or Shortness of Breath with Exercise__ Fainting__ Lightheadedness__ Leg Swelling__ Heartburn__ Abdominal Pain__ Swallowing difficulty__ Nausea__ Vomiting__ Constipation__ Diarrhea__ Black BM ___ Rectal Bleeding ___ Irritable Bowel__ Inflammatory Bowel Disease__ Gall Bladder Problems__ Stomach bleeding__ Ulcers__ Hepatitis__ Hernia__ Burning or Pain with urination__ Night time urination__ Difficulty urinating__ Incontinence__ Increased Frequency of urination___ Bladder infections__ Kidney stones__ Kidney Infections__ Blood in the Urine__ Joint pain__ Hot/Swollen Joints__ Joint Injury__ Gout__ Osteoarthritis__ Muscle pain__ Fractured Bones__ Osteoporosis__ Clinician’s Notes 4 Name________________________ History, Lyme Disease__ Skin Cancers__ Back Pain__ sciatica__ 5 Clinician’s Notes: Eczema__ Hives__ Acne__ Cold Sores__ Genital Herpes__ Psoriasis__ Headaches__ Numbness or Tingling__ Weakness or paralysis__ History of stroke__ Vision changes__ History of meningitis__ Difficulty walking___ Tremor__ Balance problems___ Unusual Bruising/bleeding__ Blood Clots __ Phlebitis__ Anemia__ Swollen Glands___ Sad Mood__ Difficulty Sleeping__ Anxiousness__ Suicidal Thoughts__ Inability to enjoy activities__ History of Abuse__ History of treatment for emotional problems____ Sexual function concerns___ MEN ONLY Prostatitis__ Discharge from Penis__ Problems with erections__ Pain or lump in testicles/scrotum___ WOMEN ONLY Periods started at (what age)_____ If No, at what age did your periods end? ____ Pregnancies Y/N (How many)____ Have you had a hysterectomy? Live Births Y/N If yes, were your ovaries also removed? Y/N (How many)_____ Abnormal Pap smears? Y/N If yes, when was the last one?______ Y/N If you no longer get periods, skip the following questions. Vaginal spotting __ Last Menstrual Period (when)_____ Abnormal vaginal discharge__ Bleeding between periods ___ Heavy periods ___ Do you still get a period? Y/N Painful periods____ ~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~ Please list any other symptoms or concerns that you want to make us aware of at this visit (if we cannot address them all today, we will arrange to see you again very soon) __________________________________________________________________ ___________________________________________________________________ ___________________________________________________________________ ___________________________________________________________________ ___________________________________________________________________ Name________________________ History, 6