Chapter 17 notes
advertisement

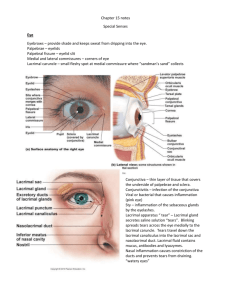
1 Chapter 17 - SPECIAL SENSES Interpretation occurs in Vision, olfactory, auditory (equilibrium), and gustatory are considered the special senses Perceptions of sensory inputs are overlapping, therefore Chemical senses: Taste and Smell GUSTATION (TASTE) Receptors: gustatory hairs (cilia) of taste cells •Taste cells located in taste buds of tongue (most), pharynx, larynx, & soft/hard palate – •Most all taste buds located in lingual papillae (epithelial projections on the tongue) Filiform – do not contain taste buds but help move substances around the mouth Fungiform – small; contain about five taste buds which sit towards the top Circumvallate – larger; contain as many as 100 taste buds, which are in the epithelium of the sidewalls; •Taste bud cells are replaced every 7 to 10 days by •For a chemical to be tasted it must dissolve in saliva, diffuse into the taste pore, contact gustatory hairs - Different gustatory cells have different thresholds for activation 4 basic tastes (sweet, sour, salty, biter) - not spatially distributed -sweet: elicited by organic substances including -sour: produced by acids with a -salty: produced by inorganic salts ( metal ions) such as -bitter: elicited by alkaloids •Two additional tastes have been discovered - Umami and Water receptors - Pleasant tastes of broth and cheese, and yes we can taste water 2 Gustatory (sensory) pathway: •Taste cells coiled by sensory dendrites •afferent fibers (carrying taste info from the tongue) (VII) facial: monitors taste buds (IX) Glossopharyngeal: taste buds (X) Vagus: taste buds on the epiglottis •synapses in Medulla (reflex center for swallowing/vomiting) stream to the thalamus and are then interpreted in the gustatory cortex - triggers reflexes involved with digestion •Sensitivity to tastes differs among individuals and it declines as we age •Taste is intimately associated with olfaction – OLFACTION (SMELL) Receptors: olfactory epithelium located in the roof of the nasal cavity Odorants – small organic molecules that stimulate olfactory receptors •olfactory epithelium contains millions of olfactory receptor cells – •receptor cells are highly modified cells that have a knob that projects past the epithelium – extensions •unmyelinated axons of olfactory receptor cells gathered into fascicles (filaments of olfactory nerve I), project through cribiform plate where they synapse with distal end of the olfactory tracts •we can detect over 2000 chemical smells based on a combination of about 50 primary smells •via Olfactory tracts to either: 1. to olfactory cortex (medial surface of temporal lobe) and part of frontal lobe above orbits 2. to hypothalamus & limbic system where emotional aspects of smell are analyzed and/or responded to 3 •Receptor cells adapt rapidly and therefore need to be turned over – VISION •70% of all sensory receptors of the body are in the eyes A. Accessory Structures: 1. eyebrows: help protect the eye – 2. eyelids (palpebrae): lubricate and clean off surface of the eye - - separated by the palpebrae fissure connected at the medial and lateral canthus eyelashes protect from foreign material o associated with a tarsal gland that secretes a lipid-rich product – keep from sticking lacrimal caruncle at the medial canthus secretes a thick substance that may accumulate during the night a blockage in any of these ducts may produce a localized swelling - 3. Conjunctiva: epithelium covering the inner surface (palpebrae conjunctiva) of the eyelids and outer surface (ocular conjunctiva) of the eye a. Extends over the eye to the cornea where the epithelium thins Conjunctivitis – (pinkeye) 4. Lacrimal apparatus: lacrimal gland and the ducts (lacrimal puncta) that drain excess secretions into the nasal cavity a. Lacrimal secretions: fluid containing mucus, antibodies, and lysozome (attacks bacteria) b. Blinking sweeps this fluid across the eye 5. Extrinsic eye muscles – inferior, medial, superior, & lateral rectus, and superior & inferior oblique B. Structure of the Eye: o The eye sits in the orbit surrounded by the extrinsic muscles, the lacrimal gland, orbital fat, and the cranial nerves and blood vessels that supply the eye and area around it 1. Tunics forming wall of eye 4 a. Fibrous tunic (outermost layer of the eye) composed of Sclera: glistening white dense fibrous connective tissue; o Thickest in the posterior and thinnest in the anterior; extrinsic muscles insert on the sclerea Cornea: regular arrangement of its collagen fibers makes it transparent, forming a clear o The limbus is the border between the two o well supplied w/ nerve endings; o vulnerable to damage – b. Vascular Tunic (middle coat) also called the *3 regions: iris, ciliary body, & choroid • Iris: visible colored part of eye - houses pupil (opening in eye for light to enter) & o papillary dilator and constrictor muscles - iris color determined by the density of melanocytes and density of pigmented epithelium • Ciliary Body: encircles lens posterior to the iris - predominately made up of ciliary muscles (smooth) - pulls on suspensory ligaments which keep the lens • Choroid: provides nutrients to all eye tunics o contains an extensive capillary network and separates the neural tunic and the fibrous tunic posterior to the ora serrata c. Neural Tunic (retina): (innermost tunic) • outer pigmented layer (closest to the choroid) -absorbs light and prevents it from bouncing back producing visual “echoes” • inner neural layer (plays a direct role in vision) -contains 3 main types of neurons: o photoreceptors – cells that detect light (rods and cones) 5 o Rods - highly sensitive to light; allow us to see in poor lighting Mostly span o Cones – require more intense light; provide us with Highly concentrated in the macula lutea and fovea (central area) – center of site where image is projected – o Rods and cones synapse with bipolar cells which in turn synapse with ganglion cells o Horizontal cells and Amacrine cells extend across outer portion between synapses altering the sensitivity of the retina Optic disc (blind spot): site where optic nerve exits the eye and central artery and vein enter the eye o Optic nerve is formed from o There are no photoreceptors this area – continual involuntary eye movements 2. Internal Chambers & Fluids a. Anterior Cavity (anterior to lens) • Anterior segment filled with -formed by the ciliary bodies & drained at -supplies nutrients and removes wastes -creates pressure that stabilizes - intraocular pressure – 12 to 21 mm Hg *Glaucoma – for various reasons, aqueous humor cannot enter the canal of Schlemm. Intraocular pressure builds and leads to disruption of graded potentials b. Posterior cavity (behind lens & is the largest) • filled with vitreous humor (body) – viscous, gelatinous liquid •transmits light •helps to stabilize •also contributes to 6 c. Lens: biconvex, transparent, flexible structure that can change shape •enclosed in •avascular •lens fibers are added throughout life which leads to *Cataract Vision: Stimulus: electromagnetic energy-wave lengths Receptors: photoreceptors (quarter billion) Light/image must pass through the cornea, aqueous humor, pupil, lens, and vitreous body before it reaches the retina Four basic processes must occur for an image to form on the retina 1. Refraction of light rays – light rays will bend when they travel through a medium of different density at the surface 2. Accomodation of the lens – the greater the convex curve, the more the light rays bend toward each other. It can change focusing power by becoming moderately curved or greatly curved Emmetropic eye – sufficiently refract light rays to focus an image on the retina Myopia (nearsightedness) or hyperopia (farsightedness) occur here 3. Constriction of the pupil – narrowing the diameter of the hole through which light enters 4. Convergence – movement of the two eyeballs toward the nose so they are both directed to the object Important, along with binocular vision, for depth perception Remember: visual images are focused upside down and undergo a mirror reversal on the retina Light impulses are converted to nerve impulses on the surface of the retina on the quarter billion photoreceptors found in the neural retina (rods and cones) 7 Photopigments – substance that can absorb light and undergo a change in structure to produce a generator potential Rods: dim light & peripheral vision receptors •contain light sensitive visual pigment (rhodopsin) •rhodopsin:(visual purple) – composed of a protein called opsin and a derivative of Vitamin A called retinal •Rhodopsin absorb light which causes it to break down causing depolarizatioin of rods thereby initiating a visual impulse •have low threshold to light; broken down and replaced at the same rate during night; non-functional during the day because •absent from fovea centralis Cones: receptors for bright light and color • have higher threshold than rods • lateral to blind spot region called macula lutea w/ minute pit in its center called fovea centralis •in this area light is passed almost directly passed to the photoreceptors •fovea contains only cones • •contain 1 of 3 different visual pigments that respond differently to different wavelengths -red cones respond to the highest wavelengths, then green cones, to the lowest blue cones •overlap in their absorption spectra •color blindness: Visual pathway: •photoreceptors to bipolar cells to ganglion cells (cell bodies in neural layer of retina and axons that extend to form optic nerve. •optic chiasma -fibers from medial aspect of each eye cross over to the opposite side Optic tracts: 8 Each optic tract contains a) fibers form lateral aspect of the eye on the same side & fibers from the medial aspect of the opposite eye, and b) carryall the same information from the same half of the visual field. -carry these impulses to the Thalamus which organizes information Interpretation: visual cortex (occipital lobes) -image focused upside down/brain "turns" it right side up Common visual defects: 1. Nearsightedness: 2. Farsightedness: 3. Astigmatism: 4. Cataracts: 5. Color blindness: HEARING Stimulus: sound waves 3 major areas of ear: external, middle, & inner External Ear: funnels sound waves of air into the auditory canal •auricle or pinna = flap of elastic cartilage known as the ear sends waves down the external auditory canal •tympanic membrane (eardrum) boundary between the external auditory canal and the middle ear •sound waves make it vibrate, which then transfers the energy to the bones of the middle ear. Middle Ear (tympanic cavity): air filled mucosa lined cavity •auditory (Eustachian) tube: links middle ear with nasopharynx: equalizes pressure •smallest bones of the body: ossicles •malleus (hammer), incus (anvil), stapes (stirrup) •malleus secured to the eardrum and stapes fits into the oval window •transmit vibrations from ear drum to oval window 9 Inner (internal) Ear: (labyrinth) •2 major divisions: •Membranous labyrinth: tubes and sacs filled with endolymph •Bony labyrinth: filled w/ perilymph which surrounds membranous labyrinth -channels through the temporal bone -vestibule, cochlea, semicircular canals Vestibule- central egg shaped cavity -lateral wall contains the oval window -contain receptor regions that respond to the pull of gravity and position of head Semicircular canals: posterior to vestibule - 3 canals that are oriented in all three planes of space; involved in equilibrium Cochlea: spiral bony chamber (snail shaped) -3 separate chambers: scala vestibuli, scala tympani, chochlear duct Organ of Corti (organ of hearing) – consists of supporting cells and hair cells, which are receptors for auditory sensations - hair cells are in contact with the cochlear branch of the vestibulocochlear (VII) and covered by the tectorial membrane Sound waves - frequency of vibration is its pitch Physiology of hearing 1. Sound waves that reach the ear are directed by the auricle into the external auditory canal. 2. When the waves strike the eardrum, the eardrum vibrates. The distance the eardrum moves is relative to the intensity and frequency of the sound waves. It vibrates slowly in response to lowfrequency sounds and rapidly in response to high-frequency sounds. 3. The center of the eardrum is connected to the malleus, which also starts to vibrate. The vibration is then picked up by the incus, which transmits the vibration to the stapes. 4. As the stapes moves back and forth, it pushes the oval window in and out. 5. The movement of the oval window sets up waves in the perilymph of the cochlea. 6. As the oval window bulges inward, it pushes on the perilymph of the scala vestibuli. Pressure waves are transmitted from the scala vestibuli to the scala tympani and eventually to the round window, causing it to bulge outward into the middle ear. 10 7. As the pressure waves push on the walls of the scala vestibuli and scala tympani, they also push the vestibular membrane back and forth. As a result, the pressure of the endolymph inside the cochlear duct changes. 8. The pressure changes in the endolymph move the basilar membrane slightly. When the basilar membrane vibrates, the hair cells of the spiral organ move against the tectorial membrane. The bending of the hairs ultimately leads to the generation of nerve impulses. Physiology of Equilibrium Equilibrium: refers to a state of balance between opposing forces. There are two kinds of equilibrium (Static and Dynamic). Static Equilibrium: refers to the balance and posture of the body (mainly the head) when the body is not moving. Dynamic Equilibrium: refers to the balance and posture of the body (mainly the head) in response to rotational movements. Collectively, the receptor organs for equilibrium are in the internal ear and are referred to as the vestibular apparatus. It includes the saccule, utricle, and semi-circular ducts.