Amyloidosis can be described as the accumulation of protein

Amyloidoses
Proteins, Mechanisms and Structures
Hanka Venselaar
0115010, MLW
Table of contents
1: Introduction
2: Primary and Secondary Amyloidosis
-The role of Immunoglobulin Light-chains in
Primary Amyloidosis (AL 13)
-The role of AA-protein in Secondar Amyloidosis (AA)
3: Hereditary Amyloidosis
-Transthyretin (ATTR)
-Apolipoprotein A1 (AApoA1) and A2 (AApoA2)
-Gelsolin (AGel)
-Lysozym (ALys)
-Cystatin C (ACys)
-Fibrinogen A α (AFib)
4: Other Amyloidoses
The role of Aβ-peptide in Alzheimer’s Disease
-
β2-Microglobulin (Ab2M)
-Prion protein (APrp)
-Islet Amyloid Poly Peptide (AIAPP)
5: Intracellular aggregation
-T he role of α-synuclein in the α-synucleinopathies
-The role of Tau-protein in the tauopathies
-
The role of Huntingtin in Huntinton’s Disease
6: Conclusion
7: References
40
40
44
47
49
51
2
13
13
16
17
17
19
20
21
22
24
26
27
31
34
37
1
1: Introduction
All chemical processes in live are controlled by proteins. The human body can produce 100.000 different types of proteins, all with their own specific function 19 .
The information for the proteins is stored in the DNA. It is first transcripted into
RNA and then the RNA is translated into a protein. After dissociation of the translation-complex with the ribosome, the polypeptide chain has to adopt its native conformation to fulfill its role. Folding of the protein is an important process because the function of a protein depends on its conformation. The folding process is guided by the amino acid sequence, other external factors and sometimes by chaperones. Unfortunately, every protein has a small tendency to misfold which can result in a disease. This tendency can be strengthened by mutations. In some diseases the misfolded proteins can accumulate and form aggregates of (fragments of) the protein. The group of resulting diseases are called amyloidoses.
Amyloidosis can be defined by the accumulation of deposits of normally soluble protein deposits in the extra cellular environment. They are also called amyloid fibrils or plaques. These protein aggregates can disturb the structure and function of tissue and organs and are known to cause a wide range of diseases. These involve
Alzheimer’s Disease (AD), different Spongiform Encephalopathies, like
BSE and Creutzfeldt-Jakob (CJ), type 2 diabetes, and also lesser known diseases. For example Dialysis Related Amyloidosis which may affect people who have been on dialysis for a prolonged time. The diseases can be local or systemic. It can affect different organs and give rise to a variety of symptoms.
However, the amyloid structure is always very similar.
A short history
The name amyloid was coined by Virchow in 1854 for the pathological extra cellular material with similar iodine staining as wood and starch 24 . The protein nature of amyloid was described four years later by Friedreich and Kekule and in
1958 Cohen discovered the electron microscopic appearance of amyloid 24 . Amyloid fibrils are long, straight and unbranched
Figure 1: Amyloid fibrils from the Ile56Thr mutant of human lysozyme, produced by transmission electron microscopy. Scale bar, 200 nm 53 . structures. An electron microscopic picture of lysozym amyloid is shown in figure 1. The plaques can also be identified by staining with Congo red. Under a polarized light microscope the stained amyloid show a very specific apple-green birefringence. The most sensitive method of identification is the orange coloured fluorescence 24 .
2
Over 20 different types of amyloid are known nowadays. The proteins involved share no sequential or structural similarity but range from intact globular proteins to largely unstructured peptides. All aggregates however, share a very similar morphology 10 . In 1968 and 1969 two groups discovered the first structures by
X-ray fiber diffraction 25-27 . Glenner and co-workers were in 1970 the first to identify the light-chain of Ig as major part of the aggregates in patients with AL amyloidosis 26 . The same Glenner found in 1984 fibrils with the same characteristics in material derived from brains of Alzheimer patients 24 .
The structure of amyloid fibrils
The typical structure in wich all amyloidogenic peptides accumulate is called a “cross β-structure”. In this highly organized conformation the antiparallel β-strands run perpendicular to the fibril-axis. The hydrogen bonds between the amide and carbonyl groups of the main chain run parallel to the fibril-axis, this can be seen in figure 2. Because the interactions are mainly between backbone atoms it was suggested that every peptide should be able to aggregate under the right conditions
19 . Different proteins which are not associated with amyloid disease have been shown to form deposits under specific conditions. Pawar et al.
introduced a formula to identify amino acid regions that are sensitive for aggregation 21 .
Figure 2: Amyloidogenic proteins with very different sencondary structure can aggregate into fibrils. The cross
β-structure consists of hydrogen bonds between mainchain atoms, parallel to the fibrilaxis, the β-sheets are anti-parallel 9 .
P agg
=α hydr
I hydr +α
α
I
α +α
β
I
β +α pat
I pat +α ch
I ch (1)
In this formula P agg
is the propensity to aggregate ,
I hydr is the hydrophobicity of the sequence, I α is the
α-helical propensity, I β is the β-sheet propensity, I pat is the hydrophobic pattern and I ch is the absolute value of the net charge of the sequence. The coefficients α have been determined by Pawar et al . for every factor and can be found in table 1.
Values of the α-coefficients
Parameter
α
Hydrophobicity −1.99±0.31
α − 5.7±2.3
β
Charge
Patterns 0.39±0.02
Table 1: α-coefficients used in equation (1) 21 .
5.0±1.7
−0.08±0.03
3
The
α-values indicate that hydrophobicity, hydrophobic patterns and the propensity to form β-sheets favour aggregation. Net charge and the presence of
α-helices have a negative effect on aggregation. With this formula the tendency to aggregate of every peptide can be calculated.
Amyloid fibrils have a length of 0.110 μm and a width of ~10nm 28 . They consist of 2-6 proto-fibrils or protofilaments that twist around each other to form the mature fibril 10, 19, 26, 53 . In figure 3 an amyloid fibril of four twisted proto-fibrils is shown. Congo red can bind between the protofibrils to give the characteristic histological staining.
The mature fibrils make up for 90% percent of the amyloid-plaques but typically there are two other components 50 . The first one is amyloid P (pentagonal) component (AP). This glycoprotein is related to normal serum amyloid protein (SAP) which is used for diagnosis in a SAP-scan because it binds to amyloid independently from the aggregated protein 51 . In this scan radioactive SAP is used to find the localization and size of the aggregates. Furthermore, AP is also thought to protect the plaques against proteolysis 52 .
Figure 3: Amyloid fibrils, made of four twisted protofibrils 9 .
The third component of amyloids, next to the aggregated protein itself and SAP, are proteoglycans 50 . These carbohydrates were responsible for the starch-like staining during the first discovery of amyloid.
They are also thought to initiate the first accumulation steps by providing a scaffold for the first aggregations. For example, the proteoglycan apolipoprotein
E is often found in plaques 9 .
Different structures can be formed by a polypeptide chain; amyloid is just one form of aggregate. Other possible conformations, like oligomers and disordered aggregates, are shown in figure 4. Amyloid is unique in its highly organized
‘misfolded’ structure.
Usually the cell is able to avoid misfolding by control-pathways and even when a protein misfolds it is immediately degraded. Sometimes errors in these mechanisms occur and an otherwise soluble proteins can misfold and start to aggregate.
Amyloid fibrils interact with each other via a lot of hydrogen bonds that exclude water-molecules. The conformation is also strengthened by hydrophobic interactions. This structure is so stable that it resists proteolysis and allows a build-up of deposits in tissue 10
.
4
Fig 4: Different conformation are possible when an unfolded protein dissociates from the ribosome.
Amyloid fibrils are just one form of aggregate, but it is unique in having a highly organized
'misfolded' structure 10 . This state is usually avoided but several factors can induce the aggregation into fibrils.
Folding
A correct folding of proteins is essential for all processes in an organism. The native structure of a protein is encoded in its amino acid sequence and corresponds with the structure that is most stable under physiological conditions.
Christian Anfinsen received the Nobelprize in 1972 for his work on the connection between the amino acid sequence and the biologically active conformation. He showed that peptides can also form their correctly folded structures in vitro without any auxiliary factors 56 .
The folding in vitro of some of the simplest proteins is completed in less than 50
μs 10 . For larger proteins the total number of possible conformations is so large that it would take a lot of time to reach its native state by a systematic search of all conformations. Dobson designed the idea of an energy landscape to solve this problem 10, 19, 29 . Different interactions between residues are possible in all possible start conformations. Interactions that occur in the native state are on average more stable than non-native interactions.
5
This search mechanism is able to find the lowest energy structure that corresponds to the native fold. The correct folding of a protein often relies on a few key-interactions that form a folding-nucleus around which the remainder of the protein can condense. When these key-interactions are made, the structure has reached its transition state, see figure 5. The molecule is already forced in a native-like architecture. However it is still possible that the structure gets stuck in a local minimum.
Fig 5: An energy landscape.
Different start-conformations fold into the same transition state with a couple of “keyinteractions” present, the rest of the molecule can fold around this nucleus. The total number of possible conformations decreases along the path 19 .
Other folding theories are also present. For example, Harano and Kinoshita suggested that the driving force of protein folding is the gain of translational entropy of water. This gain overcomes the loss of conformational entropy upon folding. The most entropy is gained in the native state 30 . This explains also why a protein adopts its native conformation.
6
Molecular chaperones can help with a correct folding by offering an environment in which the folding can be completed. They recognize exposed hydrophobic residues which should in majority be inside the molecule in a correct structure.
Some chaperones interact with the newly synthesized chain when it emerges from the ribosome, others are involved at later stages of the process. They often work subsequently to guide all stages in the folding process 10 . Chaperones are important to avoid aggregation because they reduce the probability of interactions between multiple unfolded or partly folded copies of the same molecule. They can also unfold incorrectly folded proteins and give them “a second chance” to refold.
The fact that the concentrations of many of the chaperones are increased during cellular stress points to the idea that chaperones are needed to prevent misfolding 19 . Chaperones are much less abundant in the extra cellular matrix.
Therefore, proteins have to satisfy a “quality control” mechanism before secretion 10 . This involves a series of glycosylations and deglycosylations to prevent secretion of incorrect proteins. Misfolded proteins are usually recognized and degraded by the ubiquitine-proteasome pathway.
The aggregation process
Sometimes misfolded proteins escape the control-process, reach the extra cellular environment and start to aggregate. This process can, for example, be a result of errors in the ubiquitine-proteasome pathway, of errors in chaperones or of errors in the proteins itself. Buxbaum 8 suggested four different ways leading to aggregation of a protein, see also figure 6:
-Type 1: A monomer in equilibrium with the tetramer undergoes misfolding and induces the formation of fibrils. Increased synthesis facilitates the aggregation but is not needed. ATTR and AL fall in this class.
-Type 2: Incomplete digestion occurs when the amount of substrate exceeds the capacity to degenerate these proteins, for example during inflammation. Partly digested proteins accumulate into fibrils, this is for example the case during AA.
-Type 3: A normal cleavage of the precursor yields an aggregation-sensitive fragment. This happens during APP-cleavage, leading to AD.
-Type 4: An unmodified soluble precursor undergoes a conformational change into an amyloidogenic structure.
This occurs during amyloidoses in which wildtype proteins accumulate, like prion-proteins or transthyretin.
Figure 6: The 4 types of amyloidogenesis suggested by Buxbaum 8 .
Fibrils
7
There are a lot of possible changes in proteins that can result in aggregates ranging from mutations in the protein itself to errors in the ubiquitine-control system or a different cleavage. They have in common that the native state of the polypeptide is destabilized leading to an rise in the concentration of unfolded peptides. Overproduction or decreased degradation also leads to an increased concentration of misfolded or (partly) unfolded proteins. The result is a higher tendency to aggregate.
This latter mechanism of overproduction or decreased degradation is also possible for wild-type proteins. It has been shown that for example wild-type transthyretin accumulates when the concentration of the monomer is increased 31 .
Aggregation occurs in several steps. In the first phase of the process, oligomeric species are formed with a limited number of molecules, like dimers and trimers.
Next step is the formation of pre-fibrillar aggregates, resembling small bead-like structures and the earliest structures visible by electron or atomic force microscopy 19 . They assemble into the protofibrils or protofilaments. 2-6 of these twist into the mature fibrils 18 . Experiments in vitro indicated that aggregation in general is characterized by a lag-phase in which a small nucleus is formed. The lag-phase is followed by a period of rapid growth. This process, also known as seeding, can be avoided by addition of preformed aggregates 18 , see also figure
7. Seeding is common for reactions of high-order.
A recent suggestion is that seeding might be an important factor in triggering the aggregation and onset of the disease.
In the prion disease, like
Kuru and Creutzfeldt-
Jakob disease, it seems that ingestion of preaggregated states of identical protein can increase the rate of aggregation through this process 24 .
Figure 7: The formation of aggregates with (blue) and without (red) addition of preformed aggregates.
The lag-phase is shorter when fibrils are added 9 .
8
Forms of amyloidosis
Different proteins are known to be able to aggregate. Although these proteins are very different in their native states, they all adopt a structure with the same properties in the amyloids. This can happen at a few specific organs or in the complete body and give rise to several syndromes. To date more than 25 types of amyloid are known 24 . They are divided into four groups and all of them have a code in which the first A stands for Amyloidosis and the other letters indicate the aggregating protein 55 :
-Primary amyloidosis (AL): caused by accumulation of Immunoglobulin light chains. These peptides are made in excess by dysfunctioning plasma cells.
-Secondary amyloidosis (AA): caused by incomplete proteolysis of serum
Amyloid A protein. This protein is produced in excess during inflammations.
-Hereditary amyloidosis: a much bigger group. It includes all the types of amyloidosis that can be inherited. An autosomal dominant mutation in the protein causes a change in stabilization, folding or metabolism of the protein. This results in aggregation of the changed protein 31 . Several proteins are reported to contain inheritable mutations. The most common form of hereditary amyloidosis is caused by mutations in Transthyretin
(ATTR), others include Apolipoprotein A1 (AApoA1), Gelsolin (Agel),
Lysozyme (ALys), Cystatin C (ACys), Fibrinogen (AFib) and
Apolipoprotein A2 (AApoA2) 31 . These types of amyloidosis are usually systemic.
-Other types of amyloidosis can be caused by a wide variety of proteins.
Most of them cause just one local disease like the A β-amyloid peptide in
AD or Prion-proteins in the Spongiform Encephalopathies.
The official definition of amyloid points to an aggregation of normally soluble proteins outside the cell. There are however some proteins that can aggregate inside the cell and result in a disease. For example, intracellular inclusions of αsynuclein lead to α-synucleinpathies of which Parkinson’s Disease is the most well-known. In a similar way the protein tau induces tauopathies, systemic disorders with a wide variety of symptoms. Local disorders can also be caused by intracellular deposits.
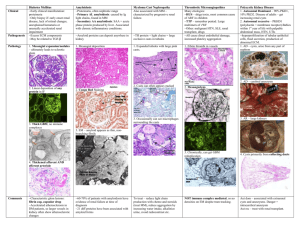
Table 2 gives an overview of different known amyloidoses, the precursor-proteins and their syndromes. Their appearance (local or systemic) and their resulting clinical syndrome is also given. The last group of proteins causes intracellular aggregations, which is according to the definition not a real form of amyloidosis.
The most well-known types of amyloidoses will be explained in the next chapters, they are shown in black.
9
Different types of amyloidoses and aggregation diseases:
Type: Protein-Precursor Local/ Clinical syndrome
AL Ig-light chain
Systemic
S/L Primary systemic amyloidose, myeloma associated
AH Ig-heavy chain S/L Primary systemic amyloidose, myeloma associated
AA Amyloid A-protein from
Serum- AA
S Secondary systemic amyloidose
Hereditary:
ATTR
AApoA1 en 2
Agel
ALys
ACys
Transthyretin (TTR) mutants
Wildtype TTR
Apolipoprotein A1/2
Gelsolin fragment
Lysozym
Cystatin - C
S
S
S
S
S
Familiar Amyloidotic
Polyneuropathy (FAP)
Familiar Amyloidotic Cardiopathy
(FAC)
Senile systemic amyloidose
Familial Amyloidotic
Polyneuropathy 2 (FAP2), Apo-A1
Amyloidosis, Familial Renal
Amyloidosis (FRA)
Finnish hereditary Amyloidosis
Lysozym amyloidosis, Familiar
Renal Amyloidosis (FRA)
Hereditary cerebral amyloid angiopathy
AFib
ABri/AD an
Fibrinogen α-chain
S
Other amyloidoses:
A
β
A
β-precursor protein (APP) L (Brain)
ABriPP/ADanPP L (Brain)
Ab2M β2-microglobulin (B2M) S
AANF Atrial natriuretic factor
Fibrinogen a-amyloidosis, FRA
Alzheimer Disease
Familial Britisch/Danish Dementia
APrp Prions, PrP L (Brain)
AIns Insulin L Insulin related amyloidosis,
Iatrogenic
AIAPP Islet amyloid peptide (IAP) L (pancreas Type 2 diabetes, Insulinomas
ACal (Pro)calcitonin L
Dialysis Related Amyloidosis
(DRA)
Prion-diseases, Spongiform
Encephalopathies (SE) like
B(ovine)SE, Creutzelfdt-Jakob
(CJ), Kuru, Scrapie
Medullary carcinoma of the thyroid, C-cell thyroid tumors
Atrial amyloidosis
APro
AMed
ALac
AKer
Prolactin
Lactadherin
Lactoferrin
Kerato-epithelin
L(Cardiac atria)
L
L
L
L
Aging pituitary/Prolactinomas
Senile aortic, media
Familial
Cornea, Familial
10
Intracellular aggregation proteins:
α-synuclein
L (in cells of basal ganglia)
S
Parkinson’s Disease
Tau
(intracellular)
Tauopathies
Frontotemporal dementia (FTDP-
17), Progressive Supranuclear
Palsy (PSP), Steele-Richardson-
Olszewksi syndrome,
Amyoptrophic Lateral Sclerose,
Lou Gehrig’s Disease,
Corticobasal Degeneration, Pick’s
Disease, Argyrophylic Grain
Disease,
Huntington disease Huntingtin L (CNS, intracellular)
Superoxide dismutase
ZZ-type a1- antitrypsin L( ER of hepatocytes)
Sickle hemoglobin (HbS) L(in
GM2 gangloiside
Erythrocytes)
Amyoptrophic Lateral Sclerose
A1-antitrypsin deficiency
Sickle cell anaemia
Tay-sachs
Rhodopsin y-Crystallins
L(eye)
L(eye)
Retinitis Pigmentosa
Cataract
Table 2: Types of amyloidosis with precursor, localization and resulting diseases. The types printed in black will be discussed in the following chapters. The types printed in grey are lesser known types of amyloidosis and will not be discussed in this study. This table is an interpretation of tables found in reference 8, 26, 32, 53 .
Tissue damage
Why the amyloid plaques cause a disease is still subject of lively debate. It is very well possible that the deposits in the extra cellular environment change the architecture of tissue and organs with subsequent dysfunction of the organ. It is also possible that the fibrillar species interact with receptors. For Aβ-peptide and
TTR it is known that the oligomeric intermediates are toxic and lead to apoptosis via nuclear factor κB 8, 9 .
Intracellular aggregates can also lead to apoptosis. For example, the intracellular deposits that are characteristic for Parkinson’s Disease result in dying of the dopamine producing cells. In this case the toxic mechanism was suggested to be the accumulation of the protein into elliptical pores that can puncture the celmembrane and induce cell death 14 . The toxic mechanism is in the majority of cases not understood.
It is remarkable that the end-stage amyloid fibrils are relatively benign in contrast to the pre-fibrillar aggregates. It is now suggested that the final amyloid aggregates could even be a protection mechanism for the cell by decreasing the amount of highly toxic pre-fibrillar aggregates 19, 29 .
11
The proteins
In this study different amyloidogenic proteins will be identified. Although all proteins could misfold and aggregate, some of them are more sensitive for aggregation than others. They are directly related with several diseases like
Alzheimer’s Disease, Parkinson’s Disease, diabetes type 2, prion-disease and many others. The amyloid types printed in black in table 2 are some of the beststudied amyloidogenic proteins. Their symptoms, the protein precursor and aggregation mechanism will be discussed in the next chapters.
The chapters are organized along the same groups that are used in table 1. First
Primary and Secondary amyloidosis will be discussed followed by different forms of hereditary amyloidosis and several other types of the disease. Additionally, three intracellular forms of intracellular aggregation will be discussed.
The common properties of the amyloidogenic proteins that lead to aggregation are unknown. The involved proteins do not share any sequential or structural similarity. This study provides a set of proteins that can be used in a Molecular
Dynamics simulation in order to find the key-properties that trigger aggregation.
12
2: Primary and Secondary amyloidosis
The role of Immunoglobulin Light-chains in Primary Amyloidosis (AL)
The most common systemic amyloidosis in the western world is Primary
Amyloidosis. It is also called AL because the amyloid deposits consist of the
Light chains of Immunoglobulin antibodies. The disease is associated with multiple meyeloma which is one of the most malignant tumors of bone next to metastatic carcinoma. In multiple meyeloma abnormal plasma cells start to proliferate and replace healthy cells in bone marrow 55 . 12-15% of all patients with this disease also develop AL 9 . Primary amyloidosis can also happen in other monoclonal gammopathies 50 . Transformed memory B-cell clones in the bone marrow start to proliferate and these dysfunctioning plasma cells produce an overload of parts of monoclonal antibodies, even when there is no real cause for it like inflammation. AL is usually systemic. The fragments can accumulate everywhere in the body and can affect different organs. Localised AL is possible but very rare and can be treated with local surgery. In this case the fibril-forming fragments seem to be produced locally 33 .
Different organs can be affected. Aggregation in the heart leads to restrictive cardiomyopathy and primary right-sided heart-failure, in the kidneys it causes proteinuria and/or renal insufficiency. Enlarged liver and a rise in alkaline phosphatase are typical for aggregation in the liver and classic neuropathy and autonomic neuropathy are a result of deposits in the nervous system. Problems in the gastrointestinal tract occur frequently which results in weight loss in nearly all patients 34 . It is neither known why deposits in AL occur in such a wide range of organs nor how organ damage is caused 33 .
The severity of AL varies per patient. It is a rare disease with only 1200 to 3200 new cases each year in the United States. Two third of the patients are male and more than 95% are over 40 years of age 55 . Usually there is a rapid progression, most people die within 2 years after diagnosis. About 20% survives 5 year or longer 54 . A significant shorter survival was observed when cardiac amyloidosis was involved 32 .
Because proliferating cells are involved in this disease, patients are treated with chemotherapy to kill these cells and stop the production of Immunoglobulin lightchains. A bone marrow transplantation may be necessary. Different immunotherapeutic approaches are also being explored 54 .
As can be seen in figure 8 antibodies are made of two heavy chains (blue) and 2 light chains (red), both chains have a constant part and a variable part. The hyper variable antigen binding site is located on top of the chains.
Figure 8: Structure of an antibody, the light chains are red, the heavy chains are blue, both have a constant and variable part 57 .
13
The fibrils found in AL are usually made of the variable part of the light chain (V
L
) or of this chain together with the adjacent part of the constant domain (C
L
) of
Immunoglobulins (Ig). In a few cases complete light chains were found amyloidal 35 .
AL can be caused by all light chain classes but λ-light-chains are three times more often seen in AL than kappa light-chains 33 . Amyloid associated germ-line genes include Vλ6a, Vλ3r, and VκB3 32 . Together they are responsible for 42% of light-chains in aggregates 9 . An amyloid-sensitive sequence can be differentiated from a non-sensitive sequence based on the substituted amino acids. An inverse correlation between stability of the complete sequence with mutation and the propensity to aggregate was demonstrated 36 .
The V
L
chain always has the same framework of 2 β-sheets, consisting of 4 and 5 β-strands. These 2 sheets form a β-sandwich fold and are kept together by a cysteinebridge, as can be seen in figure 9.
The loops between de sheets form the hyper variable region, also called complementary determining region (CDR). This is the part that has to bind to different antigens.
It is very difficult to find a consensus sequence that results in amyloidosis because of the many mutations in the variable regions.
This variation is a result of antigendriven selection undergone by the antigen-producing cell. The antibodies have to recognize many different antigens and need different binding sites to bind them during an immune respons . Some
L-chains are highly amyloidogenic as result of this variation in primary structure 8 . It was confirmed that
Figure 9: Structure of the light-chain domain of an antibody.
It consists of a β-sandwich, linked with a cys-cys bond. The highest variability is found in the CDR domain 58 . mutations in the CDRs have less effect in folding of the light-chain and fibril forming than mutations in the framework region 33 . This result was expected because the loops are not involved in the core of the amyloid fibrils. It is suggested that the common mutation in amyloidogenic light chains is the replacement of conserved polar residues with hydrophobic ones at the surface. This can lead to misfolding of the protein. The other suggested mutation involves the loss of hydrogen bonds within the molecule leading to a less stable structure 33 .
14
Usually an amyloidogenic mutation in a protein destabilizes the native structure.
The concentration unfolded peptide will rise and aggregation can occur. In contrast, the mutated unstable light-chains can still be stabilized by interactions with their heavy-chain. Some mutations in the framework regions of V
L
are tolerated, like for example the D82I mutation. The major problem in AL is the overproduction of light-chains. These light-chains cannot find their heavy-chain counterpart and therefore are not stabilized. The characteristic seeding process is also seen in AL. In 1999 Raffen et al . demonstrated that a partially unfolded state of the protein can cause formation of fibrils, even by a non-amyloidogenic light-chain 33 .
The free fragments can fold in intermediates and form oligomers that can function as nucleation sites for further aggregation. Different mutations in the framework domain are mentioned. They range from insertions that change the loops to deletion of salt bridges 33 . They stabilize the structure. An example is the mutation of D82 in a κ Ig light chain (PDB-entry 1REI), see figure 10 for the structure. Two ionic interactions are possible with this residue and a nonconservative mutation results in destabilization and rapid aggregation of the molecule 16 . The intermediate structure is formed when two shortedge β-strand separate from the others and form a site for
P40 intermolecular hydrogen-bonds. Mutations in two domains are possible to form these intermediate: the loop-fragment containing the two short β-strands (residue 40-61), and the interface between strand A and I. For example, the proline on position 40 is mutated in 80% of the AL cases. This seems to lead to more flexibility and dissociation of the E-F sheets from the β-sandwich 16 . The free edges of the
β-strand act as attracting site for other molecules. They can accumulate into the characteristic crossβ structure is formed.
Proteolysis could play a role in fibril formation.
Figure 10: Ribbon diagram of the Ig κ light chain. The red arrow points to residue P40 in the front loop 16 .
In most cases only part of the light chain has been found in aggregates. It is possible that after the first cleavage, aggregation occurs.
This could protect the chain against complete hydrolysis, while in the normal pathway the first cleavage reduces protection against further proteolysis. It is possible that parts of the light chain are protected by glycosylation 33 . However, the complete aggregation process still remains unclear.
15
The role of AA-protein in Secondary Amyloidosis (AA)
Like primary amyloidosis secondary amyloidosis is a systemic disorder. In this case the deposits are made of AA protein. The precursor is the acute phase reactant Serum Amyloid A (SAA), a high-density lipoprotein (HDL) of class 2 and
3 24 . It is normally degraded by cleavage into small peptides. During chronic infections or inflammatory diseases SAA is made in excess by the liver, stimulated by cytokines, in particular interleukine-6 24 . This exceeds the normal proteolytic capacity. As a result incomplete proteolysis yields amyloidogenic fragments. This pathway is also known as type 2 aggregation according to
Buxbaum and was already mentioned in the introduction 8 . Several disorders can cause an excess of SAA, like rheumatoid arthritis (5-10% of patients), osteomyelitis, dermatomyositis, scleroderma, regional enteritis, ulcerative colitis or granulomatous ileitis. Some of them are hereditary like familial Mediterranean fever, familial cold urticaria, Muckle-Wells syndrome and tumor necrosis factor receptor-associated periodic syndromes 8, 50, 55 .
Aggregates usually occur in the kidneys leading to proteinuria, edema and fatigue. The disease progresses to renal disease and requires renal replacement if untreated. Kidney failure is the cause of death in 40-60% of all cases.
Gastrointestinal complications are another frequently seen problem (20% of patients 32 ) resulting in chronic diarrhea, gastrointestinal bleeding, abdominal pain, and malabsorption. Other organs affected by aggregates are the liver and spleen. Cardiac aggregates were observed In 10% of the patients but these progress very seldom to a fatal state. All these problems can be added to the problems already caused by the underlying inflammation.
The underlying inflammatory process has to be present for a long time. Most people survive 4 to 10 years after diagnosis 32 . This survival depends on treatment of the underlying condition. Focus of the treatment is the inflammatory process. A disease like tuberculosis can be cured with medicines. The associated accumulation of AA can be stopped in this way. This is why AA may probably still be the most common form of amyloidosis. In areas where underlying conditions cannot be cured because of lack of money, the disease is common 8 .
The most abundant isoform of precursor SAA is SAA1, it has at least 5 allelic variants which differ in single amino acids mutations. This SAA genotype has been shown to affect the sensitivity of an individual for AA 32 . Binding of SAA to heparin sulphate (HS), a component of the extra cellular matrix, has been shown to induce AA fibril formation. Inhibiting this interaction prevents fibril formation 32 .
A new anti-amyloid agent was developed based on these observations. NC-503 inhibits the interaction of SAA with glycosaminoglycans, like HS. It has been shown to reduce progression of renal disease compared to a placebo in a trial 32 .
The fragment aggregating in AA consists of the 44 to 100 N-terminal amino acids of SAA, but the structure is unknown.
16
3: The hereditary amyloidoses
The inheritable forms of amyloidosis are the third well-described group of amyloidoses. Usually there is a very clear cause for the aggregation of the proteins, for example, a destabilizing mutation. The inheritable amyloidoses are usually systemic. Transthyretin is the best-studied protein in this group.
Mutations in this protein cause a form of amyloidosis that was given the name
ATTR. The disease was originally also known as tertiary amyloidosis. With the discovery of inheritable mutations in other proteins the name of this group was changed into hereditary amyloidoses. The proteins discussed here are:
Apolipoprotein 1 and 2, Gelsolin, Lysozym , Cystatin C and Fibrinogen.
Transthyretin (ATTR)
ATTR is the most common form of the hereditary systemic amyloidosis. In this case the cause is very clear. A mutation in transthyretin (TTR) leads to dissociation of the physiological functional homo-tetramer. The TTR-monomer misfolds into the amyloid precursor that can aggregate.
Diseases associated with mutations in TTR are mostly seen as familial amyloidotic neuropathy (FAP) because the nervous system is most affected.
Other involved organs include heart, eyes, gastrointestinal tract and the kidneys.
Aggregates in these organs result in familial amyloid cardiomyopathy (FAC), gastrointestinal dysfunction, nephropathy and vitreous opacities. Leptomeningeal amyloid deposition in the brain can cause cerebral haemorrhage and dementia 31 .
Survival depends on the type of mutation and the time of diagnosis. The disease tends to progress faster and cause death sooner when it is discovered in earlylive (around 20-30 years). For example, a V30M variant in Northern-Portugal causes onset at 30 years of age and death at 40 31 . The common age of onset is after 50 years of age, and patients can survive 15-20 years after diagnosis 54 .
The disease is spread worldwide but different variants can have a different prevalence and penetration. The usual treatment is liver transplantation because the aggregating protein TTR is produced by liver-cells. A new liver will only make wild type TTR and this can delay or even stop the progress. However, a few cases have been reported to go on with forming amyloid fibrils and this strengthens the hypothesis that wild-type TTR can also form fibrils 31 .
Transthyretin, also known as prealbumin, is a nonessential transport protein of 54 kDa in plasma and cerebrospinal fluid 37 . The 127 amino acid monomer can be seen in figure 11. It has majorly a β-sheet conformation. A functionally active complex consists of four TTR-subunits, this structure can be seen in figure 12.
TTR can transport thyroid hormone (T4) retinol- binding protein, vitamin A and a variety of pharmacological agents such as penicillin 31, 37 .
Figure 11: Monomer of
TTR 3
17
Four identical subunits form a tetramer with a central channel where two T4-molecules can bind. Every monomer consists of two β-sheets in a β-sandwich structure. Each β-sheet is composed of 4 strands, DAGH and CBEF. The first forms a channel for T4, the latter defines the external surface. A small helix connects strand E and F. To form a dimer, the sheets interact through hydrogen bonds between 2 H-strands and 2 F-strands. The tetramer is formed by hydrogen bonds from the main chain of loop-AB to strand H of the other monomer and several hydrophobic interactions 6 .
Mutations in this structure have not been shown to induce a common structural change that could explain the sensitivity for aggregation. They lead to less stability and dissociation of the tetramer.
Binding of a ligand like T4 to the tetrameric fold stabilizes the structure and is thought to be a therapy for TTR-associated amyloidoses 37 .
Figure 12: Tetramer of four TTR subunits 6 .
To date at least 100 mutations associated with amyloid-formation have been found 32 . The TTR gene is located on chromosome 18 and all mutations are single-nucleotide substitutions except for one which is a deletion of a complete codon. In addition to these mutated variants, wildtype TTR has also been found in aggregates in aged individuals. These patients suffered from a condition termed senile systemic amyloidosis 6 . This suggests that mutations in TTR only lead to a younger age of onset and accelerated progression, but that wildtype
TTR is also amyloidogenic 31 . Val30Met is the most common mutation and induces a movement of residue Cys10. This opens a channel through the molecule and alters the specificity for T4. Subsequently, the tetramer is destabilized and this causes aggregation of the TTR monomers.
Mutation of Ile122 in the dimer interface weakens the interaction between two subunits. Leu55Pro induces a drastic structural change by disrupting the D strand. This changes the interaction between the D- and A-strand and between the ABloop and the α-helix. New surfaces are exposed and can form aggregates.
This last mutation was associated with an aggressive form of FAP. It was demonstrated that other mutations in the D-strand give rise to highly aggregationsensitive fragments 6 . Possibly this domain is very important for amyloidogenesis.
Mutation Tyr78Phe also destabilizes the contacts of the α -helix with the AB-loop and yields more amyloidogenic mutants 6 .
TTR accumulates as Buxbaum’s aggregation type 1. The equilibrium between the monomer and tetramer is disturbed by a structural change in the molecule.
The equilibrium is shifted towards the monomer and the increased concentration of monomers results in aggregation.
18
The aggregation profile of TTR shows three “hot spots”, including residues 10-20 in the A β-strand, 23-33 partly in the B β-strand and 105-118 in the beginning of the H β-strand. Most of these strands are involved in stabilization of the tetramer.
The domain with the highest aggregation propensity is formed by residue 105-
115 which can assemble into amyloid fibrils. The only other fragment reported to form fibrils is the peptide 10-20 3 .
Studies of the mutants have led to the hypothesis that mutations that change interactions with the AB –loop and between the subunits, destabilize the tetramer and give rise to aggregation-sensitive monomers 6 . New approaches towards treatment of TTR-amyloidosis are the use of small molecules that can stabilize the tetramer.
Apolipoprotein A1 (AAPoA1) and A2 (AAPoA2)
Apolipoptrotein is the major constituent of high-density lipid particles and has a role in transport of cholesterol to the liver. The complete protein is unstructured at physiological conditions. Its structure is only stabilized when it binds to lipids 9 .
There are eight well-characterized lipoproteins of which Apo-A1 and Apo-A2 will be discussed here.
ApoA1 is a 243 amino acid plasma protein and is produced in the liver and the small intestine. The corresponding gene is located at chromosome 11q23.
Mutations are very rare, in 1990 a first mutation, Gly26Arg, was reported as the cause of Familial Renal Amyloidosis (FRA), a renal disorder. All patients with
FRA are heterozygous for mutations in ApoA1, lysozym or fibrinogen A. The disease usually manifests in mid-adult life. The prognosis of these patients is much better than that of patients with AA or AL. To date, thirteen amyloidassociated mutations have been reported, mostly single nucleotide substitutions
52 . They give rise to different symptoms and a varying age of onset, from 30 years to advanced age. All are autosomal dominant inherited. For example,
Amyloid cardiomyopathy is the dominant feature of patients with Arg173Pro and
Leu174Ser mutations. The first described Arg26Gly mutation results in peripheral neuropathy and FRA. Other mutations lead to renal and hepatic disorders without neuropathy.
Aggregation of Apolipoprotein A1 is caused by incomplete proteolysis yielding a
83 to 100 amino acids long Nterminal fragment which can adopt a β-sheet structure and accumulates into deposits. Wild-type protein is already slightly amyloidogenic. Aggregates of wild-type Apo-A1 occur in the aorta of 20-30% of elderly people 52 .
Mutations are usually located in the first 80 residues and only the mutant peptide has been found in the aggregates. Carboxy terminal mutations have also been reported. They result in cardiomyopathy, cutaneous and laryngeal deposits. The aggregated fragment, however, is consisting of the first 93 residues of
Apolipoprotein. Possibly the mutations alter the proteolysis of the protein 31 .
Another mechanism for aggregation is the reduction of the affinity for lipids. This reduction of affinity results in an increased concentration of unstable peptides in the cytoplasm because Apolipoprotein is only stabilized when it binds to lipids 52 .
19
ApoA1 amyloidosis is treated with renal dialysis or, in worse cases, a liver transplantation to stop the production of the amyloidotic peptides. Kidney and heart-transplantations have also been reported to be a viable approach for treatment of ApoA1-amyloidosis 32 .
The second amyloidotic lipid protein is Apo-A2. The cause of Apo-A2 amyloidosis is rather unique. The mutations at the stop codon in the gene result in an extension of the peptide with 21 amino acids 31 . Three mutations have been described, all with the same clinical presentation of deposits in the kidneys. One patient suffered from cardiac aggregates too. The usual treatment is renal transplantation 31 .
Gelsolin (AGel)
Two mutations in the gelsolin-gene have been found to result in aggregates of an internal fragment of gelsolin. This protein is made by skeletal muscle and macrophages. It is important for the reorganisation of the cyto-skelet and cell motility through its property to bind and cleave actin. Gelsolin is encoded by a single gene on chromosome 9. The protein folds in a central mixed β-sheet with two and four α-helices at its sides. This is a common structural motif for actin depolymerising proteins 38 .
The amyloid deposits affect several internal organs including the heart and kidneys but aggregate mainly in facial regions. The direct cause of gelsolin-associated amyloidosis is a single nucleotide substitution of guanine 654 with adenine or thymidine. This results in 2 possible variants. The first mutation, Asp187Asn, was found in a few families in Finland, US, Holland and
Japan. The second mutation on the same location,
Asp187Tyr, was found in Denmark and
Czechslovakia. Both mutations give similar syndromes: lattice corneal dystrophy, cranial neuropathy and cutis laxia of facial skin 31 .
The mutated Asp187 is part of a Calcium binding site. The mutation results in loss of hydrogens bonds, destabilization and unfolding of this domain.
A protease cleavage site is now exposed between residues Arg172 and Ala173. Cleavage at this point gives rise to a 68 kDa C-terminal fragment that is further cleaved at Met243. The resulting amyloidogenic 8,1 kDa peptide (G173-243) consists of four strands and an α-helix.
Figure 13: 2 amyloidogenic fragments of gelsolin 12 .
20
Further degradation produces fragment G173-202 which is also amyloidogenic.
The latter fragment consists of three strands and has a greater propensity to aggregate than the longer fragment G173-243. Both fragments can be seen in figure 13 12 . In an MD simulation the G173-
243 fragment was shown to lose its αhelical structure, which is possibly a first step in unfolding and subsequent aggregation. The shorter G173-202 fragment was shown to form aggregates in an MD simulation with multiple molecules 12 . So gelsolin-amyloidosis is caused by a hereditary mutation which facilitates the cleavage between residue 172 and
173. Liver transplantation is not an option in gelsolin amyloidosis because the precursor is not made by liver-cells.
Lysozym (ALys)
The complete lysozym protein has been found in deposits in the gastrointestinal tract, kidneys, spleen and liver of patients suffering from ALys. Progression is very slow and the disease often remains unnoticed until a crisis occurs. Common symptoms are FRA and problems in the gastrointestinal. Liver failure, cardiac amyloid and neuropathy rarely occur.
Lysozym was discovered by Alexander
Fleming, who also discovered penicillin, in
1922. The enzym was able to lyse bacteria and that is why he called it Lysozyme.
It hydrolyses the β-1,4-glycosylic linkages that occur in the peptidoglycan cell walls of some microorganisms. The 14,5 kDa C-type class lysozym consists of 130 amino acids and is located on chromosome 12. The expression is very high in haematopoietic cells and bone marrow precursors 39 .
The native structure of lysozym consists of an
α-domain with four α-helices and one 3/10 helix, and a β-domain with an anti-parallel βsheet and a long loop. The structure is shown in figure 14. The two key residues in the active site between these to domains are a glutamic acid (Glu35) and an aspartic acid
(Asp52).
Figure 14: Structure of Lysozyme 3
Four different lysozym point-mutations have been found to be associated with this disease 31 . The best-studied variants Ile56Thr and Asp76His were reported to be enzymatically active but seemed thermodynamically less stable. The
Ile56Thr mutation unfolded 30 times faster than wild-type lysozym, the unfolding of the Asp76His variant was even 160 faster than wild-type protein. It has been shown that the partly unfolded intermediates exposed hydrophobic surfaces 39 .
21
Another mutant was found in 2000 39 , but this Thr70Asn variant was not amyloidogenic and is present in 5% of the British population. This mutation is also less stable than the wild-type, it unfolds faster than lysozym but slower than the other mutants 39 . The two amyloidogenic mutations are very clearly correlated with destabilization of the protein. Three aggregation sensitive “hot spots” have been identified; these include residues 20-34 in helix B, residues 5062 in a βhairpin in the β-domain and residues 73-104 in helix C and additional following residues in the N-terminal region. The major fragment in amyloid deposits consists of residues 49-101, which is helix C and two of the three B-strands. This is exactly the part that unfolds in the Asp67His variant.
Cystatin C (ACys)
Deposits of cystatin C amyloid have been found in internal organs in this hereditary systemic disorder. The brain is most affected by deposits leading to repeated cerebral haemorrhage which is usually the cause of death in early adulthood. The disease usually surfaces when an individual is 30 or 40 years old
31 . The only reported mutation is Leu68Q and it is directly linked to hereditary cystatin C amyloid angiopathy (HCCAA). Wildtype cystatin C however has also been reported to be involved as coprecipitant in disease caused by amyloid β 5 .
Monomeric cystatin C is a serine protease inhibitor.
The single polypeptide chain is 120 amino acids long and includes four cysteines. They bridge between residue 73 and 83 and between residue 97 and 117. The monomer has an
α-helix perpendicular to five antiparallel β-strands. They form a socalled β-grip motif because the sheet slightly bends and grips around the helix 5 . This is shown in figure 15. The mutation Leu68Gln is located at the end of strand B3. The side chain of the Leucin can point into a hydrophobic pocket formed by residues at the en d of the α-helix. The mutant Gln does not fit in this pocket and destabilizes the structure. The mutant is able to dimerize at the temperature of the human body,
Figure 15: Monomer cystatin C whereas the wildtype cystatin only dimerizes at elevated temperature 5 .
Dimerization of cystatin C is tought to be the first step in aggregation of these proteins into amyloid fibrils. Destabilization of the structure makes domainswapping possible. Part of the structure is exchanged with a similar structure and forms part of the other subunit in the same way a single peptide-chain would fold.
In this case the α-helix and two flanking β-sheets are exchanged. This process can be inhibited by stabilizing the monomer structure. Newly introduced cysteinebridges between the exchangeable part and the fixed core reduced domain swapping and subsequently inhibit also fibril formation. Truncated cystatin C protein has also been reported to undergo domain-swapping in the same way, although this molecule missed the first ten N-terminal residues 5 .
22
Two different dimers were observed. The same part is swapped; differences are located in the hinge-region and result in a different overall structure. The first dimer shows th e β-sheets perpendicular to each other with a bend between strands β2 and β3, see figure 16a. The other dimer shows parallel β-sheets.
Strand β2 runs from one domain to the other and becomes β3, shown in figure
16b. A rotation of 69,1 around the backbone phi-angle of hinge residue Ile56 has occurred.
Figure 16: Two different domain-swapped dimers. a: dimer with the β-sheets perpendicular 59 b: dimer with the β-sheets parallel proposed by Janowski et al.
5 .
The latter structure is more similar to the domain swapped dimer of related cystatin A.
The dimmer structure is important because it was suggested to play a role in fibril formation by forming tetramers that can interact and form deposits.
Two dimers can form a tetramer by interacting with their β5 strands, shown in figure 17a. This strand is at the edge of the molecule and is only partly protected by the
Cterminal end of the α-helix. At both sides of the dimer five main-chain-main-chain hy drogen bonds between the β5 strands can be formed 5 , see figure 17b. The tetramers can interact by side-chain-side-chain anti parallel hydrogen bonds between the β2 strands, see figure 17c. This interaction is weaker because only one residue, Gln48, is directly involved.
Although it is not experimentally proven, domain swapping dimerization and tetramerization are likely to play an important role in aggregation 5 . The domain swapped dimers can interact by their unprotected βstrands at the edge of the molecule, as can be seen in figure 17d.
(d)
Figure 17: a: Tetramer of 2 domain-swapped dimers. b: 5 hydrogen bonds between the β5 strands form the tetramer c: hydrogen bond between β2 strands d: fibril formation by tetramers. All from 5
23
This suggests a new approach for drug-development. Molecules that can interact with important dimerization or tetramerization sites, like the β5-strand, can possibly inhibit the formation of oligomers and inhibit fibril formation.
Fibrinogen A α (AFib)
M utations in the fibrinogen Aα- chain are responsible for Familial Renal
Amyloidosis (FRA) together with lysozyme and apolipoprotein A. This nephropathy usually results in hypertension, proteinuria and subsequent azotaemia. It starts in the fourth or fifth decade of life, but has also been seen in the second decade of life. This disorder is the only hereditary amyloidosis that has been reported in children. It progresses to end-stage renal failure during 5-10 years 52 . Deposits are usually seen in the kidneys but also in the spleen, liver and adrenal glands. Neuropathy or cardiac deposits have not been reported in patients with this form of amyloidosis 52. Liver transplantation has been shown to be effective in contrast to renal transplantation which usually results in new deposits in the transplanted organ 52 . Fibrinogen is a precursor for fibrin. Both fibrin and fibrinogen play a role in blood clotting, fibrinolysis, cellular and matrix interactions, the inflammatory response, wound healing, and neoplasia 40 .
Fibrinogen can be converted into fibrin by cleavage of the N-terminal fibrino peptide Aα-chain, this exposes a polymerization site. Fibrin is a complex network of crosslinked fibrinogen molecules.
Figure 18: Fibrinogen and fibrin complex 40 . Three chains (black lines) form a structure with two D-domains at the start and end and with one E-domain in the middle. These E- and D- domains can interact during the formation of fibrin.
24
Fibrinogen is composed of 6 peptide chains, 2 alpha, 2 beta and 2 gamma types which together form the 340 kDa multimer. The subunits form a 45 nm fiber with two outer D-domains and a central E-domain. One subunit of each type forms a coiled-coil structure connected by cysteine bridges to connect the E-domain with the D-domain. All subunits are produced in the liver.
The fibrinogen Aα-chain consists of 610 residues and the polymerization sequence is located at the N-terminus of this chain. It consists of residues 17-20,
Gly-Pro-Arg-Val (GPRV) near the central E domain of the complete fibrinogen complex. When cleaved, these residues can interact with a binding pocket on the
D-domain at the ends of the complex.
Interaction of D-E domains results in the interaction of the middle domain of the chain with the domain at the end of the chain. This arrangement leads to twisted double-stranded fibrils 40 . This normal accumulation is shown in figure 18.
Fibrinogen has to accumulate to fullfil its physiological role. However, fragments of the fibrinogen Aα-chains have been found in amyloids of patients with FRA.
The formed fibril consists of fragments of 49 to 83 residues. The mutations that these patients had were all located in a relatively small C-terminal domain of the chain. The mutations reported to be associated with amyloidosis consist of three puntmutations, Arg554Leu, Gly540Val and Glu526val, and two deletions of a nucleotide at location 4904 or 4897. The latter results in a frameshift and a complete different protein 52, 31 . In a single Korean family a unique frameshift insertion-deletion mutation was found, 17 nucleotides were deleted while 2 new
(CA) were inserted. This caused a peptide with completely different amino acids after residue 516 and a premature stop codon 41 .
Patients are heterozygous for the mutation and often are not aware of the disease in the family because sometimes the symptoms are hardly noticeable.
Often patients are misdiagnosed as having AL amyloidosis. The Glue526Val mutation is the most well-known mutation 52 .
How these mutations result in amyloidogenic mutations and their aggregation mechanism is not clear.
25
4: Other amyloidoses
The fourth group also consists of several proteins that can cause some wellknown diseases like Alzheimer and type 2 diabetes. The majority of mutations in the proteins that cause aggregation are acquired. Only a few inherited mutations have been seen in the case of familial Alzheimer. Except for amyloidosis caused by β2-microglobulin, these forms of the disease are local.
The role of Aβ-peptide in Alzheimer’s Disease
Alzheimer’s Disease (AD) is the best studied form of amyloidosis. The disease is local and mostly sporadic although some familial cases have been described.
The disease is the most common cause of dementia, a state whose name means
“loss of ability to think”. It is named after Aloïs Alzheimer, a German neurologist, who in 1907 first described the symptoms as well as the neuropathological features of Alzheimer's disease 18 . Between 50 and 70 percent of all dementia patiens are suffering from AD. These are 24 million people worldwide, and every year there will be 4.6 million more. These numbers were announced on the
World Alzheimer Day, on 21-9-2005 60 .
An AD patient develops problems with his memory, concentration and orientation.
Changes in ones behaviour and progressive problems with mental functioning, like thinking and speaking, also occur. At first the symptoms may be so slight that they are unnoticed by the patient and his family or friends. However, the symptoms become more severe as the disease progresses and the patient will end up completely dependent of others. The disease also affects the immune system, resulting in pneumonia as most common cause of death 61 .
Neuropathologically the disease is characterized by the presence of amyloid plaques outside the cell in the cortical regions of the brain, the hippocampus, the basal forebrain and brain stem 28 . A major component of these deposits consists of amyloid β (Aβ) peptide aggregates. Inside the cell the neuronal cytoskelet forms neurofibrillary tangles (NFT) at the same time. The microtubule-binding protein Tau is considered to play a major part in the forming of these tangles. A less common form of AD lacks these intracellular tangles. A few cases of this
“plaque only” dementia are reported. To be exact, the second case reported by
Alois Alzheimer himself described a patient with widespread amyloid plaques but not a single neurofibrillary tangle 42 . However, in the majority of cases both intra- and extra cellular aggregates are present. NFTs without extracellular deposits are also common in other neurodegenerative diseases. The role of tau in these diseases will be explained in chapter 5.
26
The A
β-peptide is derived from the
Amyloid Precursor Protein (APP) 18 . APP is a type 1 transmembrane protein which means that it has a single membrane spanning domain, a cytoplasmic Cterminus and and extracellular N-terminus, shown in figure 19. The protein is encoded by a gene on chromosome 21.
Individuals with trisomy-21, Downsyndrom, can suffer from early deposition of A
β-peptide plaques because they carry an extra copy of the APP-gene 28 . Most people suffer from errors in the processing of APP leading to the aggregation-sensitive fragment.
APP can be processed by secretases in 2 different ways. The proteolytic cleavage of these enzymes is shown in figure 20. The
α/γ-secretase pathway yields a nonamyloidogenic product. First
α-secretase cleaves at the extra cellular site between
Lys687 and Leu688, generating a soluble
APP peptide (APP s
α) and a remaining
Figure 19: APP, with sequence and cleavage sites 62 . fragment of 83 residues (C83).
This membrane-peptide can subsequently be cleaved in the hydrophobic transmembrane domain by γ-secretase at Val711 or Ile713 thereby releasing the P3 peptide. The function of these resulting peptides is not yet understood, but they are not involved in aggregation.
The complete APP can also be processed by a β/γ-secretase pathway. Cleavage after Met671 by β-secretase generates a soluble APP peptide (sAPPβ) and a remaining transmembrane peptide C99. γ-secretase can cleave C99 and give rise to P7, an APP intracellular domain (AICD) which can function as t ranscription factor. The other 4kD peptide is the Aβ-peptide. This peptide is released into the extra cellular environment. The majorly formed structure is the
40 amino acid A β40-peptide that can form amyloid deposits. Less than 5% of the newly produced A β-peptides ends at residue 42, this is a result of the two different cleavage sites of
γ-secretase at Val711 or Ile713. This “long” Aβ42peptide is more sensitive to aggregation an it was suggested that this peptide initiates the formation of amyloid plaques 18 . The tendency to aggregate in contrast to the P3 peptide could be a result of the extra residues in the Aβpeptide. The C-terminal amino acids form the transmembrane domain. They are hydrophobic and tend to aggregate when released in the cytosol. T he Aβ42 peptide has 2 additional hydrophobic residues and this could explain the increased tendency to accumulate of this peptide.
27
Figure 20: Processing of
APP. 2 different pathways are possible, but only cleavage by β- and γ- secretase yields an amyloidogenic fragment
(A β in red) 62 .
C83 C99
The assembly of A
β-peptide starts with the accumulation of a few peptides into oligomers, also known as A β-derived diffusible ligands (ADDLs), shown in figure
21c. These ADDLs are similar to the critical nucleus in figure 7. They assemble into protofibrils (PFs), which in turn can form amyloid fibrils. The AFM appearance of protofribrils and fibrils is shown in figure 21b and 21a. The
ADLLs and PFs are considered more toxic than the final amyloid plaques. The fibrils can induce misfolding of new amyloidogenic peptides in the process known as seeding. The proto-fibrils eventually assemble into amyloid plaques but are not per se required for clinical disease 18 .
Figure 21: Different assembly-states of A β-peptide. A: The end-stage amyloid fibrils. B: Protofibrils and C: ADDL’s. Atomic Force Microscopy, Scale bars 200nm 18 .
The correlation between A β/ADDL concentration and cognitive status has been shown 18 . Elevation of the concentration precedes plaque formation and is correlated with memory loss caused by altered A β metabolism.
This is best proven by hereditary autosomal dominant AD. This familial form causes AD on a young age and the usual phenotype involves generation of the hyper-aggretable A β42.
28
Missense mutations are clustered around the N- and C-termini of the A
β-peptide domain in APP and cause an altered cleavage of APP. These familial APP mutations are the rarest known cause of familiar AD, but provide the evidence that A
β-aggregation plays an important role in AD. In figure 22 a couple of these mutations are shown. The new mutant fragment is usually named after its country of discovery.
Figure 22: Mutations in the A β-peptide 18 .
A couple of the A β mutants that have been found to be associated with earlyonset AD or hereditary cerebral haemorrhage with amyloidosis, were studied by
Pawar et al . 21 . They predicted the aggregation propensity of the Flemish (A21G),
Arctic (E22G), Dutch (E22Q), Italian (E22K) and Iowa (D23N) mutation. All but the Flemish variant were predicted to have a higher aggregation rate and indeed these results were confirmed experimentally.
However, the major part of familial AD patients suffers from mutations in the processing enzymes, like missense mutations in the catalytic subunit of
γsecretase, called presinilin (PS). PS associates with other subunits to form
γsecretase that cleaves the transmembrane peptides after cleavage with α- or β- secretase. Over 150 mutations scattered throughout the PS molecule have been described and they all act by increasing the concentration of A
β42 18 . Together with mutations in APP and PS, oxidation and the ε4-apolipoprotein allele are also suggested to be a risk factor for AD 18 .
High resolution studies have not been possible because of the insoluble nature of the amyloid plaques. Electron microscopy (EM) revealed that 2-6 protofilaments are bundled and twisted to yield a fibril with a diameter of 6-12 nm 7 diffraction showed the typical cross
β-motif.
. X-ray
With hydrogen-deuterium exchange it was shown that approximately half of the hydrogens were not protected and not involved in β-sheet formation.
Different other techniques showed that the first 13 -16 residues of the full-length
A β-peptide are not involved in making up the core of the fibril 7 . In several other studies it has been shown that the fibril core adopts an in-register parallel β-sheet conformation.
29
Only residues 15-36 are involved in this amyloid core and there are two turn regions at residues 22-23 and at 29-30 7 . Guo et al . proposed models with this in-register parallel β-sheets, a hydrophobic core and 2 turns regions for the residues 15-36 based upon the structure for
β -helical proteins 7 .
(PDB-entry 1IXA, 1BHE, 2PABa) This proposed model can be seen in figure 23.
The models have a diameter of 35 A. and could serve as one protofilament which can assemble with others into a 6-mer amyloid fibril, shown in figure 24.
Sanchez de Groot et al . studied the aggregation prone regions in different peptides 3 . Aβ-peptide has two aggregation sensitive regions.
Figure 23: Model of the 15-36 amino acids of A β-peptide after
2 ns simulation 8 .
The residues 16-21 overlap with the central hydrophobic cluster of the peptide, a region which plays a role in amyloidogenesis. Indeed, the peptide 16-22 are is able to form fibrils. The other domain consists of C-terminal residues 30-
36 and 38-42 which also have been shown to play a role in aggregation. The first region is thought to include a β-sheet portion in fibrils. Residues 30-40 are located in the core of the
A β-fibrils 3 .
Figure 24: Proposed model of the 6-mer formed by residues 15-36 7 .
So APP can be processed by two different competing pathways, of which only the β-secretase is toxic. A possible therapy could be the activation of the αsecretase pathway. This could lower the concentration of toxic A
β-peptide levels.
The phenotypically related disorders familial British and Danish dementias
(FBD/FDD) are also listed in table 1. They are mentioned here because the symptoms are very much similar to those of AD. Patients also suffer from neurodegeneration. Intracellular NFTs and extra cellular amyloid plaques have been found. However, the amyloid fibrils are composed of completely different molecules 18 . Missense mutations in the BRI and DAN gene change the stopcodons and yield a new amyloidogenic peptide.
30
β2-microglobulin (Ab2M)
Aggregation of β2-microglobulin is strongly related to dialysis and this form of the amyloid is called Dialysis Related Amyloidosis (DRA).
Deposits occur in all patients who are on long-term renal dialysis and mainly occur in the joints, but sometimes also in bones. The disorder can cause carpal tunnel syndrome, in which deposits of the protein wedge the nerves in one’s wrist.
This causes pain, loss of feeling and a tingling feeling 51 . Other symptoms are joint pain and stiffness, soft tissue masses, and weakening of bone resulting in fractures 54 . 50-60% of patients who are on dialysis for more than 10 years develop subchondral bone cysts.
Most symptoms can occur after five years of dialysis and after twenty years almost all patients have some symptoms which fit the diagnosis of DRA.
The protein was discovered as amyloidogenic in 1985. In 2002 the first solution
NMR structure and the first crystal structure have been solved. β2-microglobulin is a small peptide of 99 residues and approximately 12 kDa. The monomer adopts a wellstudied β sandwich structure of a 3 and a 4 stranded β-sheet, linked by a disulfide bond 2 . The complete full-length wild-type protein has been found to be the major component of aggregates but the truncated variant with a deletion of the first 6 N-terminal residues has also been found.
β2-microglobulin is needed in the folding and assembly process of the MHC class 1 complex which has an important role in antigen display. Normal catabolism requires β2-microglobulin to dissociate from the MHC complex and to be transported in the blood to the kidneys. A normal healthy person can remove
95% of the protein by degradation in the proximal tubule. A patient with renal failure cannot remove the protein and nor can a dialysis membrane.
The concentration of the protein in patients can be 60 times higher than the concentration in the bloodplasma of a healthy person 2 .
The elevated concentration causes β2microglobulin to self-assemble and form fibrils, this is shown in figure 25.
Figure 25: Development of DRA 2 .
31
Figure 26: a: The struct ure of β2microglobulin in complex with MHC b: monomer of β2microglobulin 2 .
MHC bonded and free monomeric β2-microglobulin are very similar, see figure
26 2 . The residues with the greatest deviation are in direct contact with the MHC complex. This involves the D-strand that consists of two parts when it is in complex with MHC. Only the first part (D1) is conserved in the solution structure.
This D-strand has been proposed to play a role in edge-edge strand association and fibril formation 2 .
The native protein is not amyloidogenic. β2-microglobulin still remains monomeric in solution at pH 7.0 even when the concentration is 1000 times higher than in patients serum 2 . At acidic conditions fibrils can be formed in vitro.
The peptides adopted different structures like rod-like fibrils (RL) and longstraight (LS) fibrils possibly representing intermediate states of fibril formation.
A complex energy landscape has been suggested for aggregation of β2microglobulin in which different paths can give rise to different morphological types. This landscape can be changed by different solution conditions. Two routes are possible; one dependent on nucleation and resulting in LS fibrils and another route non-nucleation dependent and resulting in RL and worm-like (WL) fibrils. This is shown in figure 27.
Figure 27: Energy landscape for β2-microglobulin, conditions can be changed and this results in different fibril-formations 2 .
32
It has been suggested that unfolding of the protein is needed to provide the amyloidogenic domains and that DRA is a disorder of protein unfolding 2 . With
NMR techniques it was found that residues 25 and 80 linked with the disulfide bond to the E-strand form the most stabile domain. This link seems necessary for amyloid formation. The E-strand has also been shown to form fibrils at acidic pH in vitro and was predicted to be highly amyloidogenic, possibly because the sequence contains a lot of aromatic residues. The central strands form the stabilized core of the amyloid fibril. Strands A, D and G are most unprotected.
They are in contact with the MHC complex and stabilize the overall structure of
β2-micoglobulin.
The truncated variant has been reported to enhance fibril formation 2 . Unfolded non-native states have been reported to be involved as precursors in different cases.
Four “hot-spots” were found: residue 21-31 of strand 2B, residues 56-69 of strand 6F, residues 79-85 forming strand 7G and residues 87-91 of strand H8. A peptide of residue 21-41 has been reported to form fibrils in vitro. The N-terminus of this peptide corresponds to the first predicted hot-spot of residue 21-31 and is also amyloidogenic. Other aggregatable sequences are residue 59-79 and its shorter version 59-71, which involve the second hot-spot 59-69, and the Cterminal peptide 72-99, which involves the third and fourth hotspot. The last 91-
99 and the N-terminal fragment 6-12 residues were not amyloidogenic and probably not relevant for fibril formation. The predicted hotspots are located in βstrands and this suggests that local unfolding is needed for aggregation 3
The core β-strands are B, C, E and F. An
. interconnected network of 14 residues in these corestrands has been observed. These strands were suggested to form the seeding core for fibrillogenesis. A possible model for oligomerization was made by using 2 subunits of isolated β2microglobulin, which lacked the unstable A and G strand. New interactions were made between the B and D strand. A model of 18 monomers interacting in the presented way was also suggested, see figure
28. This model gave rise to an helix of 52 β-sheets in a cross-
β formation 4 .
Therapy is focused upon the use of better methods for dialysis and artificial kidneys. The last years a decrease was seen of patients with DRA after fifteen years of dialysis 8 . This is possibly a result of better dialysis methods, but often this is not sufficient.
Renal transplantation is the only option but not always possible. Other approaches involving the degradation of the aggregates are explored 51 .
Figure 28: Proposed model of a
β2-microglobulin fibril 4 .
33
Prion protein (APrp)
No additional factors are needed to change normal proteinaceous infectious particle or Prion Protein (PrP C ) into the misfolded PrP sc –form that causes many mammalian neurodegenerative disorders. These disorders are seen in cattle as
Bovine Spongiform Encephalopathie (BSE), in sheep as Scrapie (Sc) and in human as Creutzfeldt-Jacob (CJ) or Kuru. This group of diseases is known as
Spongiform Encephalopathies. They all have a long incubation time after which affected people or animals develop problems with their central nervous system.
CJD has a stable estimated incidence between
0.5 and 1.5 cases per million people per year.
85% of the cases is sporadic and the average age of onset is 60 years. It is very rare under
40 and above 80 years. The first symptoms include fatigue, disorderd sleep, decreased appetite, behavioural or cognitive changes, visual loss, cerebellar ataxia, aphasia or motor deficits. During a rapid progress cognitive decline and myoclonus develop. 90% of patients die within one year after diagnosis.
The average time of death is 5 months 1 . The brains of patients show vacuoles inside cells, see figure 29, and neuronal loss. The group diseases is named after this spongiform appearance.
Figure 29: Histopathology of CJ, the light spots are intracytoplasmatic vacuoles, the characteristic of all prion-diseases 1 .
15% of the cases have an inherited form of the disease caused by a mutation in the PRNP gene. Over 50 different mutations have been found but 95% is caused by four point mutations at codons 102, 178,
200 and 210 and insertions of five or six octapeptide repeats. Met or Val on position 129 influences the susceptibility for CJD, incubation time and its clinical characteristics 1 . Onset of the disease is in general earlier than in sporadic disease. The phenotype of familial CJD is very much the same, but some mutations give rise to different symptoms and have been given different names.
Fatal familial insomnia, for example, is the strangest of these phenotypes. It is caused by a mutation in PRNP at codon 178 and a Met on both alleles at codon
129 1 .
CJD can be transmissed. 1% of the cases is iatrogenic, caused by for example transplantations, dural grafts, hormones extracted from human pituitary glands or contaminated neurosurgical instruments. The disease can also be transmitted by the ingestion of affected brain-material. The disease Kuru is caused by cannibalism. The symptom of Kuru is cerebellar ataxia that progresses to a helpless stage in a few months. This disease disappeared together with the suppression of cannibalism. The ingestion of BSE-infected bovine products causes the variant CJD that was first found in 1994 the United Kingdom. Infected people can be young and the disease has a long course. Psychiatric and sensory symptoms are common, and many plaques and widespread vacuoles show a
34
spongiform appearance in the brain, mainly in the cortex, thalamus, brain stem and cerebellum. The aggregates can occur in the intra- and extra-cellular environment 28 . In this disorder the tonsils, small bowel and lymphoid tissue are also infected. The most well-known disorders in animals are BSE in cattle and
Scrapie in sheep, the symptoms are here also changes in behaviour and a rapid progress of the disease. All diseases are caused by a misfolding of Prion Protein.
Normal PrP C is a glycosyl-phosphatidylinositol
(GPI) anchored protein. This means that instead of a transmembrane domain the protein is covalently linked to a sugar-chain.
Therefore it is exclusively located on the outside of the cell-membrane, in this case on the surface of primarily neuronal cells. A signal peptide is cleaved off and the resulting 23-231 fragment is linked to the phosphatidyl inositol.
The function of PrP is unknown, although it plays a role in neuronal metabolism and prevention of cell death 15 . The prion gene
PRNP can be found on chromosome 20.
The structure is shown in figure 30. The Nterminal part of the protein is unstructured and flexible. The globular C-terminal part of PrP C consists of 3 three
α-helices from residues
144-154, 175-193 and 200-219, and of a small anti-parallel β-sheet from residues 128-131 and 161-164. A disulphide bridge connects
Figure 30: Structure of Prion protein 3 . helix 2 and 3 and the octarepeats in the Nterminus bind 4-6 copper-ions. Residues 166-
171 between the β-sheet and helix 2 contain the most differences between human and bovine PrP. Misfolding results in a rise of
β-sheet content and resistance to proteases 15 .
Three predicted “hot-spots” for aggregation have been found. The one at the Nterminus (residues 1-32) appears to be uncertain because it is not necessary for prion transmission and aggregation. The hot-spot in the C-terminal region
(residues 208-252) includes helix C, mutations in this domain have been shown to influence the formation of PrP sc . A hot-spot in the connecting central region of the N- and C-terminal (residues 105-146) includes the residues 106-147 that have been predicted to be important for fibril formation 3 . When formed the PrP sc form can induce misfolding in other PrP C proteins, the toxic agent can replicate itself. A clear distinction between both structures exists. It is the only amyloidogenic peptide which is known to be taken up in the body after oral exposure and this is why it is dangerous to eat meat from infected animals.
35
The α-helical structure of PrP C (starting at residue
125) can form dimers under physiological conditions by swapping of helix 3. Helix 1 from both subunits forms a dimer interface and helix 2 is covalently linked with a disulfide bridge to helix
3 from the other subunit, shown in figure 31. It is not known whether this structure is the start of oligomerization or a physiological state. Inherited mutations that induce prion diseases are located at regions involved with dimerization 17 . PrP sc however was reported to have an increased
βsheet amount 15 . The conformation of the monomers in the present dimer is not changed, it is made of PrP C molecules and of the pathological
PrP sc .
A structural change into PrP sc has been suggested to result in a protein with 2 α-helices and a β-helix.
This conformation has the right amount of β-sheet and fits in a hexagonal symmetry built from 3 or 6 molecules.
Figure 32: Model proposed by Riesner 15 a,-d: monomer, sideview of monomer, hexamer and sideview of the hexamer of prion-protein. e-h: same views for a trimer
Figure 31: Domain swapped dimer of human prion protein 17 .
This present model, shown in figure 32, locates the β-helices inside the hexagonal unit, and the 2 α-helices at the outside.
These units can possibly stack along the fibril-axis into amyloid aggregates 15 .
Therapeutic approaches are mainly focused on prevention.
Surgical operations, transplantations and food production are strongly controlled to decrease the risk for infections.
36
Islet Amyloid PolyPeptide (AIAPP)
The formation of Islet Amyloid Polypeptide (IAPP) aggregates in the pancreas results in β-cell failure during type 2 (non-insulin dependent) diabetes.
In this type of diabetes a person can make insulin but it cannot be taken up in the cells. The age of onset is usually over 40 years and the disease progresses slowly. The symptoms are blurry vision, cuts or sores that are slow to heal, itchy skin, yeast infections, increased thirst, dry mouth, need to urinate often and leg pain 63 . The
β-cell cells secrete insulin and IAPP (also called amylin) together.
Normal IAPP is cleaved from its precursor, released in the circulation and excreted via the kidney. The high demand for insulin during diabetes results in increased production of IAPP. The protein forms amyloid fibrils that are toxic to the β-cells 43 . The overexpression of IAPP is important but not sufficient to develop AIAPP. Affected processing of pro-IAPP results in secretion of partly processed or even unprocessed IAPP which has been reported to have a higher tendency to aggregate. Mutations in the pro-IAPP may influence the stability and processing of the peptide 43 .
90% of the 150 million diabetes-2 patients worldwide develop amyloidosis 13 . The frequency of the disease in humans increases with age and is characterized with hyperglycemia. The disease progresses almost inevitably to β-cell failure. It is thought to arise from genetic but also from acquired defects insulin-sensitive tissues and insulin action 43 . The severity of the disease is related to the amount of IAPP fibrils. Like in other amyloid-related diseases other proteins have been found in the aggregates like serum amyloid P (SAP), apolipoprotein (apo) E and proteoglycan perlecan. The main component is always IAPP 43 .
IAPP is a neuroendocrine peptide hormone with unknown function. It has been proposed that
IAPP plays a role in suppression of food intake, gastric emptying and glucagon secretion of pancreatic α-cells after arginine stimulation.
IAPP is thought to act in the brain upon the calcitonin or calcitonin-like receptor 43 . After cleavage from its 67 amino acids precursor, the peptide consists of 37 amino acids and is unstructured in vitro 43 . A model for the monomeric subunit of the fibrils was proposed by
Kajava et al .
13 , see figure 33. They suggested a three stranded antiparallel β-sheet of residues
12-17, 22-27 and 31-37, with the most hydrophobic residues inside the molecule. The
N-terminus is unstructured apart from a cysteine bridge that links residue 2 and 7.
Figure 33: Monomer of IAPP, proposed by Kajava et al . 13 .
37
The aggregation hot-spots have been predicted to involve residues 12-18 and
22-28 3 . This agrees with residues 12-17 and 22-27 which have been indicated as β-sheets in the core of fibrils. Different smaller peptides have also been shown to aggregate and all are located in the predicted hot-spots. The minimum peptide to form amyloid fibrils was made of residues 22-27. Other species often cannot develop amyloid. Some residues have been mutated to their corresponding residue in human. The mutations R18H, L23F and V26I resulted in a small increase of amyloid formation by inducing a better packing around the sheets.
Pathological mutation S20G results in earlier onset and a severe variant of diabetes type 2. This mutation has not been predicted to be associated with higher aggregation tendency. It probably improves the packing around the turn 3
According to Kajava et al . 13 the 3 β-sheets stack upon each other in a parallel
. order. A small left handed twist of ~1 degree per subunit was introduced. Asn22,
31 and 35, Ser19 and Tyr37 form ladders of hydrogen bonds. The diameter of this protofilament is 4.0-4.5 nm and agrees with values found with EM and X-ray diffraction. This model is shown in figure 34A. The major type of fibrils in AIAPP has been shown by EM to consist of 3 protofilaments in a left-handed coil of 25-
50 nm long. The residues Asn, Thr and Ser on the surface may play a role in inter-protofilament interactions, shown in figure 34B. The fibrils form spontaneously in vitro by a conformati onal change from random coil to β-sheet.
(A) (B)
Figure 34: A: Proposed model of aggregation by Kajava 13 . The β-strands are shown as arrows (purple, yellow and lightblue) and are stacked upon each other. B: An EM picture of human amylin and a model of the left-handed coil 13 .
38
Another possibility for aggregation was proposed by Marzban et al . 43 .
Aggregates of diabetes patients included IAPP with extended N-terminus. This domain is cleaved during normal processing and contains a heparin-binding site.
It was proposed that defects in processing yield unprocessed forms of IAPP that can bind to heparin sulfate proteoglycans, a main component of basement membranes and also found in aggregates. Binding of these components could induce changes of conformation into
β-sheets. It is also possible that hyperglycemia or hyperlipidemia in patients with diabetes type 2 contributes to aggregation.
Insulin-related amyloidosis is related to this type of amyloidosis. A few patients with diabetes type 1 were reported to develop aggregates of insulin at injection sites 64 . But these deposits have also been seen in patients with type 2 diabetes.
Complete full-length insulin was aggregated in the fibrils. Insulin easily aggregates in vitro 44 .
Processed insulin consists of two chains: an
α-chain of 21 residues and a β-chain of
30 residues. They are connected by two cysteine bridges at A7-
B7 and A20-B19. A third cysteine bridge links A6
Figure 35: Dimer and hexamer of insulin subuits. Each monomer consists of 2 chains (light/dark blue and green/yellow), 6 of them assemble into the functional hexamer 65 . and A11. Insulin functions as a hexamer under physiological conditions in complex with two or four zinc-ions.
The insulin dimer and hexamer are shown in figure 35.
Aggregation of insulin occurs through a bulky, non-native monomer. The cysteine-bridges are not broken during the process and the Cterminus of the βchains is not expected to participate in the process 44 .
After dissociation of the hexamer and destabilization of the monomer the peptides can aggregate into protofibrils. These protofibrils have been shown to twist and form a thick mature fibril, or they undergo lateral aggregation as alternative route.
39
5: Intracellular aggregation
Amyloidoses are defined by the aggregation of an otherwise soluble protein in the extracellular environment of the cell. However, a couple of proteins are known that show amyloidogenic behaviour in the cytosol. Parkinson’s disease is the best known disorder in this group and will be discussed together with the tau- and huntingtin-protein. Tau-aggregates can be systemic, while aggregates of
αsynuclein and Huntingtin are located in the brain and CNS.
The role of
α-synuclein in the α-synucleiopathies
Lewy Bodies are the main characteristic for the second most common neurodegenerative disease, Parkinson Disease (PD). They are also found in
Dementia with Lewy Bodies (DLB) and Multiple System Atrophy (MSA).
In 1997
α-synuclein was found to be the major component in Lewy Bodies and
Lewy neurites 11 . These structures were first described in 1912 by Friedriech
Lewy, but their biochemical composition remained unknown until 1997. Lewy found these structures originally in the dorsal motor nucleus of the vagus nervus by patients with Parkinson Disease (PD), but they can also be present in the substantia nigra, the locus ceruleus, the nucleus basalis, the raphe nuclei, the
Midbrain Edinger-Wespthal nucleus, the cerebral cortex, the olfactory bulb and some autonomic ganglia 11 .
The Lewy Bodies are circular intracellular inclusions with a diameter of 5-25
μm. The dense core is surrounded by radially oriented filaments of 10-20 nm in diameter, see figure 36 11 . The Lewy Bodies that are present in cortical areas are less well-defined, with the same spherical shape but lacking a core and halo. They can also contain several other proteins like ubiquitin, neurofilaments and synphilin 14 . Lewy neurites correspond to abnormal neurites with the same staining profile as Lewy Bodies 11 .
Moretaux et al. were in 1988 the first to publish the sequence of
α-synuclein. This name was given to the protein because of the localization in presynaptic nerve terminals and portions of the nuclear envelope.
Although the localization in the nuclear envelope has never been confirmed, the name remained 11 . The protein aggregates cause dying of the dopamine-cells
Figure 36: Lewy Body, with a dense core and a lighter surrounding ring 14 . in the brain, The details of this process are still unknown.
Parkinson Disease is the most well known disease associated with Lewy Bodies.
In 1817 Dr. James Parkinson described Parkinson Disease by four major features: -Rest tremor of a limb (shaking of the limb while resting)
-Slowness of movement (bradykinesia)
-Rigidity, stiffness of the limbs or trunk
-Poor balance
40
A diagnosis of PD is considered when at least two of these features are present.
Symptons typically start at on side of the body but will spread over time to the other side. PD affects 1% of people over 60 years, the average onset is 60 years but early onset PD can also affect younger people. This is the case in 5-10% of all PD patients 66 .
PD is a chronic and progressive disease. It is a result of dying dopamine neurons in the midbrain. Dopamine is an important neurotransmitter, and bodymovement becomes uncontrolled when these cells die. Symptoms of PD develop when 80% of the dopmamine producing cells in the subtstantia nigra are gone. The first symptoms are mild, for example rest tremor in one hand. Over time, the symptoms can become worse, like severe tremor or slowness of bodymovement.
They can give a lot of problems in daily life 66 . In most cases the cause of PD is unknown. However, in a few patients a clear family history is present. In 1997 a missense mutation in the
α-synuclein gene was found to cause familial PD and led to the discovery that α-synuclein is a major part of Lewy Bodies 11 .
The human genome encodes for 3 synucleins, called
α-, β-, and γ-synuclein, all with a similar domain organization and all encoded by five exons. The N-terminal part consists of imperfect amino acid repeat, with the consensus sequence
KTKEGV 11 . It is followed by a hydrophobic middle region and a negatively charged C-terminus.
α-Synuclein consists of 140 amino acids and maps to chromosome 4q21 whereas
β-synuclein is 134 amino acids and maps to chromosome 5q35. They have 62% sequence identity and both have a molecular mass of 19kDa. In all vertebrates α- and β-synuclein are very similar. Both are expressed in presynaptic nerve terminals in contrast to γ-synuclein which is expressed throughout the nerve cell and was also found in the heart. Y-synuclein, which shares 55% sequence identity with α-synuclein, consists of 127 amino acids. It maps to chromosome 10q23 and has a molecular mass of 18 kDa.
The function of the synucleins is unknown, although different roles for
α-synuclein have been proposed. The protein may play a rol in presynaptic regulation of Dopamine release, synthesis and storage, as well as in regulation of synaptic plasticity 14
γ-synuclein
.
α-Synuclein is sensitive for aggregation in contrast to β-and
Two mutations in α-synuclein are known. An Alanine to Threonine mutation on place 53 (A53T) and an Alanine to Proline mutation on place 30 (A30P).
Wild-type α-synuclein is degraded by the ubiquitine-proteasome pathway. The
A53T mutation is known to slow down this process. The increased concentration could result in accumulation of
α-synuclein in the cell. The A30P mutation has no significant effect on accumulation rate, but has been shown to bind less to vesicles in contrast with wildtype α-synuclein 11 . This could be important because α-synuclein is natively unfolded in solution; it only adopts an α-helical structure in presence of lipid-vesicles.
41
Full-length wildtype
α-synuclein has also been shown to be able to form fibrils spontaneously, although the accumulation rate was slower in contrast to the accumulation rate of mutant A53T and truncated versions α-synuclein.
Ten genes have been found to be associated with PD, but only four of them have been characterized so far. Together with α-synuclein these are: parkin, ubiquitin carboxy-terminal hydroxylase L1 (UCHL1), and protein DJ1 11 . Parkin is an E3 ubiquitine ligase, which was suggested to be involved in the degradation of
αsynuclein. The mutations found in autosomal recessive juvenile-onset
Parkinsonism (ARJP), mostly led to loss of function of parkin. However, nullmutations in parkin have not been found to result in Lewy Bodies, while abnormal aggregates of tau-protein have been described in cases of ARJP 11 . This groups
ARJP under tauopathies, which will be described chapter 5. So ARJP leads to nerve cell death without Lewy Bodies. A link to
α-Synuclein in this disease is possible.
UCHL1 and DJ1 are the 2 other genes characterized to be involved with PD. The first enzyme has a hydrolase activity and a ligase activity 14 . DJ1 has been proposed to have a compensatory role during oxidative events 14 . Mutations in both genes could affect the structure and/or clearance of α-synuclein resulting in aggregations of this protein in Lewy Bodies.
Other disease are associated with the same pathology as PD.
Dementia with Lewy Bodies (DLB) is a late-life disease with symptoms that greatly overlap with AD. The Lewy Bodies are particularly abundant in the cingulate cortex 11 .
The largely sporadic neurodegenerative disorder Multiple System Atrophy is characterized by inclusions in the cytoplasm of glial cells. This can result in different syndromes which may be difficult to distinguish from PD, but progress more rapidly. The inclusions consist of straight and twisted filaments with a diameter of 10-30 nm and are very similar to those of DLB, although the concentration of inclusions is higher. Different proteins like ubiquitine and cytoskelet proteins have been found in the inclusions, but the major component is α-synuclein. To date there is no genetic evidence for the role of α-synuclein in
MSA 11 .
α-Synuclein is natively unfolded and can assume different conformations. In solution it is a random coil while in interaction with lipids it is stabilized into an αhelix. In aggregates it adopts a
β-sheet conformation like all other amyloidogenic proteins. The α-synuclein monomers are thought to form Lewy Bodies by first forming soluble oligomers, also called protofibrils. Two of these 4-5 nm wide molecules accumulate into fibrils of 8-10 nm. These fibrils can aggregate into
Lewy Bodies 45 . This is shown in figure 37.
42
Figure 37: Fibrils formation of α-synuclein, monomers accumulate into oligomers which form fibrils. The fibrils eventually form the Lewy Bodies 11 .
All deposits associated with synucleiopathies have been shown to consist of the
NAC (non-AB-component) residue-fragment of 35 amino acids. Residues 1-18,
27-56 and 61-94 have been predicted to be aggregation “hot spots” 3 . And indeed, the NAC domain overlaps with the 61-94 hotspot. This aggregationsensitive domain is absent in β-synuclein and this explains why β-synuclein is not amyloidogenic. The peptide 68-78 has been shown to be the smallest peptide that can aggregate, while the core of the fibrils has been shown to consist of residues 34-101 3 . The earlyonset PD mutations map in the predicted “hot spots”
There is no consensus about the toxicity of the different states. Some researchers consider the final state of Lewy Bodies to be toxic, while others consider them protective. Both A30P and A53T mutations accelerate the protofibril formation, but only A53T accelerates fibril formation while the A30P mutation results in a slower fibril formation. Because both mutation lead to PD,
Maries et al . 14 concluded that protofibrils are more dangerous than fibrils. A possible mechanism for toxicity of α-synuclein protofibrils was shown by
Lansbury et al..
They showed that protofibrils can form elliptical pores, like bacterial toxins, which can puncture cell membranes, resulting in cell death 14 .
Aggregation of α-synuclein seems to be accelerated by Reactive Oxygen
Species (ROS) like superoxide, hydrogen peroxide, and hydroxyl radical, which are formed during Dopamine metabolism in Dopamine neurons.
α-synuclein is possibly changed to form aggregates in the oxidative environment of these cells and this could explain why only the dopamineproducing cells die during αsynucleinopathies.
43
The role of Tau-protein in the tauopathies
The Tau protein plays a similar role in tauopathies as α-synuclein in the synucleinopthies. Aggregation of the protein Tau into neurofibrillary tangles (NFT) occurs intracellular during neurodegenerative diseases, also known as tauopathies. These include Alzheimer’s Disease during which extra cellular aggregates of A β-peptide but also intracellular NFTs are seen. Other disorders are characterized with NFTs without extra cellular deposits, like progressive supranuclear palsy (PSP), corticobasal degeneration (CBD), Pick’s Disease, argyrophylic grain disease and inherited frontotemporal dementia and parkinsonism linked to chromosome 17 (FTDP-17) 22 .
The diseases have a many similarities with sporadic AD. The loss of brain cells causes problems with memory, speech, movement and emotional and behavioral changes can occur. The lesser known disorders are often misdiagnosed as PD or AD because of the slowing of body movement. Usually the diseases affect elderly people and progress slowly. FTDP is an autosomal dominant inheritable familial disease linked to mutations in the Tau-gene.
The Tau protein is able to bind microtubules and is thought to be important for their assembly and stabilization 22, 46 . Tau is natively unstable and interaction with microtubules alters the conformation of the protein. It is mapped to chromosome 17q21 and normally found in the axons of nerve cells, but during the mentioned diseases it is also found in the cell body and dendrites.
Figure 38: EM picture negatively stained preparation
The tau-fibrils are mostly found in the form of a paired helical of tau aggregates of the Alzheimer-type. Examples of the characteristic PHFs (P) and SFs (S) are fragment (PHF), a twisted double-helical ribbon of subunits, indicated. Scale bar, 100 nm. 22 but a minority forms straight filaments (SF) 22 . Their appearance is shown in figure 38. Both have a clear crossβ structure and this is why the tauopathies are considered a brain amyloidosis even though the deposits are intra cellular.
Insertion or exclusion of a 29- or 58-amino acid sequence at the N-terminal side and a 31-amino acid repeat at the C-terminal side leads to six isoforms obtained from a single gene by alternative splicing 22 . Inclusion of the C-terminal repeat leads to a microtubule-binding domain with 4 repeats, exclusion of the domain results in a protein with 3 repeats. These isoforms are shown in figure 39.
Similar amounts of proteins with 3 and 4 repeats can be found in the cerebral cortex of healthy adults. These repeat domains form the fibril core in tauopathies.
44
Over 30 mutations have been described in Tau causing FTDP-17, including missense, deletion or silent mutations in the exon 22 . The disease is characterized with atrophy of the frontal and temporal lobes of the cerebral cortex and often with additional subcortinal changes. The mutations promote aggregation of tau or disturb the interaction of tau with microtubules. This leads to aggregates of all six isoforms of tau.
Approximately half of the mutations acts at RNA level by influencing the splicing of exon 10 22 . These are intronic mutations that act at the splicing enhancer, silencing sequences or stem-loop structure.
These and some other mutations at exon 10 change the splicing of the exon and lead to an overproduction of the four-repeat isoform.
Figure 39: Isoforms of Tau, N-terminal inserts are shown in red and green, the C-terminal insert with extra repeat (black) is shown in yellow. Mutations are also shown 22 .
P301L and P301S in exon 10 are examples of mutations that result in neuronal and glial inclusions of the fourrepeat isoform and FTDP-17. For a very large part, FTDP-17 is caused by alternative splicing of exon 10, which causes an imbalance between three- and four-repeat isoforms of Tau 22 .
The other tauopathies AD, PSP, CBD and PiD have almost the same phenotypes as FTDP-17. Different studies found mutations in Tau and underline the suggestion that Tau dysfunction is of great importance in these disorders 22 . In all cases of FTDP-17 the aggregated Tau was hyperphosphorylated. A study with transgenic mice expressing the pathogenic mutation P301L showed that the increase of hyperphosphorylation increased the amount of fibrils 22 . Tau has also been shown to be induced by
α-synuclein in vitro. This explains the co-occurrence of Tau and
α-synuclein in some neurodegenerative diseases like
PD. Abnormal aggregates of Tau have also been found in cases of autosomal recessive juvenile parkinsonism (ARJP) in which the Parkin-gene often is affected. Parkin is involved in protein-degradation and mutations can result in intracellular accumulation of proteins, including Tau 46 . Mouse lines expressing human Tau show a connection between Tau overexpression or dysfunction and neuronal cell death. A precise mechanism is not yet understood.
45
The tau protein is natively unfolded. Depending on the isoform it is 441 to 253 amino acids long. The longest form was predicted to have three aggregation sensitive regions: 280-278, 335-340 and 374-381, all located in the C-terminal microtubule-binding region where most mutations for FTDP-17 have been found
21 . Twelve of eighteen examined mutations have been predicted to have a higher propensity to aggregate. Two other had a lower tendency to aggregate but were known to decrease the binding to microtubules and induce accumulation by a higher local concentration 21 . The minimal sequence that can accumulate is 43 residues. It correspons to the third binding repeat and some adjacent residues. It has been suggested that a six residue fragment, 306-VQIVYK-311, is the aggregation specific region. Dinoto et al . 47 suggested two regions with morphology-determining residues at 268-312 and 336-342. The first one includes the six residue fragment 306-311, but has been reported to be less important for morphology determining. Fragment 336-342, however, has been found to be the determining region of Tau to form the paired helical fragment 47 .
46
The role of Huntingtin-protein in Huntington’s Disease
In 1972 Dr. George Huntington was the first to describe Huntington’s Disease
(HD) as a neurodegenerative disease. Nowadays it is one of the more common genetic disorders. The symptoms of HD are similar to other neurodegenerative diseases like AD and PD. A patient develops problems with body movement, like walking, balance, talking and coordination. Concentration, memory, thinking and reasoning are also affected. Emotional and behavioural changes can occur. The typical onset of the disease is in mid-life, between age 30 and 45. Progression is slow, the lifespan after diagnosis is 10-20 year. Rare cases of children developing HD are known. Progression is more rapid at a younger age of onset and children with HD hardly ever reach adulthood. HD affects 1 out of every
10.000 Americans. Most people die because of the medical side-effects that can arise with HD, like infections or pneumonia 67 . The disease is autosomal dominantly inherited, and usual has a clear family history. Only a few sporadic cases are known in which the mutation was not inherited but had developed spontaneously 68 .
In 1993 the HD gene was isolated. It is located on chromosome 4 and encodes a protein called Huntingtin. Aggregation of the protein causes damage to brain cells that results in the mentioned symptoms. The aggregates occur intracellular, like in the αsynucleinopathies. They appear in the nucleus and cytoplasm of cells in the striatum, other basal ganglia, cortex and other brain-regions. Cerebellum and hippocampus seem to be spared 48 . Huntingtin accumulates into plaques 28 , shown figure 40. The aggregates are toxic and cause dystrophy of the brain-cells.
The function of Huntingtin is still unknown, but it is necessary for life because knock-out mice without the HD gene fail to pass early embryonic stage 68 .
Huntingtin is a soluble protein in the cytoplasm that can associate with the plasma membrane and organelles or vesicles with membranes 49 . The protein is 348 kDa and 3144 amino acids long 49 . It can be found everywhere in the body, but only outside the cell’s nucleus(ninds). No structural data are known for the complete protein. However, Kegel et al . 49 made a homology model for residues 201-
237, a membrane binding domain.
Figure 40: Fibrils of
Huntingtin peptides 20 .
47
They suggest that Huntingtin first binds to the membrane through electrostatic interactions. Subsequently, an amphipathic helix penetrates the membrane and anchors the protein. They also showed that the targeting to the membrane is disrupted by a glutamine-expansion at the N-terminus. Glutamine is encoded by the nucleotides CAG. The total number of these CAG-repeats can be used to indicate the risk to develop HD. Normal healthy persons with <28 repeats will not develop HD, persons with 29-34 repeats will also not develop HD but their children can be at risk. 35-39 repeats means a certain risk for HD for these people and their children. Over 40 repeats will certainly result in HD 68 . The number of repeats is inversely correlated with the age of onset and progression of the disease 20 . These repeats can disturb targeting to the plasma membrane, because free protein in the cytosol has a higher tendency to aggregate.
Poly-L-glutamine peptides have also been shown to aggregate. Perutz et al .
23 used the exon 1 peptide of Huntingtin,
D
2
Q
15
K
2
, for X-ray scaterring studies.
They proposed a model that fitted their
X-ray data. The model consists of a single β-sheet wound in a circle around the fiber axis. This structure is shown in figure 41. 20 residues form a complete turn and hydrogenbonds can be made between main chains and side chains.
The model explains why 40 repeats is a risk for HD. 2 turns of 20 residues is a stable conformation and can act as nucleus in the seeding process. A single helical turn is not stable and that is possibly why people with fewer repeats than 36 do not develop HD. Other proteins with a poly-glutamine repeat are thought to aggregate in the same way. They may be recruited into the
Huntingtin aggregates. Other disease associated with poly-glutamine repeats are DRPLA, SCA1-3 and SBMA, respectively caused by to much CAGrepeats in the proteins Atrophin-1, ataxin1-3 and the androgen receptor 28 .
Figure 41. A: Schematic projection of a helical fiber with 20 residues per turn and a plane normal to the fibril axis. (Distances in
Angstrom.) B: computer generated model of this structure 23 .
48
6: Discussion
It has become clear that there are many amyloidogenic proteins, all with their own mechanism that leads to aggregation. It is difficult to recognize the common properties of these proteins. There is a great variety in sequence, structure and function of the proteins that can all adopt the amyloidogenic form under the right circumstances. Some proteins that are mainly α-helix have been shown to aggregate with the same ease as proteins that mainly consist of β-sheets. For αhelical proteins this sometimes means that unfolding of the helical domain and refolding into a β-sheet has to occur. In a few cases the structure is even unknown. The native proteins can be monomers, dimers or tetramers. Some of them are functionally active in complex with other proteins, others are even nonessential for life. In some cases the wild-type is already a little bit amyloidogenic, in other cases a mutation induces the aggregation. The mutations can be located in the protein itself, in the pathway that produces it, in the excretion route or even in a completely different process that is only sideways connected with the proteins.
Although there is no consensus in structure or sequence of the native protein a few important conclusion can be made.
The concentration of the protein plays an important role. Very often the concentration of the most aggregation-sensitive conformation is increased.
Different causes for this that were mentioned in this study are:
- overexpression of the protein; like IAPP that is overexpressed
- simultaneously with the expression of other proteins, or like the overexpression of the 4-repeat isoform of tau that is caused by mutations in the gene. Immunoglobulin light-chains are overexpressed because there are too many Ig-producing cells and
AA protein is overexpressed because there is an inflammation somewhere in the body that stimulates the liver to produce AA protein.
Lack of excretion/degradation; like
β2-microglobulin that cannot be excreted by the kidneys in patients with renal malfunctioning or like the A5 3T mutation in α-synuclein that slows down the degradation.
- Dissociation of the oligomer; like the tetramer of TTR that is destabilized by mutations and will increase the amount of monomers in the cell, or the A30P mutation in α-synuclein that disrupts the binding with lipids and also increases the concentration of free protein. Also in HD the CAG-repeat possibly hinders the protein to bind to the membrane.
In an increased concentration the proteins will have a tendency to accumulate.
Even wild-type proteins have been shown to form amyloid deposits when abundant in high concentrations. The body usually avoids these high concentrations by a strictly organized balance between production and degradation of the proteins. This is another important point that can be concluded from this study.
49
Mutations in the protein itself can cause amyloidosis, but are not the only cause for aggregation. The metabolism of the protein is also very important.
A mutation in the metabolic pathway can be enough to cause amyloidosis when the production exceeds the degradation.The mutations can have several effects:
- Destabilize the protein and thereby unfolding the native state. In gelsolin for example this reveals a cleavage-site and eventually leads to a more amyloidogenic fragment. Mutations in lysozym also result in unfolding and an amyloidogenic domain that is revealed.
-
-
Lead to another metabolism: For example APP is cleaved differently in AD because of the mutations in the secretases, resulting in the highly aggregation sensiti ve Aβ42.
Disturb the interaction with complexes. As was already mentioned, this can lead to an increased concentration, for example of
αsynuclein in PD. This is also the case with cystatin C, that can swap domain more easily when a mutation is present.
Lead directly to a more amyloidogenic protein. For example in the - case of Apolipo-protein 2 in which a mutation causes a longer Cterminus that can aggregate.
Mutations in the protein itself that are the direct cause for the accumulation of the protein are mostly seen in the inheritable amyloidoses, like AGel, ATTR, AApoA1 and 2, ACys and AFib.
It can also be concluded that there is a great variety in information about the different proteins that can cause amyloidoses. AD is the best studied type because of its social relevance. The accumulation mechanism and fibril structure of several other types have been studied very well. But for most other forms very little is known.
The formation of the fibril often involves β-strands at the edge of the molecule. It is obvious that in many cases the hydrophobicity of the residues plays an important role. The interaction of the hydrophobic side chains and the exclusion of water molecules is energetically favorable. The mutation of a residue into a hydrophobic residue is often seen in amyloidogenic mutations.
However, other suggestions for fibril formation have also been proposed. For example in the case of Huntingtin, that seems to form a single β-sheet that is wound around the fiber-axis. In other cases, like tau-protein or AA-protein, the process is not understood at all.
It is very well possible that all proteins have a different mechanism of aggregation.
A lot of work has to be done to understand them all. With MD simulations the fibril formation of several proteins can be studied. This study provides a list with proteins that can be used in these studies. It is only a start because there are a lot more amyloidogenic peptides. A few of them are shown in grey in table 2. The study could also be expanded to non-disease related protein deposits. However, the best studied amyloids are listed in this study.
50
7: References
22.
23.
24.
25.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
1.
2.
3.
4.
15.
16.
17.
18.
19.
20.
21.
Johnson RT. Prion diseases. Lancet Neurol. Oct 2005;4(10):635-642.
Radford SE, Gosal WS, Platt GW. Towards an understanding of the structural molecular mechanism of beta(2)-microglobulin amyloid formation in vitro. Biochim Biophys Acta.
Aug 11 2005.
Sanchez de Groot N, Pallares I, Aviles FX, Vendrell J, Ventura S. Prediction of "hot spots" of aggregation in disease-linked polypeptides. BMC Struct Biol. Sep 30 2005;5:18.
Benyamini H, Gunasekaran K, Wolfson H, Nussinov R. Fibril modelling by sequence and structure conservation analysis combined with protein docking techniques: beta(2)microglobulin amyloidosis. Biochim Biophys Acta. Aug 15 2005.
Janowski R, Kozak M, Abrahamson M, Grubb A, Jaskolski M. 3D domain-swapped human cystatin C with amyloidlike intermolecular beta-sheets. Proteins. Sep 16 2005.
Saraiva MJ. Transthyretin amyloidosis: a tale of weak interactions. FEBS Lett. Jun 8
2001;498(2-3):201-203.
Guo JT, Wetzel R, Xu Y. Molecular modeling of the core of Abeta amyloid fibrils. Proteins.
Nov 1 2004;57(2):357-364.
Buxbaum JN. The systemic amyloidoses. Curr Opin Rheumatol. Jan 2004;16(1):67-75.
Merlini G, Bellotti V. Molecular mechanisms of amyloidosis. N Engl J Med. Aug 7
2003;349(6):583-596.
Dobson CM. Protein folding and misfolding. Nature. Dec 18 2003;426(6968):884-890.
Spillantini MG, Goedert M. The alpha-synucleinopathies: Parkinson's disease, dementia with Lewy bodies, and multiple system atrophy. Ann N Y Acad Sci. 2000;920:16-27.
Liepina I, Janmey P, Czaplewski C, Liwo A. Towards gelsolin amyloid formation.
Biopolymers. 2004;76(6):543-548.
Kajava AV, Aebi U, Steven AC. The parallel superpleated beta-structure as a model for amyloid fibrils of human amylin. J Mol Biol. Apr 29 2005;348(2):247-252.
Maries E, Dass B, Collier TJ, Kordower JH, Steece-Collier K. The role of alpha-synuclein in Parkinson's disease: insights from animal models. Nat Rev Neurosci. Sep
2003;4(9):727-738.
Riesner D. Biochemistry and structure of PrP(C) and PrP(Sc). Br Med Bull. 2003;66:21-
33.
Nowak M. Immunoglobulin kappa light chain and its amyloidogenic mutants: a molecular dynamics study. Proteins. Apr 1 2004;55(1):11-21.
Knaus KJ, Morillas M, Swietnicki W, Malone M, Surewicz WK, Yee VC. Crystal structure of the human prion protein reveals a mechanism for oligomerization. Nat Struct Biol. Sep
2001;8(9):770-774.
Gandy S. The role of cerebral amyloid beta accumulation in common forms of Alzheimer disease. J Clin Invest. May 2005;115(5):1121-1129.
Dobson CM. Principles of protein folding, misfolding and aggregation. Semin Cell Dev
Biol. Feb 2004;15(1):3-16.
Poirier MA, Li H, Macosko J, Cai S, Amzel M, Ross CA. Huntingtin spheroids and protofibrils as precursors in polyglutamine fibrilization. J Biol Chem. Oct 25
2002;277(43):41032-41037.
Pawar AP, Dubay KF, Zurdo J, Chiti F, Vendruscolo M, Dobson CM. Prediction of
"aggregation-prone" and "aggregation-susceptible" regions in proteins associated with neurodegenerative diseases. J Mol Biol. Jul 8 2005;350(2):379-392.
Goedert M. Tau protein and neurodegeneration. Semin Cell Dev Biol. Feb 2004;15(1):45-
49.
Perutz MF, Finch JT, Berriman J, Lesk A. Amyloid fibers are water-filled nanotubes. Proc
Natl Acad Sci U S A. Apr 16 2002;99(8):5591-5595.
Gruys E. Protein folding pathology in domestic animals. J Zhejiang Univ Sci. Oct
2004;5(10):1226-1238.
Bonar L, Cohen AS, Skinner MM. Characterization of the amyloid fibril as a cross-beta protein. Proc Soc Exp Biol Med. Sep 1969;131(4):1373-1375.
51
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
Horwich A. Protein aggregation in disease: a role for folding intermediates forming specific multimeric interactions. J Clin Invest. Nov 2002;110(9):1221-1232.
Eanes ED, Glenner GG. X-ray diffraction studies on amyloid filaments. J Histochem
Cytochem. Nov 1968;16(11):673-677.
Ross CA, Poirier MA. Protein aggregation and neurodegenerative disease. Nat Med. Jul
2004;10 Suppl:S10-17.
Dobson CM. Protein misfolding, evolution and disease. Trends Biochem Sci. Sep
1999;24(9):329-332.
Harano Y, Kinoshita M. Translational-entropy gain of solvent upon protein folding.
Biophys J. Oct 2005;89(4):2701-2710.
Benson MD. The hereditary amyloidoses. Best Pract Res Clin Rheumatol. Dec
2003;17(6):909-927.
Obici L, Perfetti V, Palladini G, Moratti R, Merlini G. Clinical aspects of systemic amyloid diseases. Biochim Biophys Acta. Sep 27 2005.
Bellotti V, Mangione P, Merlini G. Review: immunoglobulin light chain amyloidosis--the archetype of structural and pathogenic variability. J Struct Biol. Jun 2000;130(2-3):280-
289. van G, II, Lokhorst H, Hazenberg BP, Vellenga E. Therapeutic options in systemic AL amyloidosis. Neth J Med. Apr 2004;62(4):106-113.
Ozaki S. Role of immunoglobulin light chains in Al amyloidosis. Intern Med. May
2005;44(5):399-400.
Wall JS, Gupta V, Wilkerson M, et al. Structural basis of light chain amyloidogenicity: comparison of the thermodynamic properties, fibrillogenic potential and tertiary structural features of four Vlambda6 proteins. J Mol Recognit. Jul-Aug 2004;17(4):323-331.
Morais-de-Sa E, Pereira PJ, Saraiva MJ, Damas AM. The crystal structure of transthyretin in complex with diethylstilbestrol: a promising template for the design of amyloid inhibitors. J Biol Chem. Dec 17 2004;279(51):53483-53490.
Benyamini H, Gunasekaran K, Wolfson H, Nussinov R. Conservation and amyloid formation: a study of the gelsolin-like family. Proteins. May 1 2003;51(2):266-282.
Merlini G, Bellotti V. Lysozyme: a paradigmatic molecule for the investigation of protein structure, function and misfolding. Clin Chim Acta. Jul 24 2005;357(2):168-172.
Mosesson MW. Fibrinogen and fibrin structure and functions. J Thromb Haemost. Aug
2005;3(8):1894-1904.
Gyung Kang H, Bybee A, Soo Ha I, et al. Hereditary amyloidosis in early childhood associated with a novel insertion-deletion (indel) in the fibrinogen Aalpha chain gene.
Kidney Int. Nov 2005;68(5):1994-1998.
Graeber MB, Kosel S, Egensperger R, et al. Rediscovery of the case described by Alois
Alzheimer in 1911: historical, histological and molecular genetic analysis. Neurogenetics.
May 1997;1(1):73-80.
Marzban L, Park K, Verchere CB. Islet amyloid polypeptide and type 2 diabetes. Exp
Gerontol. Apr 2003;38(4):347-351.
Jansen R, Dzwolak W, Winter R. Amyloidogenic self-assembly of insulin aggregates probed by high resolution atomic force microscopy. Biophys J. Feb 2005;88(2):1344-
1353.
Conway KA, Lee SJ, Rochet JC, et al. Accelerated oligomerization by Parkinson's disease linked alpha-synuclein mutants. Ann N Y Acad Sci. 2000;920:42-45.
Spillantini MG, Goedert M. Tau and Parkinson disease. Jama. Nov 14
2001;286(18):2324-2326.
Dinoto L, Deture MA, Purich DL. Structural insights into Alzheimer filament assembly pathways based on site-directed mutagenesis and S-glutathionylation of three-repeat neuronal Tau protein. Microsc Res Tech. Jul 2005;67(3-4):156-163.
McGowan DP, van Roon-Mom W, Holloway H, et al. Amyloid-like inclusions in
Huntington's disease. Neuroscience. 2000;100(4):677-680.
Kegel KB, Sapp E, Yoder J, et al. Huntingtin associates with acidic phospholipids at the plasma membrane. J Biol Chem. Oct 28 2005;280(43):36464-36473.
52
50.
R.C. Mellors, “Immunopathology – Amyloidosis”, http://edcenter.med.cornell.edu/CUMC_PathNotes/Immunopathology/Immuno_04.html,
51.
52.
30-7-1999
B. P. C. Hazenberg, “Zoektocht naar de bestrijding van amyloidose”, LVD wisselwerkingartikel 2002/2, http://www.lvd.nl/wisselwerking/2002/2/2002-2-29.htm, 29-2-2002
H. J. Lachmann, “eMedicine – Amyloidosis, Familial Renal”,
53.
54.
http://www.emedicine.com/med/topic3379.htm, 22-1-2004
C. M. Dobson, “Protein misfolding and its links with human disease” http://www.beilsteininstitut.de/bozen2002/proceedings/dobson/dobson.html, 15-5-2003
University of Maryland Medical Center, “Amyloidosis”,
55.
http://www.umm.edu/altmed/ConsConditions/Amyloidosiscc.html, 2004
Amyloidosis support network, http://amyloidosis.org/
56.
The Nobel Prize Internet Archive, http://www.nobelprizes.com/
57.
The Univers ity of Arizona, “Antibody Structure” http://www.biology.arizona.edu/immunology/tutorials/antibody/structure.html, 12-6-2000
58.
A. Honegger, “Aho’s Amazing Atlas of Antibody Anatomy”, http://www.biochem.unizh.ch/antibody/, 7 -6-2003
59 .
60.
http://www.man.poznan.pl/CBB/GIF/hcc-dim.gif
Alzheimer’s Disease International, “ World’s Alzehimer Day 2005” ,
61.
62.
http://www.planet.nl/planet/show/id=75098/sc=779f81, 22-10-2005
Alzheimer Europe, http://www.alzheimer-europe.org
Mayo Clinic College of Medicine, “Amyloid Precursor Protein”,
63.
64.
65.
66.
67 .
68.
http://mayoresearch.mayo.edu/mayo/research/mcj/Amyloid.cfm, 2005
“BD Diabetes Worldwide”, ref http://www.bddiabetes.com
B. swift, “Exercise consultation in diabetes – Examination of insulin injection sites: an unexpected finding of local amyloid osis”, http://www.blackwellsynergy.com/links/doi/10.1046/j.1464-5491.2002.07285.x/pdf, 2002
“The structure of insulin”, http://arbl.cvmbs.colostate.edu/hbooks/pathphys/endocrine/pancreas/insulin_struct.html
National Parkinson Foundation, http://www.parkinson.org
Huntington’s Disease Society of America, http://www.hdsa.org
National Institute of Neurological Di sorders and Stroke, “Huntington’s Disease, Hope though research”, http://www.ninds.nih.gov/disorders/huntington/detail_huntington.htm, 8-
3-2005
53