CHAPTER 37 Spirochetes
advertisement

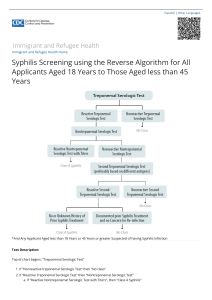
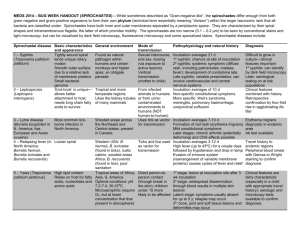
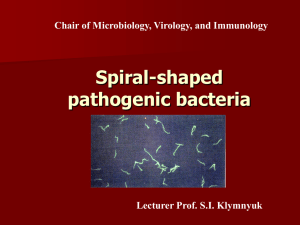
CHAPTER 37 Spirochetes Spirochetes are bacteria with a spiral morphology ranging from loose coils to a rigid corkscrew shape. The three medically important genera include the cause of syphilis, the ancient scourge of sexual indiscretion, and Lyme disease, a newly discovered consequence of an innocent walk in the woods. General Features I. BACTERIOLOGY A. MORPHOLOGY AND STRUCTURE 1. Spiral structure is wound around endoflagella 2. Motility includes rotation and flexion 3. Many are thin and take stains poorly 4. Darkfield microscopy demonstrates unstained living spirochetes B. GROWTH AND CLASSIFICATION 1. Some have not been isolated in culture 2. May be aerobic or anaerobic II. SPIROCHETAL DISEASES 1. Many are part of oropharyngeal flora 2. Overgrowth causes trench mouth 3. Major diseases are zoonoses or venereal TREPONEMA PALLIDUM 1. T. pallidum is the causative agent of syphilis, a venereal disease first recognized in the 16th century as the ”great pox” 2. Syphilis represents an extended balance of parasitism and disease I. BACTERIOLOGY 1. Corkscrew-like spirals spin and bow 2. Heat, drying, and disinfectants kill quickly 3. Prolonged growth only in animals 4. Genomic study is gaining insights 5. Lacks common enzymes 6. No LPS and few proteins in outer membrane II. SYPHILIS A. EPIDEMIOLOGY 1. Infection is acquired from direct sexual contact with an individual who has an active primary or secondary syphilitic lesion 2. Transmission is by contact with mucosal surfaces or blood (transfusion) 3. Congenital infection is transplacental 4. Tertiary syphilis is not infectious 5. Syphilitic lesions are a portal for HIV transmission B. PATHOGENESIS 1. The spirochete reaches the subepithelial tissues through inapparent breaks in the skin or possibly by passage between the epithelial cells of mucous 2. Spread from mucosal breaks to blood is rapid 3. Slow multiplication produces endarteritis, granulomas 4. Initial ulcer heals but spirochetes disseminate 5. Minimal triggers for immune response 6. Injury is due to prolonged hypersensitivity responses C. IMMUNITY 1. Immunity develops slowly and incompletely 2. Antibodies to OMPs are associated with reinfection resistance 3. Development of cell-mediated immunity clears lesions 4. Variable T lymphocyte suppression may link to stages III. SYPHILIS: CLINICAL ASPECTS A. MANIFESTATIONS a. Primary Syphilis 1. Painless, indurated ulcer called the chancre starts the disease 2. Heals spontaneously after weeks b. Secondary Syphilis 1. Secondary or disseminated syphilis develops 2 to 8 weeks after the appearance of the chancre 2. Lymphadenopathy and maculopapular rash are generalized 3. Spirochetes are abundant in lesions 4. Lesions resolve but disease continues in one third of patients c. Latent Syphilis 1. Latent syphilis is by definition a stage where there are no clinical manifestations but continuing infection is evidenced by serologic tests 2. Secondary relapses interrupt latency 3. Blood-borne transmission risk continues d. Tertiary Syphilis i. Neurosyphilis 1. Due to the damage produced by a mixture of meningovasculitis and degenerative parenchymal changes in virtually any part of the nervous system 2. Chronic meningitis leads to degenerative changes, and psychosis 3. Demylination causes peripheral neuropathies 4. Syphilitic paresis has many signs of dementia ii. Cardiovascular syphilis 1. Due to arteritis involving the vasa vasorum of the aorta causing a medial necrosis and loss of elastic fibers 2. Aortitis leads to aneurysm 3. Gummas are destructive, localized granulomas e. Congenital Syphilis 1. Fetuses are susceptible to syphilis only after the fourth month of gestation 2. Rhinitis, rash, and bone changes are common 3. Anemia, thrombocytopenia, and liver failure are terminal events 4. Serologic screening and treatment is preventative B. DIAGNOSIS a. Microscopy 1. Darkfield microscopy requires experience and fluid from deep in lesion 2. May be negative in primary syphilis due to small numbers of spirochetes b. Serologic Tests i. Nontreponemal Tests 1. Reagin antibody reacts with cardiolipin, a lipid antigen complex 2. Most common nontreponemal tests are the rapid plasma reagin (RPR) and the Venereal Disease Research Laboratory (VDRL) 3. Become positive during primary lesion and are uniformly positive during the secondary stage 4. Antibodies slowly wane in the later stages of the disease 5. False positive results can occur in autoimmune states, pregnancy and HIV infection. 6. Antibody level peaks in secondary syphilis 7. Titer is related to disease activity and declines with successful therapy ii. Treponemal Tests 1. T. pallidum is the antigen 2. Fluorescent treponemal antibody (FTA-ABS) uses spirochetes fixed to slides 3. Treponemal tests are more specific than the cardiolipin-based nontreponemal tests 4. Positive result confirms RPR or VDRL 5. Remain positive for life, even after therapy 6. IgM is used to diagnose congenital syphilis C. TREATMENT AND PREVENTION 1. Penicillin is preferred 2. Safe sex blocks transmission LEPTOSPIRA INTERROGANS I. BACTERIOLOGY 1. L. interrogans is the member of the genus Leptospira that is pathogenic to humans and animals 2. Loose spirals seen in darkfield 3. Multiple serogroups have geographic associations 4. Survives in water II. LEPTOSPIROSIS A. EPIDEMIOLOGY 1. Domestic and wild animals are reservoir 2. Water contaminated with animal urine is transmission route B. PATHOGENESIS AND IMMUNITY 1. Enters through small mucosal breaks 2. Blood and CNS spread is common 3. Antibody response may be part of disease III. LEPTOSPIROSIS: CLINICAL ASPECTS A. MANIFESTATIONS 1. Initial disease is flu-like 2. Meningitis and muscle aches last for weeks 3. Hemorrhagic rash is linked to fatal outcome B. DIAGNOSIS 1. Serologic tests are limited to reference laboratories C. TREATMENT AND PREVENTION 1. Penicillin is primary treatment 2. Rodent and water control are important BORRELIA 1. Relapsing fever and Lyme disease caused by different species 2. Loose, irregular spirals take common stains 3. Nutrients taken from external sources 4. Many genes are in plasmids I. Relapsing Fever Borrelia (B. recurrentis, B. hermsii) A. BACTERIOLOGY 1. Surface proteins undergo antigenic variation 2. Recombination between linear plasmids leads to altered protein B. RELAPSING FEVER a. EPIDEMIOLOGY 1. Body lice or ticks transmit the spirochete 2. Tick reservoir feeds on rodents and small animals 3. Nighttime painless tick bite transmits bacteria 4. Body lice infected from human blood 5. Lice must be transferred from human to human b. PATHOGENESIS 1. Spirochetes appear in blood 2. Antigenically different OMPs occur with relapse c. IMMUNITY 1. Antibody eventually controls disease II. RELAPSING FEVER: CLINICAL ASPECTS A. MANIFESTATIONS 1. Fever, headache and muscle pain last 2–4 days 2. Louse-borne is more severe B. DIAGNOSIS 1. Blood smears demonstrate Borrelia C. TREATMENT 1. Doxycycline is primary treatment D. PREVENTION 1. Attention to ticks and general hygiene are important BORRELIA BURGDORFERI I. BACTERIOLOGY 1. B. burgdorferi consists of at least 10 different subspecies which differ in geographic distribution and some clinical manifestations 2. Multiple classes of OMPs, many of which undergo antigenic variation 3. Grows in microaerophilic atmosphere 4. Outer surface proteins (Osps) differ at stages of infection II. LYME DISEASE A. EPIDEMIOLOGY 1. Spirochetes are transmitted in tick–mouse–deer cycle 2. The primary reservoir of B. burgdorferi is rodents, particularly white-footed mice 3. Ticks feed on mice and then deer 4. Adult and nymph stages can infect humans 5. Ticks must feed on humans in the woods to start Lyme disease 6. No deer, no human disease B. PATHOGENESIS 1. Antigenic makeup of B. burgdorferi changes as it migrates from the tick midgut and salivary glands and again after it reaches mammalian tissue 2. OspA predominates in ticks 3. Shift to OspC is completed at vertebrate transmission 4. Surface proteins bind to fibronectin, serum factor H 5. Cell wall peptidoglycan stimulates inflammation 6. Downregulation of immune function contributes to chronicity 7. Antibody may have autoimmune action C. IMMUNITY 1. Target of protective antibody is unclear III. LYME DISEASE: CLINICAL ASPECTS A. MANIFESTATIONS 1. Spreading lesion from bite site is most characteristic finding 2. Erythema migrans and febrile aches mark acute disease 3. Nerve palsies and cardiac findings appear later 4. Fluctuating arthritis may become chronic B. DIAGNOSIS 1. Presently, the diagnosis of early Lyme disease is based on exposure and typical clinical findings 2. Culture is not practical 3. Despite considerable progress serologic tests are not yet definitive C. TREATMENT 1. Doxycycline and β -lactams are recommended D. PREVENTION 1. Preventing bites and removing ticks are important 2. Unique vaccine designed to act in the feeding tick is no longer available