2.5 Recommendations for treatment in Ireland.
advertisement

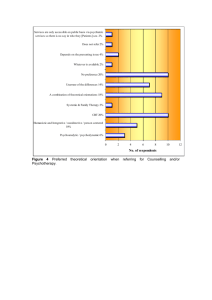
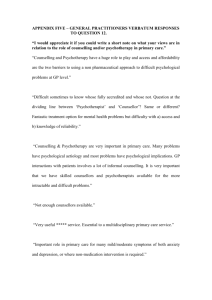
2.5 Recommendations for treatment in Ireland Mimi Copty, from the Irish College of General Practitioners, is the main contributor to the Irish Health Services Executive (HSE) guidelines on mental health. These guidelines are based around a report that Copty completed in 2003 (Copty, M. 2003). In this report patients and primary carers were involved. It was both quantitative and qualitative including responses from GPs, Mental Health providers and Service users. It was limited qualitatively (focus groups) in the number of GPs who participated and notably there were none from a rural practice. There was also a low representation from consultant Psychiatrists (1 in total). In its recommendations to the former South Western Area Health Board (SWAHB) it concluded that mental health training is lacking among GPs even though 95% of mental illness is being dealt with in primary care. Training needs and deficits need to be identified and appropriate training should be provided for GPs. Protocols must be developed for detection, assessment, treatment, referral and interface between primary and secondary care, discharge, and communication with the patient. There also needs to be more collaboration between GPs and Mental Health Service Providers. This can be helped by employing counsellors, psychologists and community psychiatric nurses in the general practice. Mental health providers can relocate to a primary care setting thus facilitating the communication between psychiatric staff and GPs. If there is a regular interface between GPs and Psychiatrists there could be case discussion before referral. Link workers, such as community psychiatric nurses could provide a link from psychiatry to general practice in order to facilitate communication and training needs (Copty 2003). This is calling for a multidisciplinary approach to Mental Health care in the community. There is a lack of knowledge among GPs of the psychological services available. The onus is on allied mental health providers to make themselves known to GPs. It was also found that there was a lack of knowledge concerning various psychological service providers, GPs and the public did not understand the difference between different psychological approaches. It is up to these service providers to educate the public and GPs about licensing and accreditation and the various therapeutic approaches. Media such as leaflets, tapes and posters on Mental Health should be available in GP practices (Copty 2003). There is no specific mention of psychotherapy in this report. The “Guidelines for the Management of Depression and Anxiety Disorders in primary care” (HSE 2006) provide guidelines for screening, assessment, diagnosis and management of depression and anxiety in primary care. It specifically states it is of interest to GPs, pharmacists, psychiatric nurses, psychiatrists, clinical psychologists, service users and all other people caring for depression and anxiety (again counselling and psychotherapy are not mentioned by name). For both depression and anxiety the format is the same. High risk groups are identified. A brief psychiatric assessment guideline is provided for GPs. GPs are asked to consider using one of the widely available psychological instruments to assess depression. There is also a brief summary of the diagnostic criteria as set out in the DSM-IV for diagnosis purposes. The two forms of treatment prescribed are pharmacological treatment and Psychological recommendations made in relation to providing both. treatment. There are no The Psychological section is brief and a little unclear. It does provide a distinction between counselling and psychotherapy but also states that the two overlap. In this section it addresses the lack of primary care psychological services provided by the HSE. However there is a commitment to their development. It is significant that it is believed that this service will be provided by counselling psychologists rather than by any other discipline. Users of the guidelines are also provided with accreditation information. It states that patients with mild to moderate mental health problems should be referred to primary therapy services. More severe cases should be referred to secondary and tertiary services. These are not clearly defined but it assumed Copty means Psychiatric Institutions. The shortcomings of this document are offset by the “Guidance document for the provision of counselling in a primary care setting” (HSE 2006). This guideline document gives definitions of counselling and a brief summary of different approaches. However it does not provide a clear distinction between counselling and psychotherapy. It states that the preferred method of counselling is CBT. The document briefly distinguishes between a counsellor/therapist, a clinical psychologist, a counselling psychologist and an addiction counsellor, but again one would be none the wiser as to what a counsellor/therapist is after reading it. It does however state that only accredited counsellors/psychotherapists and clinical/counselling psychologists would be qualified to provide counselling in primary care. Only in the section entitled “Access to Counselling” do we get an insight into the differences between counselling and psychotherapy. Mild stress related problems, struggling with life events and losses are appropriate for primary care. For severe and complex mental disorders or personality disorders “generic counselling” is not recommended. Patients with trauma, unsuccessful treatment, complex social problems, severe depression, severe anxiety or comorbidity should be referred from a primary care counselling setting to a community mental health team or psychotherapy service.