Discussion of Homework Vignettes
advertisement

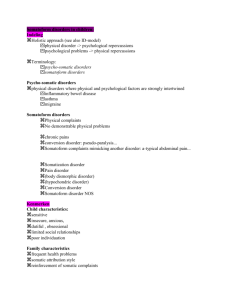
SOMATOFORM and FACTITIOUS DISORDERS EPC 695B, Behavior Disorders Homework Fall 2010 1. Jason is a muscular 24-year-old man who presented himself to the admitting office of a state hospital. He told the admitting physician that he had taken thirty 200-mg tablets of chlorpromazine in the bus on the way over to the hospital. After receiving medical treatment for the “suicide attempt,” he was transferred to the inpatient ward. On mental status examination, the patient told a fantastic story about his father’s being a famous surgeon who had a patient die in surgery. The patient’s husband then killed Jason’s father. Jason stalked his father’s murderer several thousand miles across the United States and, when he found him, was prevented from killing him at the last moment by the timely arrival of his 94-year-old grandmother. He also related several other intriguing stories involving his $64,000 sports car, which had a 12-cyclinder diesel engine, and about his children, two sets of identical triplets. All these stories had a grandiose tinge, and none of them could be confirmed. The patient claimed that he was hearing voices, as on the TV or in a dream. He answered affirmatively to questions about thought control, thought broadcaster, and other unusual psychotic symptoms; he also claimed depression. He was oriented and alert and had a good range of information except that he kept insisting that it was the Iranians (not the Iraqis) who had invaded Kuwait in 1990. There was no evidence of any associated features of mania or depression, and the patient did not seem elated, depressed, or irritable when he related these stories. It was observed on the ward that Jason bullied the other patients and took food and cigarettes from them. He was very reluctant to be discharged, and whenever the subject of his discharge was brought up, he renewed his complaints about “suicidal thoughts” and “hearing voices.” It was the opinion of the ward staff that the patient was not truly psychotic, but merely feigned his symptoms whenever the subject of further disposition of his case came up. They thought that he wanted to remain in the hospital primarily so that he could bully the other patients and be a “big man” on the ward. 4 possible points Axis I 300.16 Factitious Disorder With Predominantly Psychological Signs and Symptoms Although this patient would have us believe that he is psychotic, his story, almost from the start, seems to conform to no recognizable psychotic syndrome. That his symptoms are not genuine is confirmed by the observation of the ward staff that he seems to feign them whenever the subject of discharge was brought up. Why does this fellow try so hard to act crazy? His motivation is not to achieve some external incentive, such as, for example, avoiding the draft, as would be the case in Malingering; his goal of remaining a patient is understandable only with knowledge of his individual psychology (the suggestion that he is motivated to assume the sick role because he derives satisfaction from being “big man” on the ward). 2. Irene, a 36-year-old meter maid, was referred for an evaluation by her attorney. Six months previously, moments after she had written a ticket and placed it on the windshield of an illegally parked car, a man came dashing out of a barbershop, ran up to her, sweating and shaking his fist, swung, and hit her in the jaw with enough force to knock her down. A fellow worker came to her aid and summoned the police, who caught the man a few block away and placed him under arrest. The client was taken to the hospital, where a hairline fracture of the jaw was diagnosed by X-ray. The fracture did not require that her jaw be wired, but the client was placed on a soft diet for 4 weeks. Several different physicians, including her own, found her physically fit to return to work after 1 month. The client, however, complained of severe pain and muscle tension in her neck and back that virtually immobilized her. She spent most of her days sitting in a chair or lying on a bed 1 board on her bed. She enlisted the services of an attorney as the Workmen’s Compensation Board was cutting off her payments and her employer was threatening her with suspension if she did not return to work. The client shuffled slowly and laboriously into the therapist’s office and lowered herself with great care into a chair. She was attractively dressed, well made up, and wore a neck brace. She related her story with vivid detail and considerable anger directed at her assailant, her employer, and the compensation board. It was as if the incident had occurred yesterday. Regarding her ability to work, she said that she wanted to return to the job, would soon be severely strapped financially, but was physically not up to even the lightest office work. She denied any previous psychological problems and initially described her childhood and family life as storybook perfect. In subsequent interviews, however, she admitted that as a child, she had frequently been beaten by her alcoholic father, and had once had a broken arm as a result, and that she had often been locked in a closet for hours at a time as punishment for misbehavior. 6 possible points Axis I 307.89 Pain Disorder Associated with Both Psychological Factors and a General Medical Condition, Chronic In this case, the first question is: Can this woman=s pain be entirely accounted for by the nature of her very real physical injury? Evidently, the answer is no, given the extensive assessment by several physicians. The next question is: Is this woman simply attempting to get continued financial support from Workmen=s Compensation so that she will no longer have to earn a living? If the answer is yes, this would be an instance of Malingering. However, the apparent genuineness of her suffering and her desire to return to work make this unlikely. Although the pain was initially caused by her injury, it appears that she is sufficiently recovered physically and that her persistent complaints of pain are excessive. In addition, there is evidence of specific psychological factors contributing to the severity and maintenance of the pain. The history of the client=s having been physically abused by her father as a child probably produced psychological conflict that was revived by the assault. This might account for the continuation of the pain beyond what would be accounted for by her injury. This leaves us with the diagnosis of Pain Disorder Associated with Both Psychological Factors and a General Medical Condition, as both are judged to play an important role in this case. 3. Patricia, a 34-year-old woman, is currently hospitalized on a general medical ward for evaluation of right-side paralysis. The attending physician requested a psychiatric consultation when no medical reason for the paralysis was found. On examination, Patricia is initially quite upset that anyone doubted the medical nature of her complaints. She reports the sudden onset of right-side problems while she and her boyfriend were talking with a lawyer. According to her this complaint occurred once before: "They thought I had a stroke." She is quite dramatic in her presentation and describes a long, complex medical history. She denies prior psychiatric hospitalizations or contact with other mental health professionals, and denies drug or alcohol abuse or Panic Attacks. Her family history includes a father who was an alcoholic (she is unfamiliar with his recent whereabouts) and a brother who is currently in prison. Review of Patricia's many medical records reveals numerous hospitalizations and medical evaluations for a wide variety of complaints. Complaints that resulted in past hospitalizations or medical evaluations include vomiting, chronic diarrhea, chronic abdominal pain, "crippling" migraines, dysuria, shortness of breath, amnesia, double vision, loss of consciousness, seizures, paralysis (on three different occasions), dyspareunia, dysmenorrhea, dysphagia, menometrorrhagia (irregular and excessive periods), and blindness. Despite numerous extensive medical evaluations, no organic reasons were found for any of her complaints. 3 possible points 2 Axis I 300.81 Somatization Disorder Patricia presents herself in a dramatic fashion, and has a long-standing, complex history. She has multi-organ complaints and no evidence of any medical conditions. Patricia has all the clinical features necessary for the diagnosis of Somatization Disorder. She also meets the criteria for Conversion Disorder; however, this diagnosis can not be given during the course of a more pervasive disorder, such as Somatization Disorder. The Axis II diagnosis is deferred pending additional information and observation. 4. Deborah, a 29-year-old, married woman was presented as a neurology patient at the examination of a young psychiatrist for his specialty certification in psychiatry. Four months previously she had been riding in a car, driven by her husband, that was involved in a minor traffic accident. She was thrown forward, but was kept from hitting the window or dashboard by her seat belt. Three days later she began to complain of a stiff neck and sharp pains radiating down both arms, her spine to the small of her back, and both legs. Because an orthopedic consultation failed to uncover the cause of the pain, she was referred to the neurology clinic. The patient was an attractive, statuesque woman in obvious distress who described her injury and her symptoms in vivid detail, tracing the course of her pains down her arms and legs with her hands. She smiled frequently at the young psychiatrist and at the two examiners who were observing him. She performed each test of neurological function with precision and appeared to relish the attention. The neurological examination findings were totally normal. The psychiatrist inquired into the patient=s personal history and present life. There was not previous history of emotional disturbance. The patient currently worked as a computer programmer. She had been married 4 years and had no children. Until recently her marriage had been sooth, except that her husband sometimes complained that they were mismatched sexually. He seemed considerably more interested in frequent and imaginative sex, whereas she seemed satisfied with weekly intercourse without variation or much foreplay. Two weeks before the accident, the patient had discovered a woman=s phone number in her husband=s wallet. When she confronted him with it, he admitted that he had seen several women over the preceding year, mainly for sexual release. The patient was bitterly hurt and disappointed for several days, and then he began to get angry and attack him for his hang-ups. At the time of the accident, they had been arguing in the car on the way to a friend’s house for dinner. After the accident they decided to try harder please each other in their marriage, including sexually; but because of the pains that the patient was experiencing, they had not been able to have any sexual contact. 5 possible points Axis I 307.80 Pain Disorder Associated with Psychological Factors, Acute The predominant focus of this woman=s clinical presentation is pain in several anatomical sites. The absence of physical findings and the apparent genuineness of the symptoms rule out a physical disorder, Malingering, and a Factitious Disorder. The pain is of sufficient severity to cause her to seek treatment and it impairs her functioning. It is difficult to escape the conclusion that this woman=s pain serves the function of enabling her to avoid an activity that is noxious to her: having to deal with both her husband=s increasing sexual demands and their apparent sexual incompatibility. Further, positive evidence of the role of psychological factors is the temporal relationship between the onset of the symptoms and the discovery of and argument about the husband=s extramarital sexual activity. When psychological factors are judged to have an important role in the onset, severity, exacerbation, or maintenance of pain, and no general medical condition is judged to have an important role, the DSM-IV-TR diagnosis is Pain Disorder Associated with Psychological Factors. The specifier is Acute as the duration of the symptoms is less than 6 months. 3 5. Denny is a 21-year-old man who is concerned about his appearance. One day when he was age 13, Denny was looking in the mirror while combing his hair and noticed that his nose was slightly crooked. He examined it closely from several angles and became convinced that it was abnormal. At breakfast he asked his mother to look at his nose. "It looks fine to me," she said. Denny was not reassured. At school he asked his best friend Steve, "Does my nose look all right to you?" "You mean aside from the big zit," Steve laughed. Denny frowned, "I mean, does it look crooked to you?" Steve looked at Denny with a slight smile and said, "It's a nose. What do you want from it? Let's go to lunch." Despite reassurances from friends and family, Denny continued to be concerned about his nose. He became so self-conscious about his nose that he often held his hand up to cover it when he spoke with people. By the time he was 18, Denny began to investigate the possibility of plastic surgery to straighten his nose. When he was age 21, he made an appointment with a plastic surgeon for an evaluation. 3 possible points Axis I 300.7 Body Dysmorphic Disorder Individuals with this disorder have a preoccupation with an imagined defect or markedly excessive concern about a minor physical anomaly. 6. Walt is a 46-year-old man who has been chronically worried about his health for several years. When he visited his internist for a general physical examination last year, his blood pressure was mildly elevated at 145/93 and his electrocardiogram (EKG) was normal. The physician suggested that he have his blood pressure taken every few months, but decided not to start him on any medication. Despite the reassurance, Walt became convinced that he had high blood pressure. One night he awoke to feel his pulse throbbing in his forehead and some discomfort in his chest. He became convinced that he was having an episode of acute hypertension and a possible heart attack. He became so agitated that his wife drove him to the local hospital emergency room for an evaluation. The nurse took his blood pressure and found it to be mildly elevated blood pressure of 145/90. The physician reassured Walt again, prescribed a mild diuretic, and sent him home after telling him that his chest discomfort was not an indication of a heart attack. Walt felt somewhat better but began to worry again later in the evening when he became aware of his heart beat while lying quietly in bed. The next day Walt made an appointment with his physician. The examination in the doctor's office again showed a mildly elevated blood pressure of 145/90. The physician reassured Walt again, prescribed a mild diuretic, and sent him home after telling him that his chest discomfort was not an indication of a heart attack. Walt felt somewhat better but began to worry again in the evening when he became aware of his heart beat while lying quietly in bed. 4 possible points Axis I 300.7 Hypochondriasis, with poor insight Individuals with this disorder have a persistent (6 months or more) non-delusional belief that they have a serious illness, despite medical reassurance, a lack of physical findings, and failure to develop the disease. Specify "with poor insight" if for most of the time during the current episode, the individual does not recognize that the concern is excessive. 7. Sadie, a 43-year-old woman, was brought into a hospital emergency room by her family who reported that she experienced the sudden onset of blindness. The family explained that Sadie had just discovered that her husband had been having an affair with 4 another woman. She was arguing with her husband when she suddenly stopped and announced that she could not see anything. The family was concerned that the patient might have had a stroke because she had hypertension. The patient's husband and sister brought her to the emergency room. Sadie was examined by the emergency-room physician and the neurologist on call who found no evidence of neurological deficits. The patient's blood pressure was mildly elevated. A psychiatrist was called to see the patient. When he entered the examining room he found a concerned middle-aged woman, the sister, sitting next to the patient and holding her hand. The physician asked Sadie to tell him what had happened and she stated, "I was arguing with my husband and suddenly I couldn't see anymore, but that's OK." The patient seemed to be indifferent to her blindness. 4 possible points Axis I 300.11 Conversion Disorder, With Sensory Deficit Individuals with this disorder have one or more symptoms or deficits affecting voluntary motor or sensory function that are not intentionally produced, yet are judged to be temporally associated with psychological factors such as stress or conflict. The symptoms cannot be fully explained by the direct effects of a substance, a neurological or general medical condition, and are not limited to pain or a sexual dysfunction. Specify one of the following four types: (1) with Motor Symptom or Deficit; (2) With Seizures or Convulsions; (3) With Sensory Symptom or Deficit; (4) With Mixed Presentation. 8. Veronica is an attractive, 24-year-old woman who is concerned about the effect of her health on her social life. She has met eight men in the last year who have asked her out. A few hours before five of the dates she had a sudden attack of diarrhea and vomiting and had to cancel the dates. On two other dates she had an attack of nausea and vomiting in the restaurant powder room. On the eighth date she did not have any symptoms but the man turned out to be a jerk. Veronica denies any anxiety during the dates and is convinced that she has a chronic virus that periodically causes her problems. She has had at least two medical examinations that have not revealed any physical evidence of disease. 3 possible points . Axis I 300.81 Undifferentiated Somatoform Disorder Individuals with this disorder have persistent (6 months) physical complaints that either (1) cannot be explained by a known general medical condition or pathophysiologic mechanism, or (2) if there is a related general medical condition, the physical complaints or impairment is grossly in excess of what would be expected from the physical findings. The symptoms are not intentionally produced.