Online Appendix
advertisement
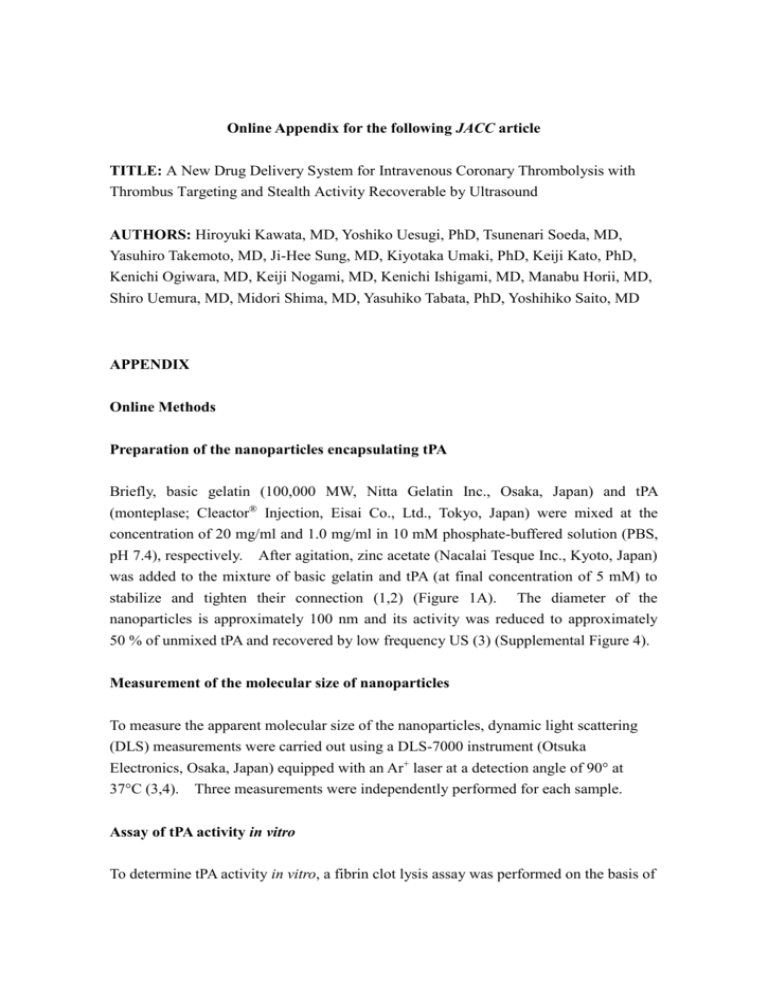
Online Appendix for the following JACC article TITLE: A New Drug Delivery System for Intravenous Coronary Thrombolysis with Thrombus Targeting and Stealth Activity Recoverable by Ultrasound AUTHORS: Hiroyuki Kawata, MD, Yoshiko Uesugi, PhD, Tsunenari Soeda, MD, Yasuhiro Takemoto, MD, Ji-Hee Sung, MD, Kiyotaka Umaki, PhD, Keiji Kato, PhD, Kenichi Ogiwara, MD, Keiji Nogami, MD, Kenichi Ishigami, MD, Manabu Horii, MD, Shiro Uemura, MD, Midori Shima, MD, Yasuhiko Tabata, PhD, Yoshihiko Saito, MD APPENDIX Online Methods Preparation of the nanoparticles encapsulating tPA Briefly, basic gelatin (100,000 MW, Nitta Gelatin Inc., Osaka, Japan) and tPA (monteplase; Cleactor® Injection, Eisai Co., Ltd., Tokyo, Japan) were mixed at the concentration of 20 mg/ml and 1.0 mg/ml in 10 mM phosphate-buffered solution (PBS, pH 7.4), respectively. After agitation, zinc acetate (Nacalai Tesque Inc., Kyoto, Japan) was added to the mixture of basic gelatin and tPA (at final concentration of 5 mM) to stabilize and tighten their connection (1,2) (Figure 1A). The diameter of the nanoparticles is approximately 100 nm and its activity was reduced to approximately 50 % of unmixed tPA and recovered by low frequency US (3) (Supplemental Figure 4). Measurement of the molecular size of nanoparticles To measure the apparent molecular size of the nanoparticles, dynamic light scattering (DLS) measurements were carried out using a DLS-7000 instrument (Otsuka Electronics, Osaka, Japan) equipped with an Ar+ laser at a detection angle of 90° at 37°C (3,4). Three measurements were independently performed for each sample. Assay of tPA activity in vitro To determine tPA activity in vitro, a fibrin clot lysis assay was performed on the basis of the plasminogen-rich fibrin plate method as previously described (4,5). Plasmin, plasminogen, and thrombin isolated from human plasma were purchased from EMD Biosciences Inc., California, USA. Briefly, 10 ml of 0.4 wt% human fibrinogen solution in 0.17 M borate buffer (pH 7.8) was poured into a flat 10 cm Petri dish. Plasminogen (0.2 ml, 50 U/ml) was added to the fibrinogen solution. After adding 0.2 ml of human thrombin (100 U/ml) to induce clot formation, the mixture was left at room temperature for 30 minutes to allow for clot formation. Then, 2.0 l of tPA or nanoparticles before or after 5 minutes of US application (continuous wave, 1.0 MHz in frequency and 1.0 W/cm2 in intensity) in vitro were placed in PBS onto the plate. After incubation at 37°C for 1 hr, the diameter of clear zones was measured while the standard curve between the diameter and the activity was prepared using human plasmin at determined concentrations. The percent activity was calculated as the percentage of sample activity to that of tPA alone. The experiment was independently performed in triplicate for each sample. Animal experiments The experiments in mice and rabbits were carried out according to the Institutional Guidance on Animal Experimentation of Kyoto University and Nara Medical University, respectively. The experiments in swine were performed at the laboratory of the Interventional Technical Center (IVTeC Co., Ltd., Kobe, Japan) and were approved by the Animal Experimental Committee of the IVTeC. Measurement of plasma tPA activity in rabbit and swine models To evaluate whether tPA activity was suppressed by nanoparticles in vivo, in rabbits, blood samples from the femoral artery (FA) were collected just distal to the site of transcutaneous US application immediately, 5, 15, 30, 45, and 60 minutes after the injection of tPA or nanoparticles (n=4 for each treatment). In the swine experiments, blood samples from the left coronary artery (LCA) and right FA were collected separately in each swine immediately (before the US application in the swine treated with transthoracic US), 10, 15, 30, 45, and 60 minutes after the injection of tPA or nanoparticles (n=5 for each treatment). The plasma tPA activity of each blood sample was measured with the synthetic substrate, chromozym tPA, according to the manufacturer’s instructions (Roche Applied Science, Indiana, USA). Data were expressed as the g/ml equivalent of control tPA. In vitro vWF binding assay To evaluate whether vWF protein binds to tPA, basic gelatin, or nanoparticles, enzyme immunoassay (EIA) was performed with the use of rabbit anti-human vWF antibody (DAKO, Glostrup, Denmark) as described previously (6,7) with minor modifications. A 96-well plate was coated with 100 l of anti-human vWF antibody (1.0×10−8 M) as a control. The experimental wells with tPA, basic gelatin, or nanoparticles were coated with 100 l of tPA (1.0×10−6 M), basic gelatin (1.0×10−6 M), or nanoparticles containing basic gelatin (1.0×10−6 M). Subsequently, 50 l of vWF protein (8.0×10−7 M) was added to each well. Horseradish peroxidase (HRP)-conjugated anti-human vWF antibody (DAKO, Glostrup, Denmark) was added to each well. The absorbance of each reaction was measured at the wavelength of 492 nm. Preparation of the mouse arterial thrombosis model Thrombotic occlusion of the left FA in 10 female ddY mice aged 6 weeks was induced by ferric chloride methods as previously described (8,9). The left FA of each mouse was exposed and wrapped with a 5 mm-wide strip of filter paper saturated with 30 % FeCl3 to injure the vessel wall and induce thrombotic occlusion. Evaluation of tPA accumulation in the occluded vessel For the evaluation of tPA accumulation at the thrombus site in the mouse arterial thrombosis model, tPA was radioiodinated with 125I according to the chloramine T method as previously described (10). After iodination, tPA activity was not reduced, suggesting that iodination procedure itself did not affect tPA activity. 125 I-labeled tPA alone (27,500 IU/kg; 0.2235 mg/kg) or nanoparticles containing the same dose of 125I-labeled tPA (n=5 for each) in 100 l of PBS were injected into the tail vein of the mouse 30 minutes after the induction of thrombotic occlusion in the left FA. Ten minutes later, the bilateral iliofemoral arteries at 2 cm length were excised along with the blood inside the lumen after ligation of both ends and all branches. The radioactivity of the iliofemoral artery was counted with a gamma counter (ARC-301B, Aloka, Tokyo, Japan). The radioactivity of the affected left iliofemoral artery was expressed as a ratio of the radioactivity in the contralateral normal iliofemoral artery. Preparation of the rabbit arterial thrombosis model For the preparation of the rabbit arterial thrombosis model, balloon injury of the right femoral artery (FA) was induced according to the procedure reported previously, with modifications (11-13). Twenty male Japanese white rabbits (2.5–2.7 kg; SLC Japan, INC. Shizuoka, Japan) were anesthetized with pentobarbital sodium (25 mg/kg, iv). The first injury was induced by fluoroscopically inserting a PTCA balloon catheter (diameter, 3.0 mm; length, 8.0 mm) via the left carotid artery to a distal site in the right FA where it was inflated to 8 atm. The inflated balloon was then pulled back a distance of 3 cm thrice. After the formation of a stenotic lesion was confirmed angiographically 4 weeks later, a second injury was induced. Another PTCA balloon catheter (diameter, 2.75 mm; length, 15 mm) was inserted via the right carotid artery to a site just distal to the stenotic lesion, and the second injury was induced in the same manner as the first. Thereafter, blood flow was reduced to approximately 10% by incomplete ligation distal to the injured area, which caused immediate formation of an occlusive thrombus. To confirm the presence of a thrombotic occlusion, angiography was carried out using a catheter inserted into the abdominal aorta 15 minutes and 2 hours after the second injury. Thrombolysis in the rabbit model Immediately after confirmation of right FA occlusion, thrombolysis was initiated by the injection of 27,500 IU/kg (0.2235 mg/kg) of tPA, which corresponds to the clinical dose used in humans, or nanoparticles containing the same dose of tPA via an ear vein. In cases treated with US, continuous wave US (1.0 MHz, 1.0 W/cm2) was simultaneously applied transcutaneously over the thrombus up to 60 minutes until successful thrombolysis was obtained (n=10 in each treatment). The ultrasound device comprised of a cylindrical probe, 3 cm in diameter and 6 cm in length, connected to a power amplifier. The effects of thrombolysis were evaluated angiographically. Angiography was carried out every 15 minutes up to 60 minutes after the initiation of thrombolysis, and the Thrombolysis in Myocardial Infarction (TIMI) flow grade was determined. Generation and evaluation of the transthoracic ultrasound device Based on the in vitro and rabbit experiments, we tested US probes of 3 different frequencies (0.5, 1.0, and 2.0 MHz) and 1.0 W/cm2 in intensity. Four US probes of each frequency were combined in parallel as shown in Supplemental Figure 1 to generate continuous wave transthoracic US (TUS) devices for the swine model. Only the 1.0 MHz frequency (continuous wave, 1.0 W/cm2) device produced relatively uniform US fields in a water bath test, as quantified by an oscilloscope. In contrast, TUS with the 0.5 or 2.0 MHz devices produced a protrusive US field at each probe (data not shown). In addition, the 1.0 MHz TUS device created uniform US fields over the swine heart as quantified by a catheter-type oscilloscope inserted into the left ventricle (LV), right coronary artery (RCA), left anterior descending coronary artery (LAD), and left circumflex coronary artery (LCx) as shown in Supplemental Figure 2. Preparation of the swine AMI model For the preparation of the swine AMI model, thrombotic occlusion of the LCx was induced in 60 female swine (35–45 kg) by balloon injury with distal balloon occlusion as shown in Supplemental Figure 3. A 0.014 inch guide wire with a 4 mm balloon at the tip was inserted into the mid-portion of the LCx. The balloon was then inflated to occlude the LCx. The PTCA balloon (diameter 3.5 mm; length 10 mm) was inserted over the guide wire to just proximal of the occlusion balloon, and inflated to 5 atm. The inflated PTCA balloon was then pulled back a distance of 3 cm thrice. After 30 minutes with distal balloon occlusion, thrombotic occlusion of the LCx was confirmed by coronary angiography (CAG). After an additional 30 minutes without distal occlusion, the occlusion of the LCx was reconfirmed. To demonstrate that the thrombus in the swine model was rich in platelets like that of AMI in humans, parts of the thrombi were extracted, fixed in 4 % paraformaldehyde, embedded in paraffin, and cut into 3 m sections, and immunostaining for GP IIb/IIIa (Affinity Biologicals Inc., Ontario, Canada) was performed. Thrombolysis in the swine AMI model After the reconfirmation of occlusion of the LCx, thrombolysis was initiated by the injection of 27,500 IU/kg (0.2235 mg/kg) or 55,000 IU/kg (0.447 mg/kg) of tPA, or nanoparticles containing the same doses of tPA via an ear vein over 5 minutes. Subsequently, continuous wave US (1.0 MHz, 1.0 W/cm2) was applied transthoracically in the cases with TUS for up to 60 minutes (n=10 for each treatment). The position of the TUS device was fluoroscopically confirmed to be located over the heart as shown in Supplemental Figure 1B. Angiography was carried out every 15 minutes up to 60 minutes after initiation of thrombolysis treatment, and the TIMI flow grade was determined. Evaluation of LVEF after thrombolysis At 60 minutes after the initiation of thrombolysis, left ventriculography at left anterior oblique view was carried out to calculate LVEF. Gene expression of apoptotic or inflammatory markers To evaluate the effects of US (continuous wave, 1.0 MHz and 1.0 W/cm2) on the gene expression of apoptotic or inflammatory markers, 4 mice (C57BL/6, CLEA Japan, Inc. Tokyo, Japan) were exposed to transcutaneous and transthoracic US for 60 minutes. The hearts, lungs, livers, and kidneys were harvested from these experimental animals as well as 4 control mice without US exposure, and RNA was isolated from each tissue sample. The expression of bax, caspase 3, and IL-6 mRNA were evaluated by real-time polymerase chain reaction (PCR). Online Table 1. Angiographic parameters (60min) tPA TIMI grade mean TIMI grade DDS 0 : n=3 (30%) 1 : n=2 0 : n=8 (80%) 1 : n=2 0 : n=0 (0%) 1 : n=0 (0%) 2 : n=0 (0%) (20%) 2 : n=4 (40%) 3 : n=1 (10%) (20%) 2 : n=0 (0%) 3 : n=0 (0%) 3 : n=10 (100%) 1.30 ± 1.06 ††p<0.01 vs NP, **p<0.01 vs NP NP †† 0.20 ± 0.42 3.00 ** ** Online Figure 1. (A) Illustration of the transthoracic ultrasound (US) device consisting of 4 probes. (B) The left photo shows transthoracic US application in swine. The right fluoroscopic image shows the positioning of the transthoracic US device. Online Figure 2. The US fields in the swine heart as quantified by a catheter-type oscilloscope inserted into the indicated structure under transthoracic US application (continuous wave, 1.0 MHz, and 1.0 W/cm2). Online Figure 3. (A) Coronary angiographic image showing distal balloon occlusion (arrow) for the induction of thrombosis in the left circumflex artery (LCx). (B) Coronary angiographic image showing thrombotic occlusion (arrowhead) in the LCx 30 minutes after distal balloon occlusion. (C) Thrombi obtained from the occluded LCx were strongly immunopositive for GP IIb/IIIa. Online Figure 4. tPA activity of the nanoparticles (NP) before and after 5-minute ultrasound (US) application expressed as the percentage of control tPA (*p<0.05). 20 plasm a tPA activi ty tPA NP+late US * 1 5 10 (g/m l 5 equiv alent) 0 * * 0 5 15 † † * 30 min 45 6 0 Online Figure 5. Time course of plasma tPA activity expressed as the g/ml equivalent of control tPA in rabbit injected with 27,500 IU/kg of tPA or nanoparticles (NP) intravenously. Transcutaneous US application was initiated 40 minutes after NP injection in the cases of NP+late US. Blue arrow indicates the duration of transcutaneous US application in NP+late US. vs tPA at each time points. *p<0.01 vs NP+late US, †p<0.01 Online Figure 6. (A) Typical angiographic images at 60 minutes in rabbits treated with tPA (27,500 IU/kg) alone, nanoparticles (NP) alone, and the drug delivery system (DDS). Arrowheads indicate the proximal site of thrombotic occlusion before treatment. (B) Time course of thrombolysis after injection of tPA (27,500 IU/kg) or nanoparticles (NP) in rabbits treated with tPA alone (▲), NP alone (●), and DDS (■) (*p<0.05 and **p<0.01 vs. tPA alone or NP alone). Online Figure 7. Gene expression of bax, caspase 3, and IL-6 in the heart (A), lung (B), liver (C), and kidney (D) with transcutaneous or transthoracic ultrasound (US) application (white column) or without (black column). Induction of each gene was not observed with US application. Online References 1. Jay SM, Saltzman WM. Controlled delivery of VEGF via modulation of alginate microparticle ionic crosslinking. J Control Release 2009;134:26-34. 2. Jay SM, Shepherd BR, Bertram JP, Pober JS, Saltzman WM. Engineering of multifunctional gels integrating highly efficient growth factor delivery with endothelial cell transplantation. FASEB J 2008;22:2949-56. 3. Uesugi Y, Kawata H, Jo J, Saito Y, Tabata Y. Ultrasound-responsive thrombus treatment with zinc-stabilized gelatin nano-complexes of tissue-type plasminogen activator. J Drug Target 2012;20:224-34. 4. Uesugi Y, Kawata H, Jo J, Saito Y, Tabata Y. An ultrasound-responsive nano delivery system of tissue-type plasminogen activator for thrombolytic therapy. J Control Release 2010;147:269-77. 5. Astrup T, Müllertz S. The fibrin plate method for estimating fibrinolytic activity. Arch Biochem Biophys 1952;40: 34651. 6. Shima M, Nakai H, Scandella D, et al. Common inhibitory effects of human anti-C2 domain inhibitor alloantibodies on factor VIII binding to von Willebrand factor. Br J Haematol 1995;91:714-21. 7. Takayama M, Nogami K, Okuda M, et al. Selective factor VIII and V inactivation by iminodiacetate ion exchange resin through metal ion adsorption. Br J Haematol 2008;142:962-70. 8. Denis C, Methaia N, Frenette PS, et al. A mouse model of severe von Willebrand disease: defects in hemostasis and thrombosis. Proc Natl Acad Sci USA 1998;95:9524-9. 9. von zur Muhlen C, von Elverfeldt D, Moeller JA, et al. Magnetic resonance imaging contrast agent targeted toward activated platelets allows in vivo detection of thrombosis and monitoring of thrombolysis. Circulation 2008;118:258-67. 10. Wilbur DS, Hadley SW, Hylarides MD, et al. Development of a stable radioiodinating reagent to label monoclonal antibodies for radiotherapy of cancer. J Nucl Med 1989;30:216-26. 11. Kawata H, Naya N, Takemoto Y, et al. Ultrasound accelerates thrombolysis of acutely induced platelet-rich thrombi similar to those in acute myocardial infarction. Circ J 2007;71:1643-8. 12. Yamashita A, Furukoji E, Marutsuka K, et al. Increased vascular wall thrombogenicity combined with reduced blood flow promotes occlusive thrombus formation in rabbit femoral artery. Arterioscler Thromb Vasc Biol 2004;24:2420-4. 13. Takemoto Y, Kawata H, Soeda T, et al. Human placental ectonucleoside triphosphate diphosphohydrolase gene transfer via gelatin-coated stents prevents in-stent thrombosis. Arterioscler Thromb Vasc Biol 2009;29:857-62. Online Video 1. A typical coronary angiography at 60 minutes in swine treated with tPA alone (55,000 IU/kg). Online Video 2. A typical coronary angiography at 60 minutes in swine treated with tPA (55,000 IU/kg) followed by transthoracic US application. Online Video 3. A typical coronary angiography at 60 minutes in swine treated with the intelligent drug delivery system (DDS).