Study Guide - American CPR Center
advertisement

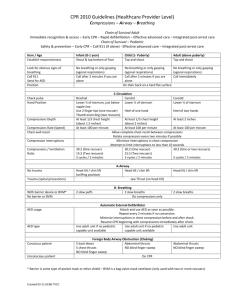
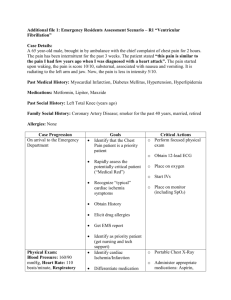
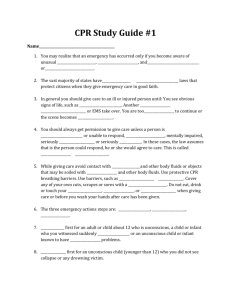
American CPR Center www.505cprstat.com This is a general study guide. If you are confused on this material we strongly recommend purchasing an AHA BLS book Adult CPR Scene Safety: Check your surroundings for danger. If present, leave and call 911, if not present then Check Responsiveness: Shake and Shout. If no response Call 911, if with someone you can send them. If you are alone then leave and call 911. Then C (Circulation): Check the pulse at the carotid artery. Spend 5-10 seconds checking pulse, if one is present, monitor the patients breathing, if not begin chest compressions. Compress at the nipple line, push deep, push hard, and allow the chest to recoil after each compression by taking your weight off of your hands. Cycle: 30 compression and 2 breaths at the rate of 100 minute for 5 rounds making sure to minimize interruption between compressions. Do this for 5 rounds then check the pulse. If no pulse continue CPR, if pulse is present monitor patients breathing A (Airway): Open the airway by head tilt/chin lift method. If you suspect trauma use the Jaw thrust Method. Then B (Breathing): Check for Breathing by look, listening and feeling for breath from the mouth. If the patient is not breathing (or gives an agonal breath) give 2 breaths and look for chest rise. Child CPR (1 year to Puberty) (Check for puberty by looking for armpit hair on men and breast on women, if absent consider the patient to be a child) (Also it is to the rescuers discretion if they choose to use one arm or two in chest compressions, as long as the rescuer compresses deep, fast and recoils off the chest) Scene Safety: Check your surroundings for danger. If present, leave and call 911, if not present then Check Responsiveness: Shake and Shout. If no response call for help or send someone to call 911 but DO NOT leave the child to call 911 until 5 rounds of CPR are done. Then C (Circulation): Check the pulse at the carotid artery. Spend 5-10 seconds checking pulse. If no pulse or pulse is under 60 bpm with signs of poor perfusion then begin chest compressions. Compress at the nipple line, push deep, push hard, and allow the chest to recoil after each compression. Cycle 30 compression and 2 breaths at the rate of a 100 minute for 5 rounds making sure to minimize interruption between compressions. Do this for 5 rounds then if alone call 911. A (Airway): Open the airway by head tilt/chin lift method. If you suspect trauma use the Jaw thrust Method. Then B (Breathing): Check for Breathing by look, listening and feeling for breath from the mouth. If the patient is not breathing give 2 breaths and look for chest rise. Then Infant CPR (Neonate to 1 year) Check for Responsiveness: If not responsive shout for help but if you are alone DO NOT leave the infant until 5 rounds of CPR is performed. C (Circulation): Check the pulse at the brachial artery. If no pulse or pulse is under 60 bpm with signs of poor perfusion then begin chest compressions. Compress at the nipple line, push deep, push hard, and allow the chest to recoil after each compression. Cycle: 30 compression and 2 breaths at the rate of a 100 minute for 5 rounds making sure to minimize interruption between compressions. Do this for 5 rounds then if alone call 911. A (Airway): Open the airway using the head tilt/chin lift being careful not to tilt the head to far back causing the airway to close. B (Breathing): Look, Listen and Feel for breathing, if not breathing give 2 breaths encircling the infant’s nose and mouth with your mouth. Look for chest rise. If the chest does not rise re-tilt and try again. AED (Automated External Defibrillator) Studies show that the AED works best when the patient is shocked immediately and with oxygen in the heart muscle. So if a rescuer witnesses a cardiac arrest then the rescuer should use the AED immediately(knowing that there is oxygen in the heart). If the rescuer did not witness the cardiac arrest then the rescuer should perform 5 rounds of CPR (to provide oxygen to the heart) before using the AED. Scene Safety: Observe the scene is safe and there are no dangers present Check for Responsiveness: Shake and Shout. If no response, Call 911 and acquire an AED (for outside hospital settings, security guards know of their location) C (Circulation): Check the carotid pulse. If no pulse then If the rescuer witnessed the cardiac arrest then use the AED immediately. If the rescuer did not witness the cardiac arrest then perform 5 rounds of CPR then use the AED A (Airway): Open the airway using the head tilt/chin lift. B (Breathing): Look, Listen and Feel for breathing. If not breathing give 2 breaths and look for chest rise. . The goal of the AED is to analyze the heart rhythm to see if it is a shockable rhythm. Many things can interfere with this analysis. For example, if the patient is wearing a necklace then the metal will interfere with the AED. Jewelry should be removed. Medication patch will interfere with the AED. Medication patches should be removed. If the chest is wet it will interfere with the AED. The chest should be dried. Chest hair can interfere with the adhesiveness of the AED pads. Chest hair should be shaved with razor that is stored with the AED. There are 4 basic steps for the AED 1. Power the AED on. 2. Attach the electro pads to the victim’s bare chest. If the chest needs to be shaved, shave it. One pad should be placed just under the right collar bone and the other should be places under the left armpit about one hand width down the rib cage. 3. Clear the victim and let the machine analyze the heart rhythm. If you are touching the patient at this time, the machine will analyze your rhythm rather than the patients. Call out “CLEAR!!” and make sure no one is touching the patient to prevent this. 4. If the AED advises shock, then “CLEAR!!” the patient and shock.(If no shock is advised turn the machine off an begin CPR analyzing the patient ever 5 rounds) After shocking the patient turn the machine off and perform 5 rounds of CPR. This is important because a heart that is just shocked does not perfuse well and needs CPR to assist in perfusion. If the heart rhythm did not convert with the shock then it needs CPR to prepare it for the next shock. In either case the heart needs CPR. Therefore perform 5 rounds immediately after shocking the patient and then check the pulse. If there is a pulse stop CPR and monitor breathing. If not analyze the heart rhythm again and shock if necessary repeating steps 1-4. It’s best to use adult pads on adults and child pads on children, but if not available then adult pads may be used on pediatrics (not infants!). Child pads on adults do not produce enough energy for adult use and not recommended. Choking Adult Conscious If a person is able to talk or is coughing do not interfere with the persons attempt to dislodge the object. Don’t pat on the back, don’t stick you finger in their mouth, just encourage there person to cough it out. If the person is not able to talk or the cough they are producing is a high pitched wheeze then you take action to relieve the choking. To do this you must: Ask if the person is choking saying “Are you choking?” If the person says “Yes I am choking!”, then they are not choking, remember choking people do not talk. If they cannot answer you, then ask “Can I help you?” If you do not ask if you can help, you risk having the patient struggle against your efforts. After the patient gives you consent, stand behind the patient (kneel for children) and wrap your arms around them, locating their belly button. Once you find the belly button make a fist with one hand and cup it with the other. Then in one large “J” motion drive your fist in (to their abdomen) and up (into their diaphragm).This is commonly referred to the Heimlich Maneuver. This movement is a forceful movement. The larger they are, the smaller you are the harder you have to push. You are trying to pop the object out. Repeat this abdominal thrust until you pop the object out or until the patient passes out. The Heimlich maneuver will not work for the obese or pregnant. In this case place your cupped fist on the breastbone (rather than abdomen) and squeeze directly in, performing a chest compression. Unconscious If the person passes out, call 911 and begin the steps of CPR, but look into the airway to see if you can see an object BEFORE you give breaths (otherwise you will blow the object down). By doing CPR you compress the lungs causing the object to pop out into the mouth, by looking into the airway before you give breaths you avoid sending the object back down. Not all the time will you get the object out, but if you get chest rise during your breath then you have an open airway. Infant Choking Conscious Infants will not make the universal distress sign for choking, nor will they answer you when you ask “Are you choking”. So due to the language restraints that bar us from proper communication we are forced to inquire about their choking situation by pinching a toe. When pinching a toe an infant will cry, if the infant doesn’t cry then the airway is being blocked and must be relieved. To do so you must: Take the child onto your arm. Position the infant so that their belly is on your forearm, your hand holds their chin (not the mouth) and their leg is tucked between your bicep and your rib (locking them into place). Then locate their shoulder blades and while holding them upside down slap their shoulder blades (with the base of your hand) 5 times, trying to pop the object out. Then after 5 slaps grab the back of the infants head with your hand and flip the infant onto your other arm and perform 5 chest compressions (at the nipple line) just as you would in CPR. Grab the infants chin again and flip the infant back on to your other arm and perform 5 back slaps. You continue this cycle until the object pops out or the infant passes out. Unconscious If the infant passes out, call 911 and perform the steps of CPR, being careful to look into the airway BEFORE giving breaths (otherwise you will blow the object down). By doing CPR you compress the lungs causing the object to pop out into the mouth, by looking into the airway before you give breaths you avoid sending the object back down. Not all the time will you get the object out, but if you get chest rise during your breath then you have an open airway. Important note: Relieving choking in an infant and adult are both forceful movements that can cause additional injury. Even if the object comes out and the person appears to be fine, call 911. The reason being is that the person can additional injuries and needs to be examined to make sure everything is okay. .