The Dutch College of General Practitioners (NHG) Practice Guideline
advertisement

The Dutch College of General Practitioners (NHG) Practice Guideline
This NHG Practice Guideline is a translation of the Dutch guideline. It is specifically written for Dutch
general practitioners in the Dutch enviroment. The advice which is given may therefore not be in
accordence with the views of general practitioners in other countries.
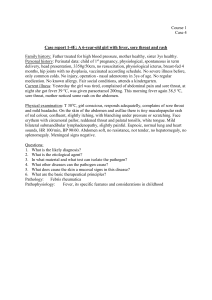
NHG Standard 'Acute sore throat'
(May 1999)
C.F. Dagnelie, S. Zwart, F.A. Balder, A.C.M. Romeijnders, R.M.M. Geijer
The standard and its scientific basis have been updated with respect to the previous
version (Huisarts Wet 1990;33:323-6). The guidelines have been revised. The most
important changes are:
The diagnostics focus on distinguishing between mild and severe throat
infections, and ruling out conditions that increase the risk of complications. The
four clinical features described by Centor [Centor RM, Witherspoon JM, Dalton
HP, et al. The diagnosis of strep throat in adults in the emergency room. Med Dec
Making 1981;1:239-46.] help in determining the severity but are no longer used
explicitly.
In mild throat infections (or a mild form of scarlet fever), patient education is
sufficient.
In severe throat infections (or a severe form of scarlet fever) or when there is an
elevated risk of complications, a narrow-spectrum antibiotic should be used.
The current widely-accepted criterion for referral for tonsillectomy (3 episodes of
tonsillitis in one year) is not well supported; consider referral only if there have
been more than 3 episodes of tonsillitis per year, taking into account the patient's
discomfort.
INTRODUCTION
The NHG Standard 'Acute sore throat' provides guidelines for the diagnosis and treatment
of sore throat of less than 14 days duration. Sore throat caused by trauma or a foreign
body will not be covered, nor will other throat complaints, such as globus sensation or
tickling cough.
Sore throat is a very common complaint and consequently most patients with a sore
throat do not consult the general practitioner.1 2 Those who do usually have an acute
inflammation of the throat caused by micro-organisms. A small minority have a sore
throat due to non-infectious causes, such as repeated clearing of the throat, inhaling dry
air, or smoking.
1
Distinguishing between acute tonsillitis and acute pharyngitis does not affect the
treatment policy, since both involve the same pathogenesis and the inflammation has a
similar clinical course.3
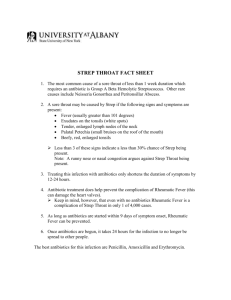
The cause is usually viral, involving one of the many common cold viruses and
sometimes the Epstein-Barr virus.4 The general practitioner will encounter the EpsteinBarr virus only a few times per year.
Bacterial throat infections probably occur more often in the select population that visits
the general practitioner than in the general population. The Group A Beta-Haemolytic
Streptococcus (GABHS) is the most important bacterial cause of throat inflammation.
Streptococci other than those in group A or Haemophilus influenzae play a modest role.5
Consequently, in this standard streptococcus will be synonymous with GABHS. Since the
late 1950s, the number of streptococcal infections with a serious clinical outcome in the
western world has decreased sharply.6 In spite of case histories reported in the
international literature concerning several streptococcal infections with a serious clinical
outcome, there are no indications of an actual increase. Furthermore, in these case
histories the throat was rarely the port of entry.
For purposes of treatment, the standard distinguishes between mild and severe throat
inflammation. Most patients with acute sore throat have a mild (viral or bacterial) throat
inflammation. Severe throat inflammation is uncommon. A severe throat inflammation is
one with severe malaise, intense throat and swallowing complaints, and greatly limited
daily functioning. It is impossible to differentiate with certainty between a bacterial and a
viral cause of the inflammation based on the clinical picture (nor, therefore, based on the
throat's appearance). Like most viral throat infections, a throat infection caused by
streptococci usually has a benign natural course, with spontaneous recovery within 7
days. Abscess formation is infrequent. Since 1998 in the western world, acute rheumatic
fever, acute glomerulonephritis, and Sydenham's chorea have become very rare
complications of a streptococcal throat infection.7 The chance that antibiotics would
prevent these complications is negligible, and about the same as the chance of a severe
anaphylactic response to penicillin.8
The course of scarlet fever also seems to be less severe than it used to be.9 Patients tend
to be less sick and complications are now rare, just as with sore throat. This has made it
less important to use the four clinical features described by Centor to distinguish viral
from bacterial causes. The question of whether or not to prescribe an antibiotic should
depend in particular on the severity of the clinical picture. The last survey of general
practitioners (in 1986) revealed that they prescribed antibiotics for 74% of patients with a
throat infection.10 Frequent prescribing of antibiotics for any and all types of throat
inflammation will only occasionally prevent abscess formation.11 Antibiotics reduce the
duration of symptoms in a streptococcal infection by an average of 1 to 2 days.12 This
limited effect does not reduce absenteeism from work and school, however. The use of
antibiotics also has disadvantages, such as side effects, development of resistance, and
medicalization (promotion of the belief that it deserves medical treatment). Whether the
use of antibiotics leads to multiple recurrences of sore throat is a matter of dispute.13
2
It is therefore recommended that antibiotics not be prescribed for patients with an acute
sore throat unless they are severely ill or have imminent complications or an elevated risk
of a complicated clinical course.14
DIAGNOSTIC GUIDELINES
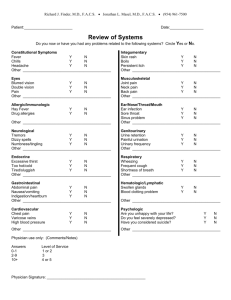
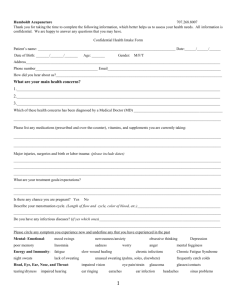
Anamnesis
In a consultation for sore throat (also by telephone), enquire about:
fever (how severe) and the severity of the illness
coughing
painful, enlarged lymph nodes in the neck
difficulty in swallowing or in opening the mouth
the duration of the symptoms and their clinical course, especially: worsening of
the pain, malaise, or swallowing complaints after 4 to 7 days
rash (scarlet fever)
acute rheumatic fever in the patient history
greatly reduced immunity
Telephone advice
In considering telephone advice, the patient should be seen if one or more of the
following are present:
severe malaise and significant limitations in day-to-day functioning
enlarged, tender lymph nodes in the neck
severe difficulties in swallowing or in opening the mouth
abnormal course (worsening of the pain, the malaise, and/or the swallowing
complaints after 4 to 7 days)
rash
acute rheumatic fever in the medical history
greatly reduced resistance, streptococcal epidemics in closed communities of
individuals in fragile health
When none of these is revealed by questioning, advice by telephone is sufficient.
Physical examination
The general practitioner notes the degree of malaise and then examines:
3
the mouth and throat:
o exudate (discharge, pus) on tonsils or pharyngeal wall
o lateral deviation of the uvula or medial deviation of a tonsil, which hinders
opening of the mouth
o erosion or ulceration in the oropharynx, petechiae on the palate (in
infectious mononucleosis)
o the condition of the teeth
the cervical lymph nodes
the skin
If the throat has been sore for more than 7 days or if the clinical course is otherwise
abnormal, the general practitioner should ask additional questions and, in certain cases,
conduct further tests or examinations.
Additional tests
Additional tests, such as a throat culture, antistreptolysin titre (AST), or an
antigen detection test (strep test) are not recommended because they will not alter
the treatment policy. When a throat culture is performed or repeated
measurements of serum AST are made, the delay in obtaining results is usually
too great for them to influence the treatment policy. Results of strep tests are
obtained rapidly but are of limited value because their predictive value for
streptococcal infection is low.15
A leukocyte count and differentiation should be performed when there is
suspicion of:
o infectious mononucleosis
o an immune system disorder such as agranulocytosis (caused by
medication) or leukaemia, as in chronically, seriously ill patients
When the differential white blood cell count is suspect for infectious mononucleosis, a
test for infectious mononucleosis can be added, such as the Paul-Bunnell test, which
measures the presence of heterophil antibodies. Serological tests should be conducted
only if the differential blood count shows the characteristic abnormalities (the laboratory
can perform these tests sequentially using the same blood sample). To reduce the chance
of false-negative results, serological tests should not be performed during the first week
of illness. If the tests are still negative while the blood count suggests infectious
mononucleosis, then cytomegalovirus (CMV) disease and toxoplasmosis must be
considered. For jaundice with infectious mononucleosis, hepatic function tests yield no
additional diagnostic information. In view of the spontaneous recovery from hepatic
function disorders after 5-6 weeks, monitoring these values over the course of the
mononucleosis infection is not meaningful. Furthermore, the clinical picture is a better
parameter for recovery. Only when hepatitis or jaundice occur as the first clinical
manifestation of a mononucleosis infection is there a clear indication for requesting
4
hepatic function tests. Measuring the ALAT level is sufficient in that case, supplemented
with bilirubin in the case of jaundice.16
Evaluation
The distinction between mild and severe throat infections is of primary importance to the
treatment policy. The four clinical features according to Centor help in determining the
severity, but are no longer used explicitly.17 This classification also applies to patients
with scarlet fever.
A sore throat is considered a mild throat infection (or mild form of scarlet fever)
in the event of:
o no severe malaise
o no enlarged, tender cervical lymph nodes
o no severe swallowing problems or problems in opening the mouth
o no abnormal course (no increase in pain, in malaise, and/or swallowing
difficulties after 4 to 7 days)
o no acute rheumatic fever in the medical history
o no signs of sharply reduced immunity
There is an elevated risk of complications in
o patients with greatly reduced immunity, as with indications of an immune
system disorder or treatment for a malignancy;
o patients with acute rheumatic fever in the medical history;
o fragile patients in closed communities during an established streptococcal
epidemic.
The problem is seen as a severe throat infection (or severe form of scarlet fever)
in the event of
o a severely ill patient (exact criteria cannot be given, but examples are
intense throat and swallowing complaints in a previously healthy patient,
significant limitations in day-to-day life due to severe malaise, high fever,
or being bedridden);
o a peritonsillar infiltrate or abscess (probable if there is lateral deviation of
the uvula or medial deviation of a tonsil together with difficulty in opening
the mouth and severe difficulty in swallowing);
o extremely swollen, painful, possibly fluctuating lymph nodes, which could
indicate infectious mononucleosis or the rare abscessing lymphadenitis
colli.
Infectious mononucleosis should be considered in patients (mainly adolescents)
with sore throat, fever, and fatigue and who have been ill for more than 7 days.18
There is usually exudate in the throat, and the lymph nodes in the neck and elsewhere are
painful and swollen. The spleen and liver may be enlarged, and in 5 to 10% of the cases
there is jaundice. Chronic hepatitis or cirrhosis of the liver do not occur as a consequence
of infectious mononucleosis. Petechiae on the palate are suggestive of the disease. The
5
diagnosis is important in order to inform the patient of the benign but sometimes
protracted clinical course. The diagnosis is certain in the presence of absolute and relative
lymphocytosis with at least 20% atypical lymphocytes in the leukocyte differentiation,
and a positive infectious mononucleosis test such as the Paul-Bunnell test. These
serological tests can be false positive and must not be interpreted independent of the other
findings.16
Other causes of sore throat, such as unhealthy habits (smoking, frequent or harsh
clearing of the throat, incorrect use of the voice), mouth breathing, inhaling dry
air or smoke or other irritants, and post-nasal drip should be considered when the
sore throat lasts for more than 7 days and is not accompanied by general illness.
Rare diseases such as herpetic or mycotic or gonococcal pharyngitis, Vincent's
angina, and diphtheria can also be mentioned for the sake of completeness.
TREATMENT POLICY GUIDELINES
Information
For a mild throat infection, the general practitioner (or the trained practice nurse) explains
that a sore throat is usually an unpleasant but harmless illness which spontaneously
disappears within 7 days. Painkillers and rest can be recommended to relieve the
symptoms. When the cause is viral, antibiotics provide no benefit. When the cause is
bacterial, antibiotics reduce the duration of the symptoms by 24 to 48 hours in some adult
patients, without reducing absenteeism from work or school. The chance that antibiotics
would prevent complications is minimal. Antibiotics also have disadvantages, such as
side effects and the development of resistance by bacteria. Consequently, penicillin is not
recommended except in the presence of a severe throat infection or an elevated risk of
complications. If the sore throat lasts for more than 7 days or if the patient becomes
increasingly ill, the patient should contact the general practitioner. When infectious
mononucleosis is confirmed or suspected, the general practitioner should explain the
benign natural course. In a minority of patients the infection leads to chronic fatigue
(weeks to months). It is not highly contagious, so special hygienic measures are not
usually necessary. Testing hepatic function has no benefit, because there is no
relationship between the severity of the disease and the degree of hepatic dysfunction,
and because within 5-6 weeks there is spontaneous recovery from these disorders and
possible jaundice. The level of illness is the best indicator for recovery. There are no
therapeutic options to shorten the time of recovery. Patient mobilization and reactivation
as soon as possible seems to be the best way to limit the dysfunction.
For scarlet fever, the general practitioner should explain that the clinical course is usually
benign and complications are rare. Although the duration of symptoms and the
contagiousness can be reduced by a few days by using antibiotics, treatment is not
necessary in milder cases.
6
For throat irritation, the doctor's advice depends on any eliciting factors, such as clearing
of the throat or smoking. Aphthae heal spontaneously in 10 to 14 days.
Medicinal treatment
A course of antibiotics for 7 days is recommended for patients with:19
a severe throat infection20
peritonsillar infiltrate or abscessing lymphadenitis
scarlet fever with severe malaise
Antibiotic treatment for 10 days (aimed at eradication of the streptococci) is
recommended for patients with21
greatly reduced immunity or acute rheumatic fever in the medical history, as soon
as there is any suspicion of a throat infection with a streptococcus.22 When there
is a potential streptococcal throat infection in the immediate environment of a
patient with a history of acute rheumatic fever, a prophylactic antibiotic course
should be considered. However, no data are available to formulate detailed
guidelines on this point.
a sore throat at the time of an established streptococcal epidemic in closed
communities with persons of fragile health, such as the elderly;
recurrent severe throat infections that do not respond well to 7-day courses of
antibiotics.
The first choice is penicillin V or phenoxymethylpenicillin (500 mg 3 dd). Children under
2 years of age are given penicillin V at a dose of 62.5 mg 3 times daily and children from
2 to 10 years are given penicillin V or phenoxymethylpenicillin at a dose of 250 mg 3 dd.
If the patient is allergic to a narrow-spectrum penicillin, erythromycin is recommended
(in adults 500 mg 4 dd, in children 30 mg/kg/day in 4 doses).23
If despite a 10-day course with a narrow-spectrum penicillin there is a recurrence,
amoxicillin/clavulanic acid could be considered as a second choice (in adults 500/125 mg
3 times daily, in children 20/5 mg/kg/dg in 3 doses) and as third choice, clindamycin (in
adults 300 mg 4 times daily, and in children 40-50 mg/kg/day in 3-4 doses).24
Follow-ups and referral
There is no need to monitor patients with an acute sore throat. It is sufficient to advise
patients to return if the symptoms worsen significantly or if they have not subsided after a
7
week. If there is a peritonsillar infiltrate, the patient should be checked after 1 to 2 days
for possible abscess formation.
When there is a peritonsillar abscess or a rare disease (confirmed or suspected) such as
abscessing lymphadenitis, sepsis, agranulocytosis, or leukaemia, the patient should be
referred.
Tonsillectomy
For recurrent severe throat infections (more than 3 per year), a referral for tonsillectomy
should be considered. However, too little good research has been done concerning the
efficacy of this for well grounded guidelines to be given. With regard to its efficacy,
however, there is not enough good research available to support guidelines. Against the
background of the benign natural course, studies conducted to date support a more
conservative approach than is common practice, in which patients are often referred for
tonsillectomy at 3 throat infections per year. In adults, tonsillectomy is major surgery
with an average sick leave of 14 days.25
note 1
Only 8-15% of patients with sore throat symptoms visit the general practitioner.
1. Bots AW. De keelontsteking in de huisartspraktijk [The sore throat in general
practice]. Leiden: Stenfert Kroese, 1965.
2. Evans CE, McFarlane AH, Norman GR, et al. Sore throat in adults: Who sees a
doctor? Can Fam Physician 1982;28:453-8.
note 2
In the Transition Project, the incidence of acute tonsillitis is 15 per 1,000 patient-years.1
The Continuous Morbidity Registration reports 19 per 1,000 for men and 23-31 per 1,000
for women.2 In a national study, comparable numbers were found for acute tonsillitis,
with a peak in the age category between 15 and 24 years.3 The incidence has declined
inexplicably over the past decades.4
1. Lamberts H. In het huis van de huisarts. Verslag van het Transitieproject [In the
doctor's house.Report on the Transition Project]. Lelystad: Meditekst, 1994.
2. Lisdonk EH, Van den Bosch WJHM, Huygen FJA, Lagro-Jansen ALM. Ziekten in
de huisartspraktijk [Diseases in general practice]. Utrecht: Bunge, 1994.
8
3. Velden J van der, Bakker DH de, Claessen AAMC, Schellevis FG. Een nationale
studie naar ziekten en verrichtingen in de huisartspraktijk [A national study of
diseases and procedures in general practice]. Utrecht: NIVEL, 1991.
4. Ruwaard D, Kramers PGN , eds. Volksgezondheid Toekomst Verkenning. De
gezondheidstoestand van de Nederlandse bevolking in de periode 1950-2010.
[Public Health Future Exploration. The state of health of the Dutch population
during the period 1950-2010]. Rijksinstituut voor Volksgezondheid en Milieu
[National Institute of Public Health and Environment]. The Hague: SDU, 1993.
note 3
In the literature, the term "sore throat" as a presenting complaint is used in the same way
as various clinical profiles such as acute tonsillitis, pharyngitis, and inflammation of the
throat. Similarly, etiological criteria (e.g., streptococcal pharyngitis) and clinical criteria
(e.g., tonsillar exudate) are used interchangeably. Since the mode of diagnosis varies per
country, classification problems arise and morbidity data from different countries are
poorly correlated.
For instance, in the United States, where throat cultures are carried out consistently,
"pharyngitis" (with a positive culture) is synonymous with a streptococcal throat
infection (in this text, "streptococci" is taken to mean group A beta-haemolytic
streptococci). In the Netherlands, the term pharyngitis is used primarily for viral
infections.
The ICHPPC-2 classification uses the following definitions:
I.
II.
III.
Acute upper respiratory tract infection: common cold, nasopharyngitis,
pharyngitis, and rhinitis. Both of the following criteria are required:
a.
signs of acute inflammation of the mucous membranes of the nose and
pharynx;
b.
absence of criteria indicating a more specific and otherwise classified
acute respiratory infection. This does not include influenza or other
specific diseases.
A proven streptococcal infection of the throat meets two of the following criteria:
a.
acute inflammation of the throat
b.
identified Streptococcus pyogenes
c.
increasing AST
The diagnosis of acute tonsillitis requires four of the following criteria:
a.
b.
c.
d.
e.
f.
sore throat
tonsil(s) redder than the posterior pharyngeal wall
pus on the tonsil(s)
swelling of the tonsil(s)
enlarged, tender regional lymph nodes
fever
9
In this standard, as in the literature, "acute sore throat" means both acute pharyngitis and
acute tonsillitis.
Anonymous. ICHPPC-2 defined. International Classification of Health Problems in
Primary Care. Oxford: Oxford University Press, 1983.
note 4
Among others, the coxsackievirus and the respiratory syncytial virus are significant. Both
cause a clinical picture resembling a cold. Pathogens such as Toxoplasma gondii, the
cytomegalovirus, Chlamydia pneumoniae, and Mycoplasma pneumoniae are of limited
significance. Herpetic, mycotic, and gonococcal pharyngitis; Vincent's angina (ulcerative
gingivitis with necrosis and large number of anaerobic bacteria such as Borrelia vincenti)
and diphtheria are rare.1 2 3
1. Bisno AL, Gerber MA, Gwaltney JM, et al. Diagnosis and management of Group
A Streptococcal Pharyngitis: A Practice Guideline. Clin Inf Dis 1997;25:574-83.
2. Komaroff AL, Aronson MD, Pass TM, et al. Serologic evidence of chlamydial and
mycoplasmal pharyngitis in adults. Science 1983;222:927-9.
3. Miller RA, Brancato F, King K, et al. Corynebacterium hemolyticum as a cause of
pharyngitis and scarlatiniform rash in young adults. Ann Intern Med
1986;105:867-72.
note 5
In 70% of a group of 598 patients, aged 4 to 60, with sore throat persisting for less than
14 days, Dagnelie found one or more micro-organisms in the throat culture. In 48% (of
the 598), beta-haemolytic streptococci were cultured, 32% of which were group A
streptococci and 16% of which were other streptococci. Enterobacteria were cultured in
5%, Candida albicans in 5%, Staphylococcus aureus in 4%, and various others in 8%.1
De Meyere found streptococci in 30% of a group of 670 patients aged 5 to 50, with sore
throat persisting for less than 5 days, 27% of which were group A beta-haemolytic
streptococci. Only streptococci were cultured.2 Other micro-organisms play a modest role
in throat inflammation. Streptococci of groups C and G cause no worse a clinical course
than those of group A.3
1. Dagnelie CF, Touw-Otten FWMM, Kuyvenhoven MM, et al. Bacterial flora in
patients presenting with sore throat in Dutch general practice. Fam Practice
1993;10:371-77.
2. De Meyere M. Acute Keelpijn in de eerste lijn. [Acute sore throat in general
practice.] [thesis] Gent: Rijksuniversiteit Gent, 1990.
3. Bisno AL, Gerber MA, Gwaltney JM, et al. Diagnosis and management of
Streptococcal Pharyngitis: A Practice Guideline. Clin In f Dis 1997;25:574-83.
10
note 6
Acute rheumatic fever is a dreaded complication of streptococcal throat infection, due to
the secondary development of cardiac defects. In the United States, the incidence of acute
rheumatic fever has decreased spectacularly, from 25-60 per 100,000 patients per year in
the 1950s to approximately 0.49-1.88 per 100,000 patients per year around 1980. The
incidence is highest (3 per 100,000) in overpopulated cities (especially in poor, black
communities) and lowest (0.49 per 100,000) among "suburban" whites. In developing
countries the incidence is high and comparable to the 1950s level in the western
countries. Although the etiological agent—the streptococcus—is still present, acute
rheumatic fever, as the most dreaded complication, has thus virtually disappeared. The
decline in the incidence had already started before the use of penicillin: improved
hygiene and nutrition and a changing immunopathogenicity of the streptococci seem to
have played a significant role. The role that penicillin played in this decrease is probably
minor.1-6 The incidence of acute glomerulonephritis as a complication has also become
rare, estimated at 1:30,000.7
For the period 1992-1993, a survey was conducted in the Netherlands concerning the
prevalence of invasive infections of group A beta-haemolytic streptococci (GABHS).8
This led to arguments for granting epidemic status, as of early 1992, to severe invasive
infections caused by Streptococcus pyogenes (particularly types T1M1 and T3M3) and
toxic shock syndrome (TSS) in (older) adults. In view of the limited response
(documentation of only 50% of GAS isolates sent in to the RIVM [National Institute of
Public Health and Environment] for typing in the Netherlands in 1.5 years), the clinical
epidemiological data are inconclusive. Among 132 patients with invasive infections, 41
of whom had toxic shock syndrome, a pharyngitis was shown to be a known or potential
port of entry in only 7% of the cases, as in only 2% of the 323 cases in a study in Ontario,
Canada. 9 The TSS complication occurs only occasionally in individuals less than 27
years of age (while it is exactly in the age category of 5-30 years that the exudative
pharyngotonsillitis is seen most often!). In 61% of the patients evaluated, no underlying
chronic disease was reported. Furthermore, Christie rarely found a relationship to sore
throat in 60 patients with GABHS bacteraemia.10 Shulman and Dele Davies, et al.11
confirm the findings of both Schellekens8 and Christie.10 Since mid-1994 the regional
laboratories have carried out an active monitoring programme. According to an oral
report from Schellekens, there seems to have been a stabilization of severe streptococcal
infections in the Netherlands over the past few years, to a level of 1-2 per 100,000
patients per year.
Conclusion: The probable slight increase in invasive streptococcal infections is, at most,
very weakly related to sore throat. There are no indications of an increase in sore throat
from GABHS or of classical complications such as acute rheumatic fever or
glomerulonephritis.
1. Denny Jr FW. A 45-year perspective on the streptococcus and rheumatic fever:
the Edward H. Kass Lecture in infectious disease history. Clin Inf Dis
1994;19:1110-22.
11
2. Del Mar Chr. Managing sore throat: a literature review II. Do antibiotics confer
benefit? Med J Aust 1992;156:644-9.
3. Little P, Williamson I. Sore throat management in general practice. Fam Pract
1996;13:317-21.
4. Howie JGR, Foggo BA. Antibiotics, sore throat and rheumatic fever. J Royal Coll
Gen Pract 1985;35:223-4.
5. De Meyere M. Acute keel pijn in de eerste lijn [Acute sore throat in general
practice]. [thesis] Gent: Rijksuniversiteit Gent, 1990.
6. Markowitz M. The decline of rheumatic fever: Role of medical intervention. J
Pediatr 1985;106:545-50.
7. Taylor JL, Howie JGR. Antibiotics, sore throats and acute nephritis. J Royal Coll
Gen Pract 1983;33:783-86.
8. Schellekens JFP, Schouls LM, Silfhout A, et al. Invasieve infecties door ßhemolytische streptokokken Lancefield groep A (Streptococcus pyogenes, GAS) in
Nederland 1992-1993 [Invasive infections of Lancefield group A ß-haemolytic
streptococci (Streptococcus pyogenes, GAS) in the Netherlands, 1992-1993].
Bilthoven: Rijksinstituut voor Volksgezondheid en Milieu [National Institute of
Public Health and Environment], 1994.
9. Dele Davies H, McGeer A, Schwartz B, et al. Invasive group A streptococcal
infections in Ontario, Canada. New Engl J Med 1996;335:547-54.
10. Christie CD, Havens PL, Shapiro ED. Bacteriemia with group A streptococci in
childhood. Am J Dis Child 1988;142:559-61.
11. Shulman ST. Complications of streptococcal pharyngitis. Pediatr Infect Dis J
1994;13:S70-4.
note 7
A GABHS infection heals—without treatment—within a week. The classic complications
of acute rheumatic fever and glomerulonephritis have become very rare in the western
world.1-6 The incidence of acute rheumatic fever and post-streptococcal
glomerulonephritis is estimated at no more than 1:30,000 cases of sore throat.7,8
According to Hoogendoorn, it has decreased throughout the Dutch population to below
1:100,000 per year.9
1. Brink WR, Rammelkamp CH, Denny FW, Wannamaker LW. Effect of penicillin
and aureomycin on the natural course of streptococcal tonsillitis and pharyngitis.
Am J Med 1951:300-8.
2. Dagnelie CF. Sore throat in general practice [thesis]. Utrecht: Rijksuniversiteit
Utrecht, 1993.
3. De Meyere M. Acute keelpijn in de eerste lijn [Acute sore throat in general
practice]. [thesis] Gent: Rijksuniversiteit Gent, 1990.
4. Del Mar C. Managing sore throat: a literature review. Med J Aust 1992;156:6449.
5. Little P, Williamson I. Sore throat management in general practice. Fam Pract
1996;13:317-21.
12
6. Little P, Gould C, Williamson I, et al. Reattendance and complications in a
randomised trial of prescribing strategies for sore throat: the medicalising effect
of prescribing antibiotics. BMJ 1997;315:350-2.
7. Howie JGR, Foggo BA. Antibiotics, sore throat and rheumatic fever. J Royal Coll
Gen Pract 1985;35:223-4.
8. Taylor JL, Howie JGR. Antibiotics, sore throat and acute nephritis. J Royal Coll
Gen Pract 1983;33:783-6.
9. Hoogendoorn D. Acuut reuma en acute glomerulonefritis; huidige klinische
incidentie en de sterfte in Nederland [Acute rheumatic fever and acute
glomerulonephritis; current clinical incidence and mortality in the Netherlands].
Ned Tijdschr Geneesk 1989;133:2334-8.
note 8
Theoretically, for a sore throat with a positive streptococcus culture, penicillin would
reduce the risk of complications from acute rheumatic fever by 10-25%, so that the risk
of acute rheumatic fever would decline from less than 1:30,000 to 1:40,000.1-3 In
practice, however, that effect would be impossible to achieve; most patients with sore
throat do not consult a doctor. In the Evans study, only 8% of all sore throat patients went
to the doctor, while 8% telephoned for advice.4 Valkenburg et al. found that just 9% of
the patients with a streptococcal throat infection went to the general practitioner. In
patients who develop acute rheumatic fever or glomerulonephritis, the sore throat may be
insignificant or—in 1/3—absent.5 Sore throat patients who have acute tonsillitis or
pharyngitis are in the minority. 6
When the throat culture is positive in a patient with a sore throat, it is not easy to
distinguish the non-pathogenic, incidental presence of streptococci (carrier) from the
pathogenic presence, just from the throat culture. Even the repeated measurement of the
antistreptolysin titre does not eliminate this ambiguity. In two general practice studies,
there was insufficient titre increase in 54 and 66% of the positive throat cultures.7 8 Based
on a theoretical mathematical model, Van der Does postulates that 1 million patients
would have to take antibiotics for 10 days to potentially prevent 2 cases of acute
rheumatic fever. 9
Conclusion: The incidence of acute rheumatic fever has become so low in the western
world that the use of penicillin to prevent this complication can now scarcely be
considered significant.7 8 10 11 Glomerulonephritis has a similar incidence; the studies
available contain no evidence that penicillin prevents this disease.11 12
1. Denny FW, Wannamaker LW, Brink WR, et al. Prevention of rheumatic fever.
Treatment of the preceding streptococcus infection. JAMA 1950;143:151-3.
2. Tompkins RK., Burnes DC, Cable WE. An analysis of the cost-effectiveness of
pharyngitis management and acute rheumatic fever prevention. Ann Int Med
1977;86:481-92.
3. Howie JGR, Foggo BA. Antibiotics, sore throat and rheumatic fever. J Royal Coll
Gen Pract 1985;35:223-4.
13
4. Evans CE, McFarlane AH, Norman GR, et al. Sore throat in adults: Who sees a
doctor? Can Fam Phys 1982;28:453-8.
5. Valkenburg HA, Haverkorn MJ, Goslings WRO, et al. Streptococcal pharyngitis
in general population. II. The attack rate of rheumatic fever and acute
glomerulonephritis in patients not treated with penicillin. J Infect Dis
1971;124:348-58.
6. Lamberts H, Wood M , eds. ICPC: International Classification of Primary care.
Oxford: Oxford University Press, 1987.
7. Dagnelie CF. Sore throat in general practice [thesis]. Utrecht: Universiteit
Utrecht, 1994.
8. De Meyere M. Acute keelpijn in de eerste lijn [Acute sore throat in general
practice] [thesis]. Gent: Rijksuniversiteit Gent, 1990.
9. Van der Does E, Masurel N. Acute virale infecties [Acute viral infections]. Alphen
a/d Rijn: Samson Stafleu, 1988.
10. Del Mar C. Managing sore throat: a literature review. Med J Aust 1992;156:6449.
11. Little P, Williamson I. Sore throat management in general practice. Fam Practice
1996;13:317-21.
12. Taylor JL, Howie JGR. Antibiotics, sore throat and acute nephritis. J Royal Coll
Gen Pract 1983;33:783-6.
note 9
Van de Lisdonk EH, Van den Bosch WJHM, Huygen FJA, Lagro-Jansen ALM. Ziekten in
de huisartspraktijk [Diseases in general practice]. Utrecht; Bunge, 1994.
note 10
Based upon the NIVEL study (with data from 1986) it was calculated that general
practitioners prescribed antibiotics in 74% of the cases, 92% of the prescriptions being
for penicillin. More recent data are not available.
De Melker RA, Kuyvenhoven MM. Management of upper respiratory tract infections in
Dutch family practice. J Fam Practice 1994;38:353-7.
note 11
The estimated incidence of peritonsillar abscess is 1 in 150-200 cases of sore throat. In
his 1950 study of general practice, Bennike saw abscesses develop in 5% of his placebotreated group.1 Dagnelie found 2 abscesses in the placebo group (1.7%) and one patient
with an imminent abscess during penicillin treatment (0.8%, not significant).2 In an
English population of 8,000 general practice patients, imminent throat abscess was
14
observed on 14 occasions in 5 years. Only 3 patients had gone to the doctor in advance
with sore throat symptoms.3 The Cochrane analysis gives a relative risk of 0.19 (95% CI
0.08-0.47) for an abscess under penicillin therapy compared to placebo.4 The absolute
risk is not stated. In spite of a declining trend, peritonsillar abscess accounted for 1,152
hospital admissions in the Netherlands in 1987. It is not known how many peritonsillar
abscesses are treated by general practitioners and how many by specialists in outpatient
clinics.5 Abscessing lymphadenitis is rare. In one study, 3 cases of severe lymphadenitis
colli were reported in approximately 6,000 sore throat episodes.6
Conclusion: The incidence of abscesses is estimated to be low: 1 per 150-200; during
placebo treatment in Dutch studies it was near 1%. Usually the diagnosis of imminent
abscess is made during the initial consultation. The chances of an abscess developing
when there is a mild sore throat are minimal.
1. Bennike T, Brøchner-Mortensen K, Kjær E, et al. Penicillin Therapy in Acute
Tonsillitis, Phlegmonous Tonsillitis and Ulcerative Tonsillitis. Acta Scand
1951;139:253-73.
2. Dagnelie CF. Sore throat in general practice [thesis]. Utrecht: Universiteit
Utrecht, 1994.
3. Little P, Williamson I. Sore throat management in general practice. Fam Practice
1996;13:317-21.
4. Del Mar CB, Glasziou PP. Abstract of review: Antibiotics for the symptoms and
complications of sore throat. Oxford: The Cochrane library, 1998.
5. SIG, gegevens uit de Landelijke Medische Registratie van klinische opnamen in
short-stay-ziekenhuizen 1981 t/m 1987 [SIG, data from the National Medical
Record of clinical admissions to short-stay hospitals, 1981 to 1987].
6. Fry J. Acute throat infections. Update 1979;18:1181-3.
note 12
In three older studies on the effect of penicillin in general practice, a 24-hour (or less)
shortening of the duration of illness was found, usually in GABHS-positive populations,
sometimes in GABHS-negative populations.1-3 Dagnelie and De Meyere found in their
double-blind, randomized, general practice studies that only GABHS-positive patients
(32 and 27%, respectively) benefited from penicillin, with a 24-hour reduction in the
duration of illness.4,5 In an open, randomized study, Little found only marginal
improvement from antibiotics.6 It should be noted that severely ill patients were not
admitted into the latter study. (Upon inquiry, Little estimated the number to be no more
than 5%; these were mainly severely ill, bedridden patients.) According to a recent
review, antibiotics reduce the duration of symptoms by about half a day.7
In a double-blind study involving 239 patients aged 4 to 60 years with a sore throat of
less than 14 days duration and three or four Centor criteria, Dagnelie et al. found no
difference in work resumption between penicillin treatment or placebo.4 Eight percent of
the patients were excluded because in the doctor's assessment there was an absolute
indication for penicillin (imminent abscess, comorbidity requiring antibiotics, or reduced
15
immunity). In the untreated group, 2 throat abscesses occurred, compared to none in the
treated group (statistically insignificant). In the penicillin group, 31% still had throat
symptoms after 2 days (placebo group 49%). Only in patients with a subsequent positive
GABHS culture (46%) was an effect from penicillin observed: 21 of 117 patients
benefited by recovering 1 to 2 days sooner, with no difference in sick leave or work
absenteeism. After 2 days GABHS was still evident in 4% of the penicillin group,
compared to 75% of the control group.
In a group of 613 patients (with 173 GABHS-positive patients, 84 treated with penicillin
and 89 with placebo), De Meyere found a significant effect in the GABHS group only if
penicillin treatment was initiated within 48 hours of the onset of symptoms.5 All
GABHS-positive patients recovered with penicillin 24 hours earlier. The reduction in
symptoms was already easy to measure after 24-48 hours, but on the fifth day there was
no further difference from the placebo group. Here, too, no significant difference in work
absenteeism or complications was found. Patients were excluded if, amongst other things,
they had had a sore throat for more than 5 days or were at high risk.
Little et al. conducted an open, randomised study among 716 patients over 4 years of age
with sore throat and at least exudate in the throat, a red pharynx or tonsils, or swollen
neck lymph nodes.6 This design was deliberately chosen to mimic the situation in general
practice as closely as possible. Children did not have to complain of a sore throat per se;
inclusion occurred even if the symptoms were mentioned in passing. Eighty-four percent
had tonsillitis or pharyngitis. Penicillin was given to 246 patients for 10 days, while 230
just received detailed written information on the clinical course and the symptoms, and
238 just a prescription for penicillin stating that the medication could be picked up if
there was no improvement after 3 days (69% of this group did not take any penicillin).
No difference was found in illness, work absenteeism or satisfaction on day 3. In most
patients with sore throat, antibiotics only marginally improved the elimination of
symptoms: the clinical course and the impact of symptoms were not affected. In a
Cochrane review, a total of 10,484 cases of sore throat were studied, but prior selection
using the Centor criteria did not always occur, which would influence the results.7
Conclusion: For some patients with acute sore throat, penicillin reduced the duration of
illness by 1 to 2 days. This limited effectiveness is partly related to problems with respect
to the accurate selection of patients who can benefit from penicillin. The presence of
streptococci in patients with an acute sore throat does not mean the streptococci are the
cause. Moreover, clinical symptoms, a throat culture, a strep test, or AST titre can be
used within a limited time period to validate the diagnosis of a sore throat due to group A
ß-haemolytic streptococci. Severely ill patients and patients with imminent complications
or reduced resistance are excluded from most studies, based on the physician’s
assessment.
1. Whitfield MJ, Hughes AO. Penicillin in acute sore throat. Practitioner
1981;225:234-9.
2. Randolph MF, Gerber MA, De Meo KK, et al. Effect of antibiotic therapy on the
clinical course of streptococcal pharyngitis. J Pediatr 1985;106:870-5.
16
3. Haverkorn MJ, Valkenburg HA, Goslings WRO. Streptococcal pharyngitis in the
general population. I. A controlled study of streptococcal pharyngitis and its
complications in the Netherlands. J Inf Dis 1971;124:339-47.
4. Dagnelie CF, Van der Graaf Y, De Melker RA, Touw Otten FWMM. Do patients
with sore throat benefit from penicillin? A Randomized double-blind placebocontrolled clinical trial with penicillin V in general practice. Br J Gen Pract
1996;46:589-93.
5. De Meyere M. Acute keelpijn in de eerste lijn [Acute sore throat in general
practice] [thesis]. Gent: Rijksuniversiteit Gent, 1990.
6. Little P, Williamson I, Warner G, et al. Open randomised trial of prescribing
strategies in managing sore throat. BMJ 1997;314:722-7.
7. Del Mar CB, Glasziou PP. Abstract of review: Antibiotics for the symptoms and
complications of sore throat. Oxford: The Cochrane Library, 1998.
note 13
Disadvantages of the use of penicillin are:
allergic reactions, the risk being approximately 1 to 2%. An anaphylactic reaction
occurs in 10 to 40 per 100,000 intramuscular administrations, with a resultant risk
of death of 2 per 100,000. With oral administration the reactions are less frequent
and less violent;1-6
selection of resistant micro-organisms, especially when broad spectrum
antibiotics are used;7-9
potentially reduced rise in specific antibodies, particularly in children; 9 10
increased chance of a recurrence: three studies compared immediate treatment
with penicillin to a 2-day delayed treatment. Immediate treatment was found to
increase the rate of recurrence by 20%;10-12
medicalizing effect: prescribing antibiotics increases the probability of a
consultation in the event of a recurrence of sore throat symptoms.13
1. Haverkorn MJ, Valkenburg HA, Goslings WRO. Streptococcal pharyngitis in the
general population. I. A controlled study of streptococcal pharyngitis and its
complications in the Netherlands. J Inf Dis 1971;124:339-47.
2. Anonymus. Continue morbiditeitsregistratie peilstations [Continuous Morbidity
Registration Sentinel Stations]. Utrecht: Nederlands Huisartsen Instituut, 1983.
3. Idsoe O, Guthe T, Willcox RR et al. Nature and extent of penicillin side-reactions
with particular reference to fatalities from anaphylactic shock. WHO Bull
1968;38:159-88.
4. Young E. Allergie voor penicilline [Penicillin allergy]. Ned Tijdschr Geneeskd
1985;129:1713-6.
5. Erffmeyer JE. Adverse reactions to penicillin. A review. Ann of Allergy
1981;47:288-300.
6. Del Mar Chr. Managing sore throat: a literature review. Med J Austr
1992;156:644-9.
17
7. Arason VA, Kristinson KG, Sigurdsson JA, et al. Do antimicrobials increase the
carriage rate of penicilline resistant pneumococci in children? Cross sectional
prevalence study. BMJ 1996;313:387-91.
8. Lacey RW. DNA in Medicine. Evolution of microorganisms and antibiotic
resistance. Lancet 1984;2:1022-5.
9. Komaroff AL. A management strategy for sore throat. JAMA 1978;239:1429-32.
10. Pichichero ME, Disney FA, Talpey WB, et al. Adverse and beneficial effects of
immediate treatment of group A beta-hemolytic streptococcal pharyngitis with
penicillin. Pediatr Infect Dis J 1987;6:635-43.
11. El-Daher N, Hijazi S, Rawasdeh N, et al. Immediate versus delayed treatment of
group A beta-hemolytic streptococcal pharyngitis with penicillin-V. Ped Inf Dis J
1991;10:126-30.
12. Gerber M, Randolph M, Demeo K, Kaplan E. Lack of impact of early antibiotic
therapy for streptococal pharyngitis on recurrence rates. J Pediatr
1990;117:853-8.
13. Little P, Gould C, Williamson I, et al. Reattendance and complications in a
randomised trial of prescribing strategies for sore throat: the medicalising effect
of prescribing antibiotics. BMJ 1997;315:350-2.
note 14
When penicillin is prescribed, usually one of the following is intended: to reduce the
duration of illness or accelerate eradication of symptoms; to prevent abscess formation,
acute rheumatic fever, and glomerulonephritis; or to eradicate GABHS in the throat more
rapidly, with the aim of reducing and curtailing the danger of infection within 24 hours.
In the decision analysis by Touw-Otten et al., in which a higher risk of recurrence was
not considered, the conclusion was: in a patient without elevated risk, who has had a sore
throat for less than 48 hours, a narrow-spectrum penicillin taken orally should be
considered if the four Centor clinical criteria are present. If three criteria are present, a
rapid strep test could be performed, after which penicillin is only given if the result of the
strep test is positive. If no strep test is available, symptomatic therapy is preferred.
Antibiotic therapy not indicated when there are less than three criteria, nor in the case of
a sore throat that has lasted more than 48 hours, unless in a patient at an elevated risk.1
De Meyere is of the opinion that the benefits do not outweigh the numerous, at times
serious, adverse effects.2 Little claims that the chance that a general practitioner would
cause a fatal anaphylactic response in the course of his career by treating every acute sore
throat with penicillin (estimated to be 1 in 3 to 1 in 14) is equal to the chance of seeing a
patient who develops glomerulonephritis or acute rheumatic fever after a sore throat.3 Del
Mar states that the frequency of acute rheumatic fever is too low, protection against
abscesses too marginal, and the reduction of symptoms in sore throat too minimal to
justify the use of antibiotics.4 5
18
In addition, treatment with antibiotics is indicated at an earlier stage in patients with sore
throat who are at an elevated risk due to sharply reduced resistance or acute rheumatic
fever in the history (if those patients are not already taking prophylactic antibiotics).
1. Touw-Otten F, De Melker RA, Dippel DWJ, et al. Antibioticabeleid bij tonsillitis
acuta door de huisarts; een besliskundige analyse [Antibiotic treatment policy for
acute tonsillitis in general practice; a decision analysis]. Ned Tijdschr Geneeskd
1988;132:1743-8.
2. De Meyere M. Acute keelpijn in de eerste lijn [Acute sore throat in general
practice] [thesis]. Gent: Rijksuniversiteit Gent, 1990.
3. Little P, Williamson I. Sore throat management in general practice. Fam Pract
1996;13:317-21.
4. Del Mar Chr. Managing sore throat: a literature review. Med J Aust
1992;156:644-9.
5. Del Mar CB, Glasziou PP. Abstract of review: Antibiotics for the symptoms and
complications of sore throat. Oxford: The Cochrane Library, 1998.
note 15
In the antigen detection test (strep test), streptococci can be detected within 5 to 20
minutes by means of an enzyme-linked immune response. The sensitivity of the strep test
compared to the throat culture has varied in different patient populations from 44 to 96%,
with a mean of about 80%. The positive predictive value is over 90%.1 In Dagnelie's
study, in all patients, the sensitivity of the strep test was 65%, the specificity 96%, the
positive predictive value 88%, and the negative predictive value 85%, with the throat
culture as the golden standard.2 In the group of sore throat patients who had three or four
Centor criteria, the sensitivity of the strep test was 75% compared to the throat culture.2
Considering those characteristics, the strep test has some added (albeit limited) value
after clinical selection using the Centor criteria. Specifically, despite clinical indications
for the use of antibiotics, a negative test further supports a conservative approach to
antibiotic use. Precise determination of the value is difficult, due to the limits of both a
throat culture and increasing antistreptolysin titres (see below). There are new rapid tests
available.4 Their value has not yet been adequately demonstrated.5 If penicillin use is
being considered in a patient with the four Centor criteria, the patient and the general
practitioner will primarily be interested in the chance of shortening the course of the
disease by use of penicillin and not so much interested in the possibility of prescribing
penicillin wrongly. Several studies found that penicillin was often prescribed even when
the strep test was negative. Apparently, given the chances of a false negative test, clinical
considerations were the deciding factor in the decision to fight a potential streptococcal
infection anyway, in spite of the low possibility.1 6 7
The throat culture is no gold standard for a streptococcal infection: there is a
streptococcal carrier state, in which there is no relationship between the presence of
streptococci in the culture and sore throat symptoms (in approximately 10% of the
population); furthermore, about 10% of the throat cultures are false negative. Newer
culturing techniques may have more validity.
19
Even increased antistreptolysin titres (AST) are no longer seen as the gold standard.
When the throat culture is positive, only about half of patients show an increase in the
antistreptolysin titres. Treatment with penicillin can suppress the AST increase, and when
the interval between the measurements is too short, a possible increase in the antibody
titres may not be measurable. Although an increase in antibody titres is no longer the gold
standard, there is no agreement on a different standard.2,8 With these limitations, a strep
test adds too little to justify its introduction into general practice. Moreover, extra
diagnostics can raise false expectations, causing patients to come back sooner.
1. De Meyere M. Acute keelpijn in de eerste lijn [Acute sore throat in general
practice] [thesis]. Gent; Rijksuniversiteit Gent, 1990.
2. Dagnelie CF, Bartelink ML, van der Graaf Y, et al. Towards a better diagnosis of
throat infections (with group A ß-haemolytic streptococcus in general practice. Br
J Gen Pract 1998;48:959-962.
3. True BL, Carter BL, Driscoll CE, et al. Effect of a rapid diagnostic method on
prescribing patterns and ordering of throat cultures for streptococcal pharyngitis.
J Fam Pract 1986;23:215-9.
4. Gerber MA, Tanz RR, Kabat W, et al. Optical immunoassay (O.I.A.) for group A
ß-hemolytic streptococcal pharyngitis. JAMA 1997;277:899-903.
5. Bisno AL, Gerber MA, Gwaltney JM. Diagnosis and management of group A
streptococcal Pharyngitis: a practice guideline. Clin Inf Dis 1997;25:574-83.
6. Dagnelie CF, De Melker RA, Touw-Otten F. Wat heeft een streptest huisartsen te
bieden? Toepassing van de streptest tijdens de testfase van het keelpijnprotocol
[What can a strep test offer to general practitioners? Use of the strep test during
the test phase of a sore throat protocol]. Huisarts Wet 1989;32:407-11.
7. Burke P, Bain J, Cowes A, Athersuch R. Rational decisions in managing sore
throat: evaluation of a rapid test. BMJ 1988;296:1646-9.
8. Gerber MA, Randolph MF, Mayo DR. The group A streptococcal carrier state. A
reexamination. Am J Dis Child 1988;142:562.
note 16
A Paul-Bunnell reaction gives the greatest certainty, but the antibodies are not always
detectable: in the first week of illness, the chance of a negative test is 60% and in the
second week it is still 20%. False positive reactions also occur.1
Almost all patients with mononucleosis have slight liver dysfunction, and 5-10% have
jaundice. The general practitioner often requests hepatic function tests.2 There is no
correlation between the severity of the symptoms and the degree of liver dysfunction. The
liver dysfunction always heals spontaneously after 5 to 6 weeks, with the peak of the
abnormalities in the tests usually occurring in the second week. Chronic hepatitis or
cirrhosis of the liver do not occur as a result of infectious mononucleosis.3
1. Schellekens JWG. Mononucleosis infectiosa (Uit de serie Huisartsgeneeskundige
conferenties) [Infectious mononucleosis (From the series: General Practice
Conferences)]. Huisarts Wet 1980;23:189-92.
20
2. Zaat JOM, Schellevis FG, Van Eijk JthM, Van der Velden J.
Laboratoriumonderzoek bij klachten over moeheid. In: Zaat JOM. De macht der
gewoonte; over de huisarts en zijn laboratoriumonderzoek [Laboratory research
for fatigue complaints. In: Zaat JOM. The power of habit: on general
practitioners and their laboratory tests] [thesis]. Amsterdam: Vrije Universiteit,
1991.
3. Drenth JPH, Pop P, Van Leer JVM. Diagnostiek van mononucleosis infectiosa
[The diagnosis of infectious mononucleosis]. Practitioner (Ned) 1988:361-6.
note 17
Centor analysed 14 characteristics for the degree to which they contributed to the
diagnosis of streptococcal throat infection in 286 adults visiting a Casualty Department
with the complaint of a sore throat. Four appeared to be significant: (recent) fever,
tonsillar exudate, swollen and tender anterior cervical lymph nodes, and the absence of a
cough. The chance of a positive throat culture proved to be 56% if all four of these
characteristics were present, 32% if three were present, and 15% if two were present.
Hence the presence of these four "classic" characteristics does not confirm the diagnosis
of a streptococcal infection.1 In children under 15 years of age, the same characteristics
proved to be irrelevant with regard to the possibility of a streptococcal infection. In this
age group, the chance of a streptococcal carrier state is much higher than in adults. Under
4 years of age, the symptoms are often more vague and streptococcal infections occur
less frequently.2 3 4
Conclusions:
A viral infection is probable when there is coughing and/or a duration of greater
than seven days in combination with fever and malaise.
The chance of streptococci being found is about 50% in the presence of all four
Centor criteria: absence of cough, fever ³38.5oC (rectally), swollen and tender
lymph nodes in front of the sternocleidomastoid muscle, and exudate in the throat.
In sore throat patients under 15 years of age, the chance of streptococci being
present in the throat is about 50%, regardless of other attendant clinical
symptoms.
1. Centor RM, Witherspoon JM, Dalton HP, et al. The diagnosis of strep throat in
adults in the emergency room. Med Dec Making 1981;1:239-46.
2. Breese BB. A simple scorecard for the tentative diagnosis of streptococcal
pharyngitis. Am J Child Dis 1977;131:514-7.
3. Dagnelie CF. Sore throat in general practice [thesis]. Utrecht: Universiteit
Utrecht, 1994.
4. De Meyere M. Acute keelpijn in de eerste lijn [Acute sore throat in general
practice] [thesis]. Gent: Rijksuniversiteit Gent, 1990.
note 18
21
In adolescents with a sore throat persisting for more than 7 days together with fever,
fatigue, and swollen lymph nodes, infectious mononucleosis should be considered.1 2
Infectious mononucleosis occurs in an average of 1 per 1,000 patients per year,
particularly in adolescents and young adults, and somewhat more often in women. The
infection only rarely occurs in two or more family members at the same time, so it has a
relatively low contagiousness. In children, infectious mononucleosis usually results in an
atypical viral clinical picture.3 4 Extremely rarely, complications such as
encephalomeningitis and ruptured spleen can occur.3-6
1. Schellekens JWG. Mononucleosis infectiosa (Uit de serie Huisartsgeneeskundige
conferenties) [Infectious mononucleosis (From the series: General Practice
Conferences)]. Huisarts Wet 1980;23:189-92.
2. McSherry JA. Diagnosing infectious mononucleosis: avoiding the pitfalls. Can
Fam Physician 1985;31:1527-9.
3. Van de Lisdonk EH, Van den Bosch WJHM, Huygen FJA, Lagro-Jansen ALM.
Ziekten in de huisartspraktijk [Diseases in general practice]. Utrecht: Bunge,
1994.
4. Sutton RNP. Clinical aspects of infection with the Epstein-Barr virus. J R Coll
Physicians Lond 1975;9:120-8.
5. Domachowske JB, Cunningham CK, Cummings DL, et al. Acute manifestations
and neurologic sequelae of Epstein-Barr virus encephalitis in children. Pediatr
Infect Dis J 1996;15:871-5. 4.
6. Connelly KP, DeWitt D. Neurologic complications of infectious mononucleosis.
Pediatr Neurol 1994;10:181-4.
note 19
In 1953 the American Heart Association Council on Rheumatic Fever and Congenital
Heart Disease recommended that oral penicillin be prescribed for 10 days in the presence
of a proven streptococcal throat infection. This recommendation was based on various
studies showing that after a 5-day course of treatment, more bacteria remain present in
the throat than after a 10-day course.1 2 These findings were confirmed in prospective
studies, which additionally showed that the clinical symptoms returned more often after a
7-day course than after a 10-day course.3-5
The standard distinguishes between a 7-day and a 10-day course of antibiotics. If such a
course is intended, then a 7-day course will be sufficient to bring about clinical recovery.
If specific prevention of the classic complication acute rheumatic fever is intended, then,
in theory, eradication of streptococci by means of a 10-day course is the best way to
achieve that goal.
1. Breese BB, Bellows MT, Fischel EE. Prevention of rheumatic fever. Statements of
American Heart Association council on rheumatic fever and congenital heart
disease. JAMA 1953;151:141-3.
22
2. Wannamaker LW, Denny FW, Perry WD, et al. The effect of penicillin
prophylaxis on streptococcal disease rates and the carrier state. N Engl J Med
1953;249:1-7.
3. Schwartz RH, Wientzen RL, Pereira F et al. Penicillin V for group A
streptococcal pharyngotonsillitis. A randomized trial of seven vs. ten days'
therapy. JAMA 1981;246:1790-5.
4. Gerber MA, Randolph MF, Chanatry J, et al. Five vs ten days of penicillin V
therapy for streptococcal pharyngitis. Am J Dis Child 1987;141:224-7.
5. Kaplan EL. The group A streptococcal upper respiratory tract carrier state: an
enigma. J Pediatr 1980;97:337-45.
note 20
Severely ill patients are excluded from most trials and treated with penicillin. A precise
description of this group of severely ill patients is not given (see note 12). It is therefore
unknown precisely how significant the effect of penicillin in this - poorly described group is. The risk of purulent complications seems greater, and the need to reduce
symptoms is evident. Therefore, the committee is of the opinion that curative and
prophylactic treatment is indicated for patients with a severe throat infection.
note 21
The endocarditis prophylaxis is specifically aimed at preventing infection by
Streptococcus viridans in interventions on patients with heart valve insufficiencies and a
previous history of endocarditis. Yet there is no relationship between throat infections
and endocarditis from Streptococcus viridans. Fever in and of itself is not an indication
for administering antimicrobial therapy.1
In patients with artificial joints and a 'significant risk' of bacteraemia, for example in
(skin) infections in the same extremity, antibiotic prophylaxis for bacterial arthritis is
recommended by the professional groups. Kaandorp's study found that the chances of
complications from antibiotic treatment could be greater than the chance of a bacterial
infection from the artificial joint. There is limited efficacy, particularly for skin infections
in patients who also have the following characteristics: an artificial joint, rheumatoid
arthritis, age over 80 years, and an additional disease such as diabetes mellitus or cancer.
With regard to throat infections, the efficacy is even less. Furthermore, throat infections
from streptococci are rare in individuals over 65 years of age.2 The general practitioner
will always consider prophylaxis with antibiotics when (rare) clustering of the
aforementioned risk factors occurs, based on the diabetes mellitus and advanced age. In
patients with an artificial joint and a bacterial skin infection, there are arguments for
administering prophylaxis; in patients with an artificial joint and a throat infection, there
is too little support to recommend prophylactic antibiotics. 2
23
1. Anonymous. Preventie bacteriële endocarditis [Prevention of bacterial
endocarditis]. Revised publication February 1996. The Hague: De Nederlandse
Hartstichting {Dutch Heart Foundation], 1996.
2. Kaandorp CJE. Prevention of bacterial arthritis [thesis]. Amsterdam: Vrije
Universiteit Amsterdam, 1998.
note 22
The decision to give antibiotics in the event of any suspicion of a streptococcal infection
is based on a consensus within the committee; no information on this was found in the
literature.
note 23
Until now, the superiority of other antibiotics, such as the cephalosporins, has not been
proved conclusively. Penicillin has been demonstrated to be effective, relatively safe, and
inexpensive, and has a narrow spectrum. When there is a narrow-spectrum penicillin
allergy, a macrolide such as erythromycin can be prescribed, based on the activity
spectrum.1 2
1. Bisno AL, Gerber MA, Gwaltney JM, et al. Diagnosis and management of group
A streptococcal pharyngitis: a practice guideline. Clin Inf Dis 1997 25:574-83.
2. Pichichero ME, Disney FA, Talpey WB, et al. Adverse and beneficial effects of
immediate treatment of group A beta-hemolytic streptococcal pharyngitis with
penicillin. Pediatr Infect Dis J 1987;6:635-43.
note 24
Most studies on recurrent throat infections assume 10 days of treatment with antibiotics,
aimed at eradication.1-3 There are no well-controlled comparative studies on the
effectiveness of amoxicillin/clavulanic acid and other antibiotics. There are, however,
indications that ß-lactamase-producing strains of anaerobic bacteria sometimes protect
the Streptococcus pyogenes against penicillin, and amoxicillin/clavulanic acid is effective
against this. Where a clinical basis is lacking, there is some consensus in the literature for
using clindamycin as third choice, in view of its effectiveness for eradication.1 4
1. Bisno AL, Gerber MA, Gwaltney JM, et al. Diagnosis and management of group
A streptococcal pharyngitis: a practice guideline. Clin Inf Dis 1997;25:574-83.
2. Brook I. Treatment of patients with acute recurrent tonsillitis due to group A ßhaemolytic streptococci: a prospective randomized study comparing penicillin
and amoxi/claviculanate potassium. J Antimicrob Chem 1989;24:227-33.
3. Kaplan EL, Johnson DR. Eradication of group A streptococci from the upper
respiratory tract by amoxicillin with clavunalate after oral penicillin V treatment
failure. J Pediatr 1988;113:400-3.
24
4. Orring A, Stjernquist-Desatnik A, Schalen C. Clindamycine in recurrent group A
streptococcal pharyngotonsillitis - an alternative to tonsillectomy. Acta
Otolaryngol (Stockh) 1997;117:618-25.
note 25
Tonsillectomy is performed preventively in 1 per 100 children each year (91.5% of
children up to 14 years). Parallel to the international trend, the number of tonsillectomies
in the Netherlands decreased by 2/3 since 1976, with the Netherlands remaining far ahead
internationally.1
Paradise et al.2 performed an 11-year prospective study in children, which used strict
inclusion criteria for children with only clinically objectifiable episodes of tonsillitis: 7
episodes of tonsillitis in the past year, or 5 per year in 2 years, or 3 per year in 3 years. An
episode of tonsillitis had at least the following symptoms: fever > 38.3 degrees, or
cervical lymphadenopathy, or exudate on the tonsils or the pharynx, or a positive throat
culture for ß-haemolytic streptococci. Among 2,043 patients, only 187 were included. Of
those, 91 children were randomized for either an adenotonsillectomy or a 'wait-and-see'
approach with antibiotic treatment for throat infection. The other 96 were subdivided
according to their parents' preference. In the first two years after the operation, there was
a reduction in the number of throat infections in the ATE group compared to the nonoperated group of 1 versus 3 episodes (measured by means of questionnaires). After 2
years, the difference was no longer significant (1 vs. 1.7 episodes). In this study, the
parental anamnesis was very unreliable.3 The effectiveness of tonsillectomies appeared to
be greatest in the category of mild throat infections: the unblinded nature of the study
could result in bias particularly in this group. In the first year, there was a difference of 3
days in school absenteeism between the two groups, and in the second year a difference
of 1.5 days. This study confirmed the results of previous studies of lesser quality.4 5
In 1990 in the Netherlands the mortality from adenotonsillectomy was estimated to be 1
in 74,000. The percentage of secondary bleeding was between 0.1 and 8.1%.6 The
impression given by at least 75% of parents was that their child's condition improved
following adenotonsillectomy. This has not been specifically studied in the Netherlands,
but the general impression is that parents are very satisfied with its results. International
studies strongly support this conclusion.7 8 A tonsillectomy in adults requires an average
of 14 days of sick leave from work.9 10
1. Hoogendoorn D. Schattingen van de aantallen tonsillectomieën en adenotomieën
bij kinderen [Estimates of the number of tonsillectomies and adenotomies in
children]. Ned Tijdschr Geneesk 1988;132:913-5.
2. Paradise JL, Bluestone CD, Bachman RZ, et al. Efficacy of tonsillectomy for
recurrent throat infection in severely affected children. New Engl J Med
1984;310:674-83.
3. Paradise JL, Bluestone CD, Bachman RZ, et al. History of recurrent sore throat
as an indication for tonsillectomy. New Engl J Med1978;298:409-13.
25
4. Mawson S, Adlington P, Evans M. A Controlled study evaluation of adenotonsillectomy in children. J Laryngol Otol 1967; 81: 777- 790.
5. Roydhouse N. A Controlled study of adenotonsillectomy. Arch Otolaryng
1970;92:611-6.
6. Hammelburg E. Honderd jaar knippen en pellen. In: Honderd jaar kopzorg,
Gedenkboek bij het eeuwfeest van de Nederlandse Vereniging voor Keel-NeusOorheelkunde en Heelkunde van het Hoofd-Halsgebied [A century of
tonsillectomies. In: A century of headiness: Commemorating the Centennial of the
Dutch Association for Otothinolaryngology and Head and Neck Surgery]. Utrecht
1993:37-48.
7. Conlon BJ, Donnelly MJ, McShane DP. Improvements in health and behaviour
following childhood tonsillectomy: a parental perspective at 1 year. Int J Pediatr
Otorhinolaryngol 1997;41:155-61.
8. Blair RL, McKerrow, WS, Carter NW, Fenton A. The Scottish tonsillectomy audit.
J Laryngol Otol 1996; suppl 20:1-25.
9. Murthy P, Laing MR. Dissection tonsillectomy: pattern of post-operative pain,
medication and resumption of normal activity. J Laryngol Otol 1998;112:41-4.
10. Mehanna HM, Kelly B, Browning GG. Disability and benefit from tonsillectomy
in adults. Clin Otolaryngol 1998;23:284.
© Copyright NHG 2002
disclaimer
26