Comparison Between Ibuprofen and Indomethacin For Closure of
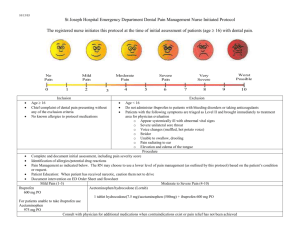
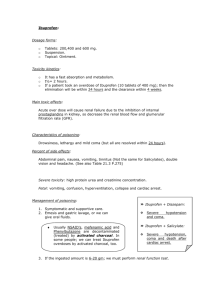
advertisement

EL-MINIA MED., BULL., VOL. 18, NO. 2, JUNE, 2007 Abdel Wahab & Mahfuz COMPARISON BETWEEN IBUPROFEN AND INDOMETHACIN FOR CLOSURE OF PATENT DUCTUS ARTERIOSUS IN PRETERM INFANTS By Walid Abdel Wahab1,3, Ahmed Mahfuz2,3 Departments of Pediatrics1, and Community Medicine2, College of Medicine, King Khalid University, Abha, Saudi Arabia, and Aseer Regional Committee of Neonatal Care3 ABSTRACT: Background: Patent ductus arteriosus (PDA) is commonly found in very low birth weight infants. Indomethacin and more recently, ibuprofen have been used to treat hemodynamically PDA in preterm infants. Both are cyclo-oxygenase inhibitors but seem to have a different influence on regional circulation. In a prospective randomized study, we compared ibuprofen and indomethacin with regard to efficacy and safety for the early non-invasive treatment of PDA in preterm infants. Methods: A total of 41 preterm infants with respiratory distress syndrome who had gestational age of < 30 weeks, postnatal age of 2-7 days, and echocardiographic evidence of hemodynamically significant PDA were enrolled in the study. Exclusion criteria were major congenital anomalies, IVH, recent bleeding (less than 48 hours previously), a platelet count of 100,000 / mm3 or less, urine output less than 1 ml / kg / hour during the previous 12 hours, serum creatinine level > 1.5 mg / dL, blood urea nitrogen (BUN) concentration > 50 mg / dL or concurrent administration of nephrotoxic medications. Patients were randomized into two groups: the first group of neonates (n = 20) received oral ibuprofen 10 mg/kg, followed by 5 mg / kg after 24 and 48 hours; the second group (n = 21) received intravenous indomethacin 0.2 mg/kg every 12 hours for three doses. Results: The efficacy of the pharmacological treatment was similar in the two groups. PDA closed in 15 (75%) patients from the ibuprofen group and in 16 (76%) patients in the indomethacin group. Serum creatinine and blood urea nitrogen levels were significantly lower (p < 0.001) in the ibuprofen group than in the indomethacin group. We found a significantly lower urine output in the indomethacin group than the ibuprofen group at 24 and 48 hours after treatment. Conclusion: Oral ibuprofen is as efficacious as indomethacin for the treatment of PDA in preterm infants and is significantly less likely to cause renal dysfunction. KEYWORDS: Patent ductus arteriosus Preterm infant. Ibuprofen Indomethacin development of symptomatic PDA which has been associated with an increased risk of intraventricular hemorrhage (IVH), Necrotizing enterocolitis (NEC), bronchopul-monary dysolasia (BPD), and death4. Consequently, prophylactic or curative INTRODUCTION: The incidence of patent ductus arteriosus (PDA) in infants weighing 501-1500 gram is approximately 31 % 1-3 . The occurrence of respiratory distress syndrome (RDS) strongly predisposes an infant to the 64 EL-MINIA MED., BULL., VOL. 18, NO. 2, JUNE, 2007 Abdel Wahab & Mahfuz / mm3 or less, urine output less than 1 ml / kg / hour during the previous 12 hours, serum creatinine level > 1.5 mg / dL, blood urea nitrogen (BUN) concentration > 50 mg / dL or concurrent administration of nephrotoxic medications. treatment has been advocated before the critical left-to-right shunting occurs5. Until recently, indomethacin has been the drug of choice. However, renal and cerebral hemodynamic side effects have been frequently reported68 . These adverse effects have prompted the search for new, safer pharmacological strategies for PDA closure9. After obtaining informed parental consent, patients enrolled in the study at each unit were randomly placed into two groups. The first group of neonates (group A, n = 20) (11 male and 9 female), received oral ibuprofen 10 mg / kg followed by 5 mg / kg after 24 and 48 hours. Ibuprofen was given undiluted through a feeding tube and flowed by flushing with distilled water. Ibuprofen has been shown to close the ductus arteriosus in animals without affecting cerebral blood flow or intestinal and renal hemodynamics10,11. More recently, ibu-profen has emerged as a potential alternative to indomethacin in the treatment of PDA12. Doses and interval for ibuprofen were in accordance with recommendations for its use in neonates based on preliminary pharmacodynamic data13. The efficacy if ibuprofen has not yet been adequately addressed in extremely premature infants9. The aim of this study was to compare the efficacy and safety of ibuprofen with that of indomethacin for closure of PDA in preterm infants. The second group of the patients (group B, n = 21) (12 male and 9 female) received intravenous indomethacin. The initial dose was 0.2 mg/kg. Two further doses were administered after 12 and 24 hours. SUBJECTS AND METHODS: This study was conducted at neonatal intensive care units of Abha General and Aseer Central Hospitals, Abha, Southwestern Saudia Arabia between between January 2003 and December 2004. Preterm infants admitted to both units were eligible for the trial if the following criteria were met: 1) Gestational age < 30 weeks, 2) Postnatal age 2-7 days, 3) RDS treated with mechanical ventilation, and 4) Echocardiographic evidence of hemodynamically significant PDA. Statistical analysis: Frequencies, percentage, arithmetic mean and standard deviation were used to present the data. Chisquare and Student “t” were used as tests of significance at 5 % level. Statistical analysis was performed by using the (SPSS) software. RESULTS: A total of 41 preterm infants with significant PDA were enrolled in the study. The first group of neonates , were treated with oral ibuprofen (n = 20), [11 (55 %) male and 9 ( 45 %) female], their mean gestational age (GA) was 27.3 + 1.2, range (25-30) weeks while their mean birth weight Exclusion criteria were major congenital anomalies, IVH, recent bleeding (less than 48 hours previously), a platelet count of 100,000 65 EL-MINIA MED., BULL., VOL. 18, NO. 2, JUNE, 2007 (BW) was 813 + 21.3, 1150) gram. range (650- Abdel Wahab & Mahfuz Safety of treatment Serum creatinine levels and blood urea nitrogen concentrations are shown in tables 2 and 3 respectively. The ibuprofen group had significantly lower (p < 0.001) serum creatinine levels and lower (p < 0.001) BUN at 24 and 48 hours after treatment than the indomethacin group. Urine output are shown in table 4. We found a significantly lower urine output in the indomethacin group than in the ibuprofen group at 24 and 48 hours after treatment. The second group of preterm infants were treated with intravenous indomethacin (n = 21), [12 (57 %) male and 9 (43 %) female], their mean gestational age was 27.2 + 1.0, range (26-29) weeks while their mean birth weight was 845 + 0.8, range (710-990) gram. Antenatal corticosteroids were given to the mothers of 8 (40 %) preterm infants in the first group and to the mothers of 9 (43 %) neonates in the second group. We found no significant differences between the two treated groups as regards GA, BW, and antenatal corticosteroids. Regarding the outcome of our patients, gastric bleeding occurred in one preterm infant in the indomethacin group however, no patients in the iburprofen group developed this adverse effect. Two patients in the indomethacin group had necrotizing enterocolitis but no infants in the ibuprofen group had this complication. One patient in each group developed IVH. Regarding the respiratory outcome, four patients in the ibuprofen group and five patients in the indomethacin group developed bronchopulmonary dysplasia. Statistically, there were no significant differences in gastric bleeding, NEC, IVH, and BPD between the ibuprofen and indomethacin groups. Efficacy of treatment Patent ductus arteriosus closed in 15 (75 %) patients in the ibuprofen group, and in 16 (76%) patients in the indomethacin group as shown in table 1. PDA reopening occurred in one patient in each group. One patient in the ibuprofen group and two patients in the indomethacin group required referral to higher center for surgical ligation. Regarding the efficacy of treatment, we found no significant differences between the ibuprofen and indomethacin groups, both are effective in PDA closure. Table 1: Efficacy of treatment PDA closure: n. (%) PDA reopening: n. (%) Transferred for surgical ligation: n. (%) *p values, not significant 66 Ibuprofen (n = 20) Indomethacin (n = 21) 15 (75) 1 (5) 1 (5) 16 (76)* 1 (4.7)* 2 (9.5)* EL-MINIA MED., BULL., VOL. 18, NO. 2, JUNE, 2007 Abdel Wahab & Mahfuz Table 2: Serum creatinine levels in mg /dL, (mean + SD) Pretreatment 24 hr after treatment 48 hr after treatment Ibuprofen (n = 20) 0.82 + 0.09* 0.86 + 0.08** 0.94 + 0.08** Indomethacin (n= 21) 0.76 + 0.11 1.42 + 0.31 1.58+ 0.28 *p = 0.7, ** p < 0.001 Table 3: Blood urea nitrogen concentrations in mg / dL, (mean + SD) Pretreatment 24 hr after treatment 48 hr after treatment Ibuprofen (n = 20) 13.8 + 3.1* 20.3 + 3.8** 23.1 + 3.7** Indomethacin (n = 21) 12.5 + 3.6 33.6 + 8.6 45.1+ 11.9 *p = 0.2, ** p < 0.001 Table 4: Urine output of the study infants in ml / kg / hr, (mean + SD) Pretreatment 24 hr after treatment 48 hr after treatment Ibuprofen (n = 20) 4.3 + 0.6* 4.0 + 0.6** 4.1 + 0.4*** Indomethacin (n = 21) 4.2 + 0.5 1.4 + 0.7 3.5+ 0.5 *p = 0.8, ** p < 0.001, ***p = 0.001 extremely preterm neonates require closure of hemodynamically 17,18 significant PDA . Vasodilator prostaglandins (PGs), PGE2 and PGI2 play a significant role in maintaining ductus patency during fetal and neonatal life19. DISCUSSION: Patent ductus arteriosus is a common complication of preterm birth and its incidence is inversely related to the gestational age14. A significant PDA in premature infants contributes to prolonged ventilator dependent, longer hospitalization, increased costs, and development of many complications including chronic lung disease, IVH, NEC and retinopathy of prematurity15,16. More than 50-70 % of Indomethacin a prostaglandin synthesis inhibitor, has been used widely in the prophylaxis and treatment of significant PDA20,21. 67 EL-MINIA MED., BULL., VOL. 18, NO. 2, JUNE, 2007 Abdel Wahab & Mahfuz Treatment with indomethacin, however, may be associated with adverse reactions such as reduced renal22, mesentric23, and cerebral perfusion24-25. Decreased perfusion to these vascular beds may lead to renal dysfunction, NEC, gastrointestinal hemorrhage and IVH or periventricular leukomalacia26. The difference between ibuprofen and indomethacin might be because indomethacin acts in part through mechanisms other than an inhibition of prostaglandin syntheses11. Other possibility is that both drugs inhibit the cyclo-oxyagenase enzyme system in the neonatal kidneys to different extent36. Ibuprofen, a cyclo-oxygenase inhibitor has been proved to be effective in closing PDA without reducing cerebral blood flow or affecting intestinal or renal hemodynamics27-29. Furthermore, ibuprofen enhances cerebral blood flow autoregulation and has been shown to protect neurological functions following oxidative stress in animal models30,31. We found 2 (9.5%) patients in the indomethacin group developed necrotizing enterocolitis however no patients in the ibuprofen group had this morbidity. These results are in consistent with that of the study done by Pezzati et al.,29. Our data support that ibuprofen does not significantly reduce mesenteric blood flow as compared with indomethacin. Ibuprofen has been shown to be effective in ductal closure by several investigators who administered it intravenously9, 12, 32. CONCLUSION: Based on our data, we conclude that oral ibuprofen is as efficacious as indomethacin for the treatment of PDA in preterm infants and is significantly less likely to cause renal dysfunction. Ibuprofen may become the drug of choice for ductal closure in premature neonates. Heyman et al., reported that oral ibuprofen might be an effective and safe alternative to intravenous ibuprofen for PDA closure in premature infants26. The pharmacokinetics of oral ibuprofen among preterm infants had been studied and reported. The finding indicated that ibuprofen is absorbed rapidly after oral administration and peak concentrations in plasma are observed after 1 to 2 hours33, 34. Acknowledgments We would like to thank cardiology department and all nurses of the neonatal intensive care units of Abha General and Aseer Central Hospitals for their support in carrying out this study. In our study, we found that oral ibuprofen therapy was as effective as indomethacin for the treatment of PDA in premature infants. Neonates treated with ibuprofen had significantly higher urine volume, lower serum creatinine and lower blood urea nitrogen values than neonates treated with indomethacin. The same findings have previously been reported by Lago et al.,35. REFERENCES: 1- The Vermont-Oxford trials network: Very low birth weight outcomes. Pediatrics 1993; 91: 540545 2- Hammerman C. Patent ductus arteriosus: Clinical relevance of prostaglandins and prostaglandin inhibitors in PDA pathophysiology and 68 EL-MINIA MED., BULL., VOL. 18, NO. 2, JUNE, 2007 treatment. Clinics in Perinatology 1995; 22: 457-479 3- Lagercrantz H, Katz-Salamon M, Forssberg H.: The Stockholm neonatal project: neonatal mortality and morbidity in the Children’s Center, Karolinska Hospital. Acta Paediatr Suppl 1997; 419: 11-15 4- Bancalari E, Claure N, Gonzalez A.: Patent ductus arteriosus and resoiratory outcome in premature infants. Biol Neonate 2005; 88: 192201 5- Stefano JL, Abbasi S, Pearlman SA, et al.,: Closure of ductus arteriosus with indomethacin in ventilated neonates with respiratory distress syndrome: Effects on pulmonary compliance and ventilation. Am Rev Respir Dis 1991; 143: 236-239 6- Van Bell F, Van der Bor M, Stijnen T, et al.,: Cerebral blood flow velocity changes in preterm infants after a single dose of indomethacin: Duration of its effects. Pediatrics 1989; 84: 802-807 7- Coombs RS, Morgan ME, Durbin GM, et al.,: Effects of Patent ductus arteriosus and parentral indomethacin. Arch Dis Child 1990; 65: 1067-1070 8- Van Bell F, Van Zoeren D, Shipper J, et al.,: Effect of indomethacin on superior mesenteric artery blood flow velocity in preterm infants. J Pediatr 1990; 116: 965-970 9- Desfrere L, Zohra S, Morville P, et al.,: Dose-finding study of ibuprofen in Patent ductus arteriosus using the continual reassessment method. J Clin Pharma & Therap 2005; 30: 121-132 10- Chemtob S, Beharry K, Barna T, et al.,: Differences in the effects in the newborn piglet of various nonsteroidal anti-inflammatory drugs on cerebral blood flow but not on cerebrovascular prostaglandins. Pediatr Res 1991; 30: 106-111 Abdel Wahab & Mahfuz 11- Malcom D, Segar J, Robillard E, et al.,: Indomethacin compromises hemodynamics during positivepressure ventilation, independency of prostanoids. J Appl Physiol 1993; 74: 1672-1678 12- Van Overmeire B. Smets K, Lecoutere D, et al.,: A comparison of ibuprofen and indomethacin for closure of patent ductus arteriosus. N Engl J Med 2000; 343: 674-681 13- Aranda J, Varvarigou A, Beharry K, et al.,: Pharmacokinetics and protein binding of intravenous ibuprofen in the premature newborn infant. Acta Paediatr 1997; 86: 289293 14- Hammerman C.: Patent ductus arteriosus. Clin Perinatol 1995; 22: 457-477 15- Drummond W.: Ductus arteriosus. In: Spitzer AR, ed. Intensive Care of the Fetus and Neonate. Mosbey-year Book, St Louis, 1996; 760-71 16- Knight D.: The treatment of patent ductus arteriosus in preterm infants. A review and overview of randomized trials. Semin Neonatol 2006: 63-73 17- Clyman R.: Ibuprofen and patent ductus arteriosus. N Engl J Med 2000; 343: 728-730 18- Fanaroff A, Hack M, Walsh M.: The NICHD neonatal research network: Changes in practice and outcomes during the first 15 years. Semin Perinatol 2003; 27: 281-287 19- Clyman R, Narayanan M. Patent ductus arteriosus: A physiologic basis for current treatment practices. In: Hansen T, McIntosh N, eds. Current Topics in Neonatology, number 4. WB Saunders, Philadelphia, 2000: 72-91 20- Krueger E, Mellander M, Bratton D, et al.,: Prevention of symptomatic ductus arteriosus with single dose of indomethacin. J Pediatr 1987; 111: 749-754 69 EL-MINIA MED., BULL., VOL. 18, NO. 2, JUNE, 2007 21- Hammerman C, Glaser J, Schimmel M, et al.,: Continuous versus multiple rapid infusion of indomethacin: Effects on cerebral blood flow velocity. Pediatrics 1995; 95: 244-248 22- Coombs R, Morgan M, Durbin G, et al.,: Gut blood flow velocities in newborn: Effects of patent ductus arteriosus and parentral indomethacin. Arch Dis Child 1990; 65: 1067-1071 23- Van Bell F, Guit G, Schipper J, et al.,: Indomethacin-induced changes in renal blood velocity waveform in premature infants investigated with color Doppler imaging. J Pediatr 1991; 118: 621-626 24- Pryds O, Greisen G, Johansen K.: Indomethacin and cerebral blood flow in preterm infants treated for patent ductus arteriosus. Eur J Pediatr 1988; 147: 315-316 25- Mardoum R, Bejar R, Merritt A, et al.,: Controlled study of the effects of indomethacin on cerebral blood flow velocities in newborn infants. J Pediatr 1991; 118: 112-115 26- Heyman E, Morag I, Batash D, et al.,: Closure of patent ductus arteriosus with oral ibuprofen suspension in premature newborns: A pilot study. Pediatrics 2003; 112: 354358 27- Patel J, Marks K, Roberts I, et al.,: Ibuprofen treatment of patent ductus arteriosus. Lancet 1995; 346: 255 28- Mosca F, Bray M, Lattanzio M, et al.,: Comparative evaluation of the effects of indomethacin and ibuprofen on cerebral perfusion and oxygenation in preterm infants with patent ductus arteriosus. J Pediatr 1997; 131: 549554 Abdel Wahab & Mahfuz 29- Pezzati M, Vangi V, Biagiotti R, et al.,: Effects of indomethacin and ibuprofen on mesentric and renal blood flow in preterm infants with patent ductus arteriosus. J Pediatr 1999; 135: 733- 738 30- Chemtob S, Beharry K, Rex J, et al.,: Prostanoids determine the range of cerebral blood flow autoregulation of newborn piglets. Stroke 1990; 21: 777-784 31- Chemtob S, Roy M, Abran D, et al.,: Prevention of post-asphyxial increase in lipid peroxides and retinal function deterioration in the newborn pig by inhibition of cyclo-oxygenase activity and free radical generation. Pediatr Res 1993; 33: 336-340 32- Fanos V, Benini D, Verlato G, et al.,: Efficacy and renal tolerability of ibuprofen vs. indomethacin in preterm infants with patent ductus arteriosus. Fundam Clin Pharmacol 2004; 19: 187-193 33- Kauffman R, Nelson M.: Effects of age on ibuprofen pharmacokinetics and antipyretic response. J Pediatr 1992; 121: 969-973 34- Kelley M, Walson P, Edge J, et al.,: Pharmacokinetics and pharma codynamics of ibuprofen isomers and acetaminophen in febrile children. Clin Pharmacol Ther 1992; 52: 181-189 35- Lago P, Bettiol T, Salvadori S.: Safety and efficacy of ibuprofen versus indomethacin in preterm infants treated for patent ductus arteriosus: a randomized controlled trial. Eur J Pediatr 2002; 161: 202-207 36- Van Overmeire B, Follens I, Hartmann S, et al.,: Treatment of patent ductus arteriosus with ibuprofen. Arch Dis Child 1997; 76: 179-84 70 Abdel Wahab & Mahfuz EL-MINIA MED., BULL., VOL. 18, NO. 2, JUNE, 2007 ”مقارنة بين عقار األيبوبروفين واألندوميثاسين لعالج األنبوبة الشريانية المفتوحة بين األورطى والشريان الرئوي فى األطفال الخدج“ وليد عبد الوهاب عيد , 1أحمد محفوظ طب األطفال ,1الصحة العامة -2كلية الطب-جامعة الملك خالد -أبها-المملكة العربية السعودية 2 خلفية وهدف البحث: يصاب حوالي % 31أو أكثر من األطفال الخدج (غير مكتملي العمر الحملي) باإلصابة بانفتاح األنبوبة الشريانية بين األورطي والشريان الرئوي ويتسبب ذلك فى العديد من المضاعفات الخطيرة والتى قد تؤدي إلى الوفاة .يستخدم األندوميثاسين فى عالج هذا المرض منذ سنوات طويلة وعلى الرغم من فاعلية هذا الدواء لكنه له العديد من اآلثار الجانبية خاصة على الكلى.هدفت هذه الدراسة إلى إجراء مقارنة بين األيبوبروفين واألندوميثاسين من ناحية الفاعلية واألمان لعالج هذا المرض فى األطفال الخدج. طريقة البحث: شملت هذه الدراسة 41طفال من األطفال الخدج المصابين بانفتاح األنبوبة الشريانية بعد تشخيصها بواسطة األشعة التلفزيونية على القلب والبالغ أعمارهم أقل من 30أسبوع رحمي. انقسم هؤالء األطفال إلى مجموعتين :المجموعة األولى بلغ عددها 20طفال وأخذوا عالج األيبوبروفين عن طريق أنبوب التغذية ,والمجموعة األخرى اشتملت على 21طفال وأخذوا عالج األندوميثاسين عن طريق الوريد .وتراوح عمر هؤالء األطفال بين 7-2أيام بعد والدتهم. استبعد من الدراسة األطفال المصابين بارتفاع فى مستوى البولينا والكرياتينين فى الدم وكذلك األطفال المصابين بنزيف أو انخفاض فى عدد الصفائح الدموية. نتائج البحث: أثبتت الدراسة أن فاعلية األيبوبروفين واألندوميثاسين فى عالج هذا المرض متساوية تقريبا حيث بلغت حوالي .%75كما أثبتت أيضا ارتفاع مستوى البولينا والكرياتينين فى دم األطفال الذين أخذوا عالج األندوميثاسين مقارنة بالمجموعة األخرى التى أخذت األيبوبروفين وذلك بعد 24و 48ساعة من أخذ الدواء .كما لوحظ أيضا أن كمية البول كانت أقل فى األطفال الذين أخذوا عقار األندوميثاسين .وكانت كل هذه الفروق ذات داللة إحصائية. اإلستنتاجات: عقار األيبوبروفين له نفس الفاعلية في عالج األنبوبة الشريانية المفتوحة فى األطفال الخدج مثل األندوميثاسين غير أنه يتفوق عليه بقلة اآلثار الجانبية خاصة على الكلى. 71