(Hand- Over/ Transfer of Patient Care)(Faculty Involvement Protocol)
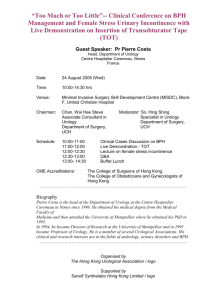
advertisement
College of Medicine DEPARTMENT OF UROLOGY RESIDENT MANUAL 2012 - 2013 CONTENTS Faculty .................................................................pg 4 & 5 Department of Urology Residents.............................................pg 6 &7 Resident Rotations ...................................................................pg 7 &8 Goals and Objectives ...............................................................pg 913 Educational Conferences ...........................................................pg 14 Clinical Training (Educational Objectives/ACGME Comp) pg 14 41 Resident Promotion Process (Policy) ....................................... pg 42 Call / Working Environment ................................................ .pg 43 Chief Residents ......................................................……… pg 43 Resident Responsibilities .......................................................pg 44 Communication ..............................................................pg 44 Duty Hour’s (Policy)……………………………………pg 44 Page 2 Department of Urology 2012-2013 Medical Records .............................................................pg 44 Referrals and Consultations .......................................... pg 45 Clinics .............................................................................pg 45 Orders .............................................................................pg 45 Rounds ........................................................................... pg 46 Progress Notes ............................................................... .pg 46 Preoperative Notes ......................................................... pg 46 Operating Room (OR) Schedule ......................................pg 47 Operating Room (OR) Etiquette ......................................pg 47 Operative Notes ...............................................................pg 47 Operative Report Dictation ..............................................pg 48 Operative Experience Record ..............................… pg 48& 49 Supervisory Lines of Responsibility for Patient Care (Policy) pg 50&51 (Hand- Over/ Transfer of Patient Care)(Faculty Involvement Protocol) Education ...................................................................................pg 52 Page 3 Department of Urology 2012-2013 General ...............................................................................pg 51 Conference Schedule ..........................................................pg 51 Urology Library ..................................................................pg 52 Residency Office and Lounge ............................................pg 53 Society Membership ...........................................................pg 53 Resident Research Presentations and Urology Review Courses Medical Student Teaching ..................................................pg 53 Research and Educational Projects ..........................................pg 53 Resident Selection .........................................................pg 54 & 55 American Bd of Urology In-Training Exam (ABUITE) .....pg 55 Resident Evaluation of the Program and Faculty(Policy) ....pg 55 & 56 Stipends ........................................................................pg 56 Licensure ...............................................................................pg 57 Moonlighting (Policy) ...................................................... pg 57 & 58 Page 4 Department of Urology 2012-2013 Identification ..........................................................................pg 58 Dress .......................................................................................pg 58 Vacation / Leaves of Absence ( Policy)…………………… pg 5760 Attestation ...............................................................................pg 61 Page 5 Department of Urology 2012-2013 DEPARTMENT OF UROLOGY FACULTY UTMC Clinical Faculty Kenneth A. Kropp, M.D., Professor Emeritus 3065 Arlington Avenue Toledo, Ohio 43614 419-383-3584 Steven H. Selman, M.D., Chairman, Program Director 3065 Arlington Avenue Toledo, Ohio 43614 419-383-3584 Michael Rees, M.D., PhD Renal Transplantation 3065 Arlington Avenue Toledo, Ohio 43614 419-383-3961 Khaled Shahrour, M.D. Assistant Professor 3065 Arlington Ave Toledo, Ohio 43614 419-383-3584 Jerzy Jankun, PhD Professor 3065 Arlington Ave Toledo, Ohio 43614 Mirza Baig, M.D. Assistant Professor 3065 Arlington Ave Toledo, Ohio 43614 Saleem Zafar, M.D. Assistant Professor 3065 Arlington Ave Toledo, Ohio 43614 Alice Bonnell, M.D. Assistant Professor 3065 Arlington Ave Toledo, Ohio 43614 Nurse Practitioner – Theresa Barabash, CNP Marc Crisenbery, CNP Urology Clinic – Manager, Anna Moss Department of Urology Administrator – Karen Edwards Residency & Curriculum Coordinator – Karen M. Boling Page 6 Department of Urology 2012-2013 COMMUNITY FACULTY Emmett Boyle, M.D. - Education Director, The Toledo Hospital Gregory Haselhun, M.D.- Educational Director, St. Vincent Mercy Medical Center Robert Navarre, M.D. Daniel Murtagh, M.D. Mark Wainstein, M.D. Michael Rashid, M.D. Eric Pizza, M.D. Timothy Schuster, M.D. Gregor Emmert, M.D. Salvador Peron, M.D. Peter Zografides, M.D. Parimal Vyas, M.D. Carin Hopps, M.D. Anyse Storey, M.D. Mani Menon, M.D. Steven Ariss, M.D. Stephen Sutton, M.D. Rou Wang, M.D. Page 7 Department of Urology 2012-2013 DEPARTMENT OF UROLOGY RESIDENTS 2011-2012 Name Medical School Natalie Singer University of Toledo Resident Year (PGY) 6 July 1, 2007-June 30, 2013 Thomas Zaciewski University of Toledo July 1, 2007-June 30, 2013 Evan Fynes University of Toledo 5 July 2008- June 30, 2014 Stanton Regan Indiana University July 2008 – June 30, 2014 Adam Becker University of Louisville 4 July 1, 2007-June 30, 2015 Stanton Regan University of Toledo July 1, 2007-June 30, 2015 Ryan Flynn Georgetown University July 1, 2010 – June 30, 2016 Timothy Suttle University of Oklahoma July 1, 2010 – June 30, 2016 Page 8 Department of Urology 2012-2013 3 Surgery Prelim Omar Khan-2 Hesham Mostafa-2 Bradley Buck-1 Daniel Murtagh, Jr.-1 RESIDENT ROTATIONS First Year Surgery Prelim Rotation Urology General Surgery Includes:plastics,SICU Trauma Duration (months) 6 months 6 months Site SVMMC UTMC,St.Lukes TTH Second Year Surgery Prelim Urology General Surgery Includes:Vasc, SICU Trauma 6 months 6 months TTH UTMC,St.Lukes TTH Third Year Urology – URO I 6 months 6 months SVMMC UTMC Fourth Year Urology – URO II 6 months 6 months SVMMC UTMC Fifth Year Urology – URO III 6 months 6 months UTMC TTH Sixth Year Urology – URO IV 6 months 6 months SVMMC UTMC Page 9 Department of Urology 2012-2013 Page 10 Department of Urology 2012-2013 Urology Residency Program Our Educational Philosophy: The objective of the Urology Program at the University of Toledo (UTMC) is to train urologists of the highest quality with the knowledge, clinical acumen and surgical skills to care for the entire spectrum of urological disorders. We believe in a rigorous academic training program with a strong didactic schedule, busy surgical caseload, and a valuable research experience. Particular emphasis is placed on teaching our residents the importance of establishing strong physician-patient relationships by the priority we place on continuity of care. We believe that faculty must dedicate themselves to teaching and that residents must demonstrate a strong commitment to learning. We expect that the residents trained in our program will become leaders in the urology community and that they will practice urology with personal integrity, high ethical standards, and respect for the rights of patients entrusted to their care. These educational goals are based on attaining the objectives set forth in the ACGME General Competencies of resident education. Overall Objectives of the Urology Residency Program The primary goal of this program is to provide training in the discipline of urology which will allow the successful graduate of the program to function as a qualified practitioner of urology and exhibit the level of performance necessary to attain board - certification. To achieve this goal the program is committed to providing a structured progressive educational environment in urology based on the six core competencies, technical skills and development of clinical knowledge. Following the conclusion of their training the trainees should be able to function as fully qualified physicians in the field of urology. The following objectives are also part of this goal: Graduate residents who are competent in the medical and surgical management of urological disorders in adults and children. Including: A) Outpatient diagnosis and therapy B) Inpatient diagnosis and management Enhance the residents experience and training in professionalism in working with: A) Peers B) Support staff C) Patients Provide exposure to and participation in research on urological disorders through: A) Work on projects in quality assurance and professional improvement B) Support for presentation of appropriate research at national meetings Educational Goals of the Urology Residency Program: Page 11 Department of Urology 2012-2013 The University of Toledo’s urology residency program seeks to develop proficiency and competency for its trainees in the surgical specialty of pediatric and adult urology. The program is broadly divided into two time frames. The first two years are considered the pre-urology years. During these years the trainee will be classified as a general surgery resident and will be educated in the principles of preoperative and postoperative care of the surgical patient. This includes principles of preoperative preparation for surgery, fluid and electrolyte problems of the surgical patient, surgical use of antibiotics and anticoagulation therapy, wound care and the overall management of critically ill patients in a surgical intensive care unit. Exposure to the surgical specialties of vascular surgery, plastic surgery and general surgery will provide the groundwork for the proper handling of tissues, vascular and bowel anastomoses, complex wound closures in the context of surgical anatomy. Additionally ample time in urology rotations in which the fundamental skills of patient assessment, radiologic evaluation, endoscopic evaluation, open and laparoscopic operative approach and postoperative management will be afforded. It is anticipated that this two year exposure will inculcate the trainee with the team work ethic that requires professionalism, self motivated education, communication skills and appreciation of health care systems issues. The subsequent 4 years will be spent in clinical urology. It is anticipated that with the gaining of clinical experience and the developing of surgical skills, increasing responsibilities will be assumed by the trainee. The clinical experience is centered at 3 venues, The University of Toledo Medical Center, St. Vincents Medical Center, and The Toledo Hospital. Both St. Vincent’s Mercy Medical Center and The Toledo Hospital are home to Pediatric Hospitals providing opportunity in the management of pediatric urologic problems. Trainees will be afforded exposure to a large number of urologic problems. Management of these problems will require education in problem assessment including physical exam, serologic determinations, radiologic evaluation including the modalities of standard x-rays, coaxial tomography, magnetic resonance, ultrasound and photon emission tomography. Clinical problem management will encompass endoscopic surgery, laparoscopic and robotic surgery, open surgery and the appropriate post operative care including the recognition and management of postoperative complications. Trainees will be exposed to the following broad classes of urologic disease: Urologic Oncology Pediatric Urology Infertility Sexual Dysfunction Calculus Disease Male and female Incontinence Male and female Voiding Dysfunction Neurogenic Bladder Renal Transplantation Procedure exposure will be provided in the following areas: Open Surgery—Flank, Transabdominal (intra and extraperitoneal), perineal Page 12 Department of Urology 2012-2013 Transurethral Laparoscopic and Robotic Percutaneous Endoureteral and endorenal Ultrasound and fluoroscopically guided Microsurgical General Urology Clinics: Goal 1 Perform a complete interview and accurate history from patients with urologic disorders encountered in the urology outpatient clinic setting Objectives – 1. Using appropriate and effective interview techniques, elicit and characterize an accurate history of the present illness from patients presenting with genitourinary complaints 2. Develop effective listening skills and be able to elicit and provide information using appropriate nonverbal and explanatory skills 3. Formulate and write coherent and legible notes in the medical record 4. Formulate treatment plans based on patient information and preferences for specific genitourinary diseases 5. Appropriately counsel and educate patients and their families about specific urologic problems 6. Be empathetic, understanding, compassionate and honest in dealings with patients and their families 7. Be sensitive and responsive to the urology patients’ culture, age, gender, and disabilities Goal 2 Perform a detailed and appropriately focused urologic physical examination Objectives – 1. Discuss and demonstrate ability to perform a detailed examination of the following genitourinary organ systems: a) Abdominal examination of the kidneys (inspection, palpation, percussion and auscultation) b) Inspection, percussion and palpation of the bladder c) Inspection and palpation of the penis d) Inspection, palpation and transillumination of the scrotum and its contents, including the testis, testicular tunics and adnexa, spermatic cord, and vas deferens 2. Discuss and demonstrate ability to perform a detailed male rectal examination to include: a) Assessment of the anal sphincter and lower rectum b) Prostate palpation to characterize its size, consistency, mobility, and the presence/absence of abnormalities, such as nodules or induration 3. Discuss and demonstrate an appropriate vaginal and rectovaginal examination in the female Page 13 Department of Urology 2012-2013 4. Be able to perform and interpret a focused neuro-urologic examination 5. Demonstrate ability to recognize visually and to palpate enlarged lymph nodes in regions related to genitourinary disease and to discuss their importance relative to differential diagnosis to various disorders 6. When performing physical examination, to be sensitive and responsive to the patients’ culture, age and gender Goal 3 Accurate performance and interpretation of commonly performed urologic laboratory studies Objectives – Demonstrate ability to perform and interpret the following laboratory studies a) routine urinalysis b) residual urine measurements c) expressed prostatic secretions d) semen analysis 2. Interpret and discuss the following laboratory studies a) serum PSA level and free/total PSA b) urinary electrolyte studies c) serum electrolyte studies and acid-base analysis d) serum creatinine and BUN e) creatinine clearance Goal 4 Performance and accurate interpretation of radiographic studies in the outpatient clinic setting Objectives – 1. Be able to competently perform and interpret the following radiographic studies a) plain films of the kidney, ureters and bladder (KUB) b) intravenous pyelogram (IVP) c) retrograde pyelogram d) retrograde urethrogram e) voiding cystourethrogram (VCUG) f) transrectal prostatic ultrasound 2. Be able to accurately interpret an abdominal/pelvic CT scan, MRI scan, renal ultrasound and radionuclide studies of the genitourinary tract Goal 5 Performance of diagnostic and therapeutic procedures encountered in the urology outpatient clinic Objectives – 1. Be able to perform the following outpatient procedures a) transrectal ultrasound-guided prostate biopsy b) flexible and rigid cystoscopy c) suprapubic tube placement d) vasectomy e) spermatic cord and penile block Page 14 Department of Urology 2012-2013 f) circumcision g) intravesical administration of chemotherapeutic or immunotherapeutic agents h) urethral dilation Goal 6 Competent care and evaluation of the pre-operative and post-operative urologic patient Objectives – 1. Perform and write clear, legible and an appropriately detailed history and physical examination on all pre-operative patients 2. Prepare and write clear and detailed admission orders 3. Assess and discuss the operative and anesthetic risks of surgical procedures 4. Obtain informed consent for all surgical procedures 5. Understand the indications for obtaining consultation with other health care specialists prior to the surgical procedure in select patients 6. Discuss the physiologic response of the normal patient to surgical procedures and factors that modify these responses 7. Discuss and evaluate wound healing as it relates to surgical incisions 8. Treat and evaluate pain in a safe and effective manner in the post-surgical patient 9. Discuss and evaluate the role of pharmacological agents, singly or in combination, and apply this knowledge to the care of the surgical patient 10. Understand the influence of other diseases and co-morbidities upon surgical care 11. Recognize and correct nutritional deficits in the surgical patient 12. Recognize and deal effectively with the psychological and emotional problems associated with anxiety imposed by urologic surgery ERECTILE DYSFUNCTION AND INFERTILITY : Goal 1 – Be proficient in the diagnosis, evaluation and treatment of patients with erectile dysfunction. Objectives 1. Describe the normal development and demonstrate the anatomy and function of the penis and male urethra 2. Describe the normal physiology of penile erection 3. List the etiologies of erectile dysfunction 4. Discuss common medical disorders associated with erectile dysfunction 5. Describe, in depth, the evaluation of patients with erectile dysfunction, including a sexual history, medical history, surgical history, physical examination, laboratory evaluation, and specialized testing 6. Describe, in detail, the various treatments of erectile dysfunction to include the following: a. medical treatment b. intracavernosal injection c. vacuum constriction devices d. psychological and sexual therapy e. surgical procedures implantation of penile prosthesis microvascular arterial bypass procedures Page 15 Department of Urology 2012-2013 Goal 2 – Demonstrate ability to diagnose, evaluate and treat patients with idiopathic priapism and prolonged penile erection secondary to intracavernosal injection of vasoactive drugs. Objectives 1. Describe the normal development and surgical anatomy of the penis 2. Discuss disturbances in the mechanism of normal erection resulting in priapism 3. List and describe the various etiologic factors in priapism 4. Demonstrate the ability to take a pertinent history and physical examination in patients with idiopathic or PIP-induced priapism 5. Demonstrate knowledge of the diagnostic studies that are helpful in establishing the etiology of priapism 6. Describe the vascular shunting procedures used in the treatment of priapism 7. Discuss the complications of each therapeutic method and appropriate treatment of these complications Goal 3 – Understand the basic science of male reproductive physiology and infertility Objectives 1. Demonstrate an understanding of the hypothalamic-pituitary-gonadal (HPG) axis and its endocrine control of testicular function 2. Identify the hormones involved in the HPG axis, their origins, function, reciprocal interrelationships and feedback control 3. List the endocrinopathies, both exogenous and endogenous, that may interfere with the normal testicular axial relationships and specify the nature of these alterations 4. Describe the anatomy, physiology, and pathophysiology of the male reproductive tract, spermatogenesis, sperm transport, and capacitation 5. Identify the sequence of sperm maturation, the cell types found within and between the seminiferous tubules and the time sequence of spermatogenesis 6. Describe the mechanism of ejaculation, including neurologic control and the anatomic structures involved 7. Identify disease states that interfere with ejaculation and the manner in which these states disrupt normal ejaculatory mechanisms 8. Describe the difference between emission and ejaculation Goal 4 Competent diagnosis, evaluation, and treatment of patients with male infertility Objectives 1. List the important components of a historical review in males presenting with infertility 2. Describe the components of the physical examination of infertile males 3. List the specific laboratory studies that should be obtained as part of the male infertility evaluation and the manner in which abnormal results may contribute to or reflect the extent of infertility 4. Select the surgical diagnostic techniques used in patients with male infertility including vasography, rectal sonography, and testicular biopsy 5. Identify exogenous drugs that may suppress fertility, ejaculation, and erectile dysfunction 6. Identify the appropriate surgical or medical therapies for patients with male infertility and defend the rationale and indications for clinical application of these modalities Page 16 Department of Urology 2012-2013 7. List and describe, in detail, the assisted reproductive techniques commonly used in patients with male factor infertility UROLITHIASIS: Goal 1 Know the etiology and pathophysiology of urinary tract stone disease Objectives 1. Understand the epidemiology of urolithiasis to include the following: Geographic distribution of urinary calculus incidence in this country and the world Incidence in relation to race, sex, age, and climatic factors The effects of dietary and fluid intake on occurrence 2. Describe the crystalline architecture of urinary calculi and theoretical factors affecting crystallization 3. Describe the part played by matrix in the architecture and possible prevention or initiation of stone formation 4. Describe the role of urinary tract obstruction in the etiology of urolithiasis 5. Present a working classification of the etiology of stone disease to include the following: Renal tubular syndromes Enzyme disorders Hypercalcemic conditions Hypercalciuric states Uric acid lithiasis Secondary urolithiasis Iatrogenic urolithiasis Goal 2 Be proficient in the evaluation and diagnosis of a patient with urolithiasis Objectives 1. Elicit a history compatible with stone disease from a patient including a list of pertinent problems referable to stone formation 2. Discuss the information to be gained from urinalysis including the appearance of typical crystals 3. Know the relationship of stone formation to urinary bacteria and pH 4. Select appropriate serum studies in the evaluation of stone disease including assessment of serum creatinine, calcium, phosphate, and uric acid. 5. Describe the role of stone analysis in the diagnosis and treatment of patients with stone disease 6. Have an in-depth knowledge of the radiographic evaluation of patients with stone disease, including the use of both plain film radiography and the CT urolithiasis study Goal 3 Select appropriate management strategies for patients with stone disease Objectives 1. Describe the role of dietary restriction and fluid intake modifications 2. Discuss, in detail, the medical therapy of patients with metabolic stone disease Page 17 Department of Urology 2012-2013 3. Discuss, in detail, and perform various procedures used in the treatment of stone disease to include the following: ESWL Percutaneous nephrolithotomy Pyelolithotomy Ureteroscopy Cystolithotomy Lithopaxy 4. Given a patient with recurrent stone disease, develop a plan for follow-up care including metabolic evaluation, appropriate treatment by diet, fluid intake or medications and subsequent evaluation by radiographic studies Goal 4 Demonstrate competence in the use of ESWL in the treatment of urolithiasis Objectives 1. List the types of ESWL machines available, including the sources of energy, methods of coupling energy to patient, and the methods for imaging and targeting stones 2. Describe the physics of shock wave stone fragmentation, including the absorption of energy at the acoustical interface, internal reflections of shock wave within the stone, and cavitation bubbles 3. List the indications and contraindications for the use of ESWL 4. Be familiar with pre-lithotripsy management including the indications for pre-treatment stents and selection of methods of anesthesia 5. Demonstrate ability to treat various stone types and describe initial energy levels used, total energy delivered, and the use of contrast to assist stone targeting 6. Discuss the post-treatment management of patients treated with ESWL 7. List the complications and risks of ESWL Goal 5 Develop competence in the use of endourologic techniques to treat upper urinary tract stones Objectives 1. Describe the surface relationships of the kidney and the structures traversed when a needle is passed into the renal pelvis through a posterior calyx 2. Know the intrarenal anatomy important to percutaneous renal access 3. Discuss the equipment commonly used in endourology, including guidewires, balloon dilators, stents, stone baskets and lithotriptors 4. Demonstrate knowledge of the various types of fluoroscopy equipment and the risks of fluoroscopy 5. Understand the technique of percutaneous nephrostomy placement, the use of fluoroscopy or ultrasound for guidance and the potential complications of this access procedure 6. Know the methods and instruments used for stone removal including forceps, baskets, and various grabbers, and know which stones can be removed with each 7. Discuss various methods of power lithotripsy, including ultrasound, electrohydraulic and laser lithotripsy 8. Know the complication of percutaneous stone removal and understand methods for their management Page 18 Department of Urology 2012-2013 9. Discuss the appropriate selection of patients for percutaneous lithotripsy as compared to ESWL 10. Discuss the use of percutaneous stone dissolution and describe various chemolytic agents 11. List the complications specific to various types of stone dissolution techniques Goal 6 Develop competence in the use of endourologic techniques to treat lower urinary tract stones Objectives 1. Demonstrate ability to perform both rigid and flexible ureteroscopy in the treatment of ureteral and renal stones 2. Understand the use of baskets, forceps, and other devices for ureteroscopic stone removal 3. Have a thorough knowledge of lithotripsy methods used via the ureteroscope to fragment ureteral stones 4. Describe the immediate and long-term complications of ureteroscopy, including extravasation, ureteral stricture, and avulsed ureter 5. Discuss the indications for ureteroscopic stone extraction as compared to the use of ESWL in the treatment of ureteral stones PEDIATRIC UROLOGY: Goal 1 Diagnose, evaluate and treat pediatric patients with adrenal disease Objectives 1. Understand the physiology of the normal adrenal 2. Recognize the clinical manifestations of the adrenal-genito (A-G) syndromes 3. Institute appropriate diagnostic steps in evaluation of the A-G syndrome 4. Institute treatment of the A-G syndrome 5. Counseling of families of patients with the A-G syndrome 6. Recognize, evaluate and treat patients with benign and malignant neoplasms of the adrenal, including adrenal hemorrhage, adrenal adenoma, pheochromocytome, and neuroblastoma. Goal 2 Diagnose, evaluate and treat patients with space-occupying lesions of the kidney Objectives 1. Diagnose and manage the spectrum of cystic disease of the kidney 2. Diagnose Wilm’s tumor of the kidney 3. Understand the role of adjuvant therapies for the management of patients with Wilm’s disease 4. Understand the surgical approach to patients with Wilm’s tumor Goal 3 Develop expertise in the management of UPJ anomalies Objectives 1. Understand the role of prenatal ultrasound in the diagnosis of UPJ obstruction 2. Recognize the clinical spectrum of presentation of UPJ obstruction 3. Understand the role of renal nuclear scan in the management of patients with UPJ obstruction Page 19 Department of Urology 2012-2013 4. Understand the various surgical approaches to the management of patients with UPJ obstruction 5. Understand follow up strategies in patients having undergone repair Goal 4 Be familiar with the diagnosis and management of ureteral anomalies Objectives 1. Understand the embryology and physiology of the normal ureter 2. Recognize the clinical spectrum of the megaureter 3. Understand management strategies for the patient with a megaureter 4. Recognize the clinical implication of the Meyer Weigert rule 5. Know the surgical options in the management of patients with ureteral duplication and associated renal anomalies Goal 5 Manage vesico-ureteral reflux Objectives 1. Know the classification system for vesico-ureteral reflux 2. Know and interpret the radiographic studies for the diagnosis of vesico-ureteral reflux 3. Understand the non-operative management of vesico-ureteral reflux 4. Know the surgical indications and techniques for the treatment of vesico-ureteral reflux Goal 6 Manage pediatric voiding dysfunction Objectives 1. Understand the role of urodynamics in the pediatric population 2. Know the options for management of the patient with enuresis 3. Understand the role of the urologist in the multidisciplinary management of patients with meningomyelocele 4. Understand the role of vesical augmentation in the patient with the neurogenic bladder 5. Understand the Mitrofanoff technique 6. Understand the indications for the Malone procedure 7. Discuss and understand the indications and surgical options for bladder neck reconstruction Goal 7 Management of pediatric undescended testicle Objectives 1. Know the embryology of the testes and testicular descent 2. Understand the indications for BHCG use in the management of the undescended testes 3. Know the indications for the use of laparoscopy in the management of patients with nonpalpable testes 4. Understand the surgical principals involved with the repair of the undescended testicle Goal 8 Management of the patient with ambiguous genitalia Objectives 1. Understand the full spectrum of the biochemical and genetic disorders which lead to intersex 2. Know the appropriate diagnostic steps in managing the patient with intersex Page 20 Department of Urology 2012-2013 3. Understand the surgical management of the patient with intersex Goal 9 Management of the patient with urethral abnormalities Objectives 1. Understand the embryology of the urethra 2. Classify the various degrees of hypospadias 3. Become adept in the surgical management of the hypospadiac urethra UROLOGIC ONCOLOGY: Goal 1 Know how to diagnose, evaluate and treat patients with kidney cancer Objectives 1. Understand the normal development, function and surgical anatomy of the kidney 2. Identify and discuss the gross and histopathologic features of the various types of renal tumors 3. Discuss the natural history and epidemiology of kidney cancer 4. Know the paraneoplastic syndromes that may be associated with renal cell carcinoma 5. Know and discuss the clinical and pathological staging systems used for renal cancer, and identify the prognosis as a function of the TNM stage of disease 6. Discuss the evaluation and plan a course of therapy for selected patients with various stages of renal cell carcinoma 7. Demonstrate the ability to select the best surgical approach (radical vs partial vs laparoscopic nephrectomy) in patients with kidney cancer 8. Discuss adjuvant therapy for patients with renal cancer including the roles of radiotherapy, chemotherapy and the use of biologic response modifier therapies 9. Identify and discuss the appropriate follow-up, including the role of radiographic imaging, of patients after radical or partial nephrectomy for renal cancer Goal 2 Competent diagnosis, evaluation and treatment of patients with cancer of the renal pelvis and ureter Objectives 1. Understand the normal development, function and anatomy of the ureter and renal pelvis 2. Discuss the theories regarding the etiology of cancer of the renal pelvis and ureter, and know the natural history and risk factors for tumor progression 3. Know the histopathologic features of transitional cell carcinoma of the upper urinary tract, including evaluation of urinary cytology 4. Demonstrate the ability to elicit a history compatible with cancer of the upper urinary tract and discuss findings on physical examination 5. List and be able to interpret the appropriate laboratory studies necessary to diagnose and stage cancer of the renal pelvis and ureter 6. Accurately select and interpret imaging studies of the upper urinary tract 7. Demonstrate competence in evaluation of the ureter and renal pelvis using endoscopic techniques Page 21 Department of Urology 2012-2013 8. Discuss the rationale for various surgical procedures used in the treatment of patients with ureteral or renal pelvic cancer, including the indications of nephron-sparing approaches in selected patients 9. Discuss the rationale, methodology, agents used and potential toxicities of intracavitary agents used in the treatment of superficial tumors 10. For patients with invasive or metastatic tumors of the upper urinary tract, discuss the role and potential toxicities of systemic chemotherapy Goal 3 Competent diagnosis, evaluation and treatment of patients with cancer of the bladder Objectives 1. Understand the embryology, normal development, function and anatomy of the bladder 2. Discuss the epidemiology of the various forms of bladder cancer, the concepts of initiation and promotion of carcinogenesis and risk factors for bladder cancer development 3. Know the natural history of superficial and muscle invasive bladder cancer 4. Know and discuss the clinical and pathological staging systems used for bladder cancer, and identify the prognosis as a function of the TNM stage of disease 5. Demonstrate the ability to recognize the signs and symptoms of patients with bladder cancer and be able to perform a bimanual examination of the bladder under anesthesia 6. Demonstrate the ability to interpret the results of laboratory and imaging studies in the diagnosis and staging of bladder cancer 7. Demonstrate competence in the performance of urethroscopy and cystoscopy in the evaluation and follow-up of patients with bladder cancer 8. Describe the endoscopic approaches to treatment of bladder cancer 9. Know and discuss the indications, efficacy, and complications associated with the use of intravesical therapies 10. Know and discuss the role of open surgical therapy for patients with bladder cancer, and discuss the role of lymph node dissection 11. Describe the various types of urinary diversion and considerations of their suitability in the context of extent of disease and patient preferences 12. Discuss the role of radiotherapy and chemotherapy in the treatment (adjuvant and therapeutic) of advanced bladder cancer Goal 4 Be proficient in the diagnosis, evaluation and treatment of patients with prostate cancer Objectives 1. Understand the embryology, normal development, function and anatomy of the prostate 2. Discuss the pathophysiology and theories regarding the etiology of prostate cancer 3. Know the gross and microscopic histopathology of prostate cancer and be able to differentiate these from other common histologic entities 4. Discuss the natural history and epidemiology of prostate cancer 5. Elicit a detailed and appropriate history from patients with prostate cancer 6. Demonstrate an ability to perform a digital rectal examination, including location and size of induration or nodules, pelvic sidewall and seminal vesicle extension of cancer Page 22 Department of Urology 2012-2013 7. Discuss the appropriate diagnostic and staging studies used to evaluate cancer of the prostate and interpret their results 8. Demonstrate the ability to perform an adequate transrectal ultrasound and biopsy of the prostate, and understand the rationale for various biopsy strategies 9. Discuss the risks, complications, and benefits of the various treatment options for prostate cancer, and demonstrate the ability to select appropriate patients for each treatment modality 10. Discuss with patients and families the prognosis and complications associated with prostate cancer treatment and understand the medical and psychological management of these complications 11. Know the appropriate follow-up regimens for patients after radical prostatectomy and radiation therapy for prostate cancer 12. Discuss the indications and controversies surrounding the use of adjuvant therapy after definitive therapy (radical prostatectomy or radiotherapy) Goal 5 Competent diagnosis, evaluation and treatment of patients with testicular cancer Objectives 1. Understand the embryology, normal development, function and surgical anatomy of the testis and paratesticular structures 2. Know and discuss the lymphatic drainage of the testicle and the pattern of lymphatic progression of disease to the retroperitoneum 3. Discuss various factors in the possible etiology of testis cancer 4. Know and differentiate the gross and histopathologic features of seminomatous, nonseminomatous and non-germ cell tumors 5. Demonstrate the ability to elicit a history compatible with testicular cancer 6. Perform a complete and accurate physical examination of patients with testicular cancer, including evaluation for lymphadenopathy or gynecomastia 7. List the appropriate diagnostic and staging studies used to evaluate cancer of the testicle or be able to interpret the results of these studies 8. Discuss the use of serum tumor markers in patients with testis cancer 9. Interpret testicular ultrasound and abdominal/pelvic CT findings in patients with testis cancer 10. Discuss the relative roles of retroperitoneal lymph node dissection and surveillance in patients with Stage I nonseminomatous testis cancer 11. Understand and discuss the selection of radiotherapy for the treatment of patients with testis cancer 12. Discuss various chemotherapeutic agents used in the treatment of advanced testis cancer and their relative value, depending on tumor type and stage Goal 6 Competent diagnosis, evaluation and treatment of patients with penile cancer Objectives 1. Understand the embryology, normal development, function and surgical anatomy of the penis and urethra Page 23 Department of Urology 2012-2013 2. 3. 4. 5. Discuss the incidence, epidemiology and potential etiologic factors of penile cancer Identify and discuss treatment and follow-up of premalignant penile lesions Know and use the TNM staging system for squamous cell carcinoma of the penis Demonstrate an appropriate examination of the penis and inguinal lymph nodes in patients diagnosed with penile cancer 6. Describe the surgical treatment options and their applicability to various stages of penile cancer 7. Discuss the strategies and indications for inguinal lymph node dissection 8. Discuss the roles of radiotherapy and chemotherapy in the treatment of local and advanced penile cancer Goal 7 Understand the role of chemotherapeutic agents in the treatment of genitourinary malignancies Objectives 1. Classify the commonly used chemotherapy agents used in urologic cancers 2. Discuss the pharmacology of the various types of chemotherapeutic drugs used in the treatment of urologic cancers 3. Describe the current chemotherapeutic regimens for genitourinary cancers 4. Know the specific complications of chemotherapy, both immediate and long-term, and treatment of these conditions 5. Discuss the treatment results and expected response rates of chemotherapy regimens used for the treatment of various genitourinary malignancies Goal 8 Understand the role of radiotherapy in the treatment of genitourinary malignancies Objectives 1. Discuss the physical properties of ionizing radiation, including the fundamental units used to describe the interaction of radiation matter and the differences in penetration and absorption between different types of radiation 2. Know the differences between external beam and interstitial radiotherapy 3. Discuss the isotopes used for interstitial radiotherapy, including differences in energy emitted, half-lives and the clinical utilization of each 4. Discuss the biologic factors impacting the effectiveness of radiotherapy 5. Demonstrate a basic understanding of radiotherapy principles as it relates to genitourinary malignancy 6. Discuss the commonly employed curative and palliative radiotherapeutic doses, schedules and fields for urologic tumors 7. Demonstrate knowledge of potential complications of radiotherapy, both in general and those associated with the treatment of specific urologic tumors Renal Transplantation: Goal 1 Evaluate patients who are potential recipients of a renal transplant Page 24 Department of Urology 2012-2013 Objectives: 1. Understand the pathologic states that lead to ESRD 2. Recognize co-morbid states which influence outcomes of renal transplantation. 3. Evaluate the suitability of potential renal transplant recipients 4. Understand the systems-based issues surrounding the acquisition of a renal transplant 5. Know the various immunosuppressive agents and their potential toxicities 6. Manage patients post transplantation with special emphasis of immunosuppressive regimens 7. Perform renal transplantation FEMALE UROLOGY: Goal 1 Understand the normal development, function and surgical anatomy of the female urethra, bladder and pelvis Objectives 1. Describe and explain the developmental processes by which the urethra progresses to tubular form and the hormonal influences in urethra development 2. Describe female urethral function by which urinary incontinence is maintained and the functional role of secondary structures, such as striated muscle 3. Know the blood, lymphatic, and nerve supply of the female bladder and urethra 4. Understand the normal anatomy and support of the female pelvis, including all involved organs and the supporting ligaments, muscle and fascia Goal 2 Competent evaluation, diagnosis and treatment of females presenting with urinary incontinence Objectives 1. Perform and demonstrate a complete medical history applicable of female patients presenting with urinary incontinence 2. Demonstrate an appropriate and complete physical examination of women with incontinence 3. Describe the laboratory studies that may assist with the diagnosis of women with incontinence 4. Demonstrate the ability to chose and carry out the appropriate therapy for the following conditions associated with female incontinence: Stress incontinence due to anatomical changes Stress incontinence due to sphincteric damage Urge incontinence and bladder instability Neurogenic bladder dysfunction Urinary retention and obstruction Urethral diverticula 5. Understand the role of pelvic floor neuromodulation in the treatment of patients with refractory voiding dysfunction due to pelvic floor dysfunction Page 25 Department of Urology 2012-2013 Goal 3 Know how to perform urodynamic studies in patients with voiding dysfunction Objectives 1. Discuss the value and indications for urodynamic evaluation of the lower urinary tract 2. Have an in-depth knowledge of the relationship of specific part of the urodynamic study to the filling/storage and emptying phases of micturition 3. Demonstrate the ability to independently set up and perform filling and voiding cytometry and be able to identify and interpret all of the following: Urinary flow rate Residual urine volume Flow patterns Bladder compliance Involuntary bladder contractions Abnormal bladder sensation Leak point pressures Bethanechol supersensitivity test Pressure/flow studies 4. Demonstrate the ability to independently set up and perform videourodynamics 5. Demonstrate the ability to independently set up and perform electromyography utilizing both needle and patch electrodes Goal 4 Know how to evaluate, diagnose and treat patients with pelvic pain syndromes, including interstitial cystitis Objectives: 1. Demonstrate an understanding of the epidemiologic aspects of interstitial cystitis 2. Be familiar with the common theories regarding the pathogenesis of interstitial cystitis 3. List the typical symptoms of interstitial cystitis in men and women 4. Discuss the differential diagnosis of the symptoms of interstitial cystitis 5. Be familiar with the cystoscopic findings in patients with interstitial cystitis and the indications and limitations of bladder biopsy 6. Explain the therapeutic rationale for the various treatments used in interstitial cystitis and be familiar with their benefits, efficacy and side-effects 7. List the systemic and intravesical pharmacotherapies used to treat interstitial cystitis 8. Know the role of bladder hydrodistention in patients with interstitial cystitis 9. Know the role of pelvic floor neuromodulation in the treatment of patients with interstitial cystitis and other pelvic pain syndromes 10. Know the role of surgical therapy for patients with refractory interstitial cystitis 11. Demonstrate proper selection of interstitial cystitis patients for surgical therapies Goal 5 Be competent in the diagnosis and treatment of patients with vesicovaginal and ureterovaginal fistulae Page 26 Department of Urology 2012-2013 Objectives 1. List the signs and symptoms commonly associated with vesicovaginal (VVF) and ureterovaginal (UVF) fistulae 2. Describe the pathogenesis of VVF, including iatronic, post-irradiation and obstetric trauma induced fistulae 3. Describe the important components of the history and physical examination in patients with VVF and UVF 4. Distinguish between VVF and UVF using historical and diagnostic techniques 5. Discuss the surgical principles involved in repair of these fistulas including the biology of wound repair and the preparation of tissues for surgery 6. Describe the conservative management of VVF and UVF 7. Discuss in detail the surgical repair options for patients with VVF or UVF UROLOGIC SURGERY: Goal 1 Know the background, indications and potential complications of several commonly performed urologic operative procedures Objectives 1. Describe the rationale and indications for surgery, and list the complications associated with the following surgical procedures: Nephrectomy Partial nephrectomy Pyeloplasty Ureteroureterostomy Ureteroneocystostomy Augmentation cystoplasty Transureteroureterostomy Boari flap and psoas hitch Ileal conduit Ileal neobladder Goal 2 Develop and refine basic surgical techniques required for performance of some of the commonly performed surgical cases in urology Objectives: 1. Describe specific surgical techniques applicable to the following operative procedures: Nephrectomy Partial nephrectomy Ureteroureterostomy Ureteroneocystostomy Augmentation cystoplasty Transureteroureterostomy Boari flap and psoas hitch Ileal conduit Ileal neobladder Page 27 Department of Urology 2012-2013 The knowledge base for the practice of urology will be provided through a series of conferences including a weekly standard textbook review, morbidity and mortality conference, indications conference, journal club, pathology review, tumor board and visiting professor rounds. During the URO III year those trainees assigned to the transplant service are expected to attend the weekly multidisciplinary patient evaluation conference as well as the monthly transplant operations meeting. Scholarly/Research opportunities both in clinical and basic science areas are provided and encouraged throughout the training years. It is expected that during the URO III year trainees will complete a research project suitable for presentation at a regional or national meeting appropriate for the research context. Residents will be expected to understand the fundamental importance of the six basic competencies and how they shape modern medical practice. The six competencies are: Patient Care Medical Knowledge Practice Based Learning Interpersonal and Communication Skills Professionalism Systems-Based Practice Educational evaluation will use faculty and health professional feedback. Each trainee will meet with the program director twice per year for assessment of progress. Each trainee is expected to participate in the yearly in-service examination. Professional skills training will be provided. Trainees will be evaluated within the framework of the six competencies. Evaluation is a two way process and it is expected that residents at all levels will provide constructive feedback as to the content and quality of the learning experience. Promotion will be based upon a consensus of program directors from the three training sites. General Competency-Based Goals and Objectives URO I, URO II, URO III, URO IV Level Specific Goals & Objectives URO – I : During the URO I year rotations include the first steps in mastery of all aspects of the clinical activities for both adult and pediatric urology. During this time, the resident develops the core of clinical and basic sciences knowledge required to care for patients with urologic diseases. In conjunction with the faculty at The Toledo Hospital and St. Vincent Mercy Medical Center, the residents master the fundamentals of the interpretation of urologic imaging, such as intravenous pyelography, coaxial tomography, and renal ultrasonography. The resident will also develop familiarity with invasive examination of the genitourinary tract, cystoscopy, ureteroscopy, and transrectal ultrasonography. Resident core knowledge of the diagnosis and staging of urologic malignancies, diagnosis of calculus disease, forms of incontinence, as well as embryologic and pediatric urologic problems develop through supervised patient contact and structured didactic sessions. Residents can expect their accumulating knowledge to be "tested" by faculty questions that assess the depth of resident knowledge of the clinical problem at hand. Page 28 Department of Urology 2012-2013 URO I residents are directly supervised by the Chief Resident. Daily rounds (except when off call on weekends, vacations and holidays) are made in conjunction with the Chief Resident. Efficient, expeditious and compassionate care-giving is developed. Residents are expected to develop basic bedside skills, such as suprapubic tube placement, use of filiforms and followers, catheter guides and flexible cystoscopy. Emergency room coverage and consultations are performed when on call in conjunction with the Chief Resident. Outpatient evaluations the Urology outpatient clinic are of great importance in the URO I training as a way to develop timely and cost-effective skills in the diagnosis and management of patients. Costs of patient management (pharmaceutical and lab expenses, etc.) are reviewed with the Chief Resident and attending physician in a prospective manner. Proper documentation of care in a problem-oriented and legible manner is emphasized. Technical Skills: In general, URO I residents participate in all endoscopic and open procedures. Principals of surgical handling of tissues and basic endoscopic skills are further developed. Residents are expected to “first assist” on procedures commensurate with their level of surgical training and “second assist” on more technically advanced open cases. PATIENT CARE: Goal To provide quality care that is appropriate, effective and compassionate to patients with urological health problems Objectives – 1. Obtain a complete and accurate history and physical examination from patients with genitourinary complaints 2. Interpret and obtain appropriate laboratory studies for the evaluation of urologic disorders 3. Formulate treatment plans based on patient information and preferences for specific genitourinary diseases 4. Apply current scientific evidence using information technology to facilitate the diagnosis and treatment of urologic disease 5. Appropriately counsel and educate patients and their families about specific urologic problems 6. Know the health care services aimed at preventing urologic problems and maintaining health 7. Work with other medical and surgical disciplines and healthcare professionals to provide multidisciplinary care to the urology patient 8. Competently perform all diagnostic and invasive procedures required for the appropriate management of genitourinary disorders in the outpatient setting 9. Perform all urologic surgical procedures including open, endourologic and laparoscopic cases, in a competent manner MEDICAL KNOWLEDGE: Goal Page 29 Department of Urology 2012-2013 Acquire basic scientific and clinical knowledge of the full spectrum of genitourinary disorders and be able to apply this knowledge to the care of the urologic patient Objectives – 1. Know the embryology, anatomy and physiology of the genitourinary system 2. Apply knowledge of the pathophysiology of the urologic disorders to the care of individual patients 3. Obtain and process knowledge about urologic disorders from reading standard urologic sources, current literature, internet sources and didactic teaching sessions 4. Perform well on standardized examinations (both written and oral) assessing fund of basic science and clinical knowledge 5. Dedication to improvement in medical knowledge through a commitment to continued medical education 6. Score in the 20th percentile or above on the annual American Board of Urology In-service examination PRACTICE-BASED LEARNING AND IMPROVEMENT: Goal Improve urologic patient care practices by the critical evaluation of current practice patterns and by the appraisal and assimilation of scientific evidence Objectives – 1. Critically analyze on a regular basis current practice experience using a systemic and reliable methodology 2. Perform practice-based improvement by implementing a change in practice based on newly acquired clinical information 3. Locate, appraise, and assimilate scientific studies from the urologic literature applicable to patient management 4. Understand scientific study design and statistical analysis to allow evaluation and appraisal of clinical studies 5. Use information technology to access and manage on-line medical information 6. Be an effective teacher of medical students, junior urology residents, and other healthcare professionals INTERPERSONAL AND COMMUNICATION SKILLS: Goal Develop interpersonal and communication (verbal and writing) skills that will allow effective exchange of information with urologic patients, their families, and other healthcare professionals Objectives – 1. Develop rapport with urologic patients and their families 2. Develop effective listening skills and be able to elicit and provide information using appropriate non-verbal, explanatory and patient interview skills 3. Formulate and write coherent and legible notes in the medical record 4. Write clear, concise and comprehensible manuscripts for publication in the urologic literature Page 30 Department of Urology 2012-2013 5. Prepare and deliver oral or case presentations in a thoughtful, organized and coherent manner 6. Work effectively with others (urologic residents and faculty) as a member/leader of the urology healthcare team PROFESSIONALISM: Goal Be professional by adherence to high ethical standards, professional responsibilities, and sensitivity to the diverse patient population Objectives – 1. Have respect, compassion, and integrity in interactions with patients, their family members, and other healthcare professionals 2. Accept responsibility readily, be industrious and self-motivated, and bring assigned tasks to completion 3. Function as an effective leader of the urology healthcare team 4. Understand and commit to the ethical principles pertaining to provision or withholding of clinical care, confidentiality of patient information, informed consent, and urology business practices 5. Be sensitive and responsive to the urology patients’ culture, age, gender, and disabilities SYSTEMS-BASED PRACTICE: Goal Be aware of and responsive to the healthcare system and use available resources from this system to optimize the care of urologic patients Objectives – 1. Understand how urology patient care practices affect other healthcare professionals within the local, regional, and national healthcare system 2. Describe how these varied types of healthcare systems affect individual urology practice 3. Understand differences between various types of medical practices and delivery systems, especially with regards to healthcare costs and allocation of resources. 4. Readily identify and correct healthcare system deficiencies that may result in less than optimal care of the urology patient 5. Assist urology patients in dealing with healthcare system complexities 6. Practice cost-effective healthcare and resource allocation without compromising quality of patient care 7. Know how to partner with healthcare managers or other providers in efforts to improve coordination and effectiveness of the healthcare system It is the intent of this training program to develop physicians who are clinically competent in urology. Physicians completing this program will be eligible for certification by the American Board of Urology with an ultimate goal of a 100% pass rate on this examination. To achieve this goal, the program has the following additional comprehensive objectives: 1. To provide an educational environment in urology so that postgraduate trainees receive and utilize adequate knowledge and experience to function as surgeons in Page 31 Department of Urology 2012-2013 2. 3. 4. 5. the field of urology following conclusion of six years of progressive education and training. To provide the trainee the opportunity to learn and understand the fundamentals of basic science as applied to clinical urology. To instill in the trainee a strong sense of honesty, integrity, and compassion in patient care. To instill in the trainee the lifelong discipline to continually learn new developments and changes in patient care so as to serve the patients. To instill in the trainee a sense of responsibility to disseminate new knowledge and teach other health professionals and colleagues. This program is composed of educational conferences and clinical training activities which are essential to the goals and objectives of the program. These essential functions of the program provide the broad background required to establish the basic competency to practice medicine in any field. This residency program is established so that the residents receive a progressive education with increasing responsibilities in the broad field of urology over a period of six years. This program is designed in such a fashion that the trainee receives education for evaluation of the patient, appropriate work-up to establish a diagnosis, management of patients and any complications of the disease or treatment in the broad field of urology; specifically, diseases of the genitourinary system, the comprehensive management of urologic trauma and emergency operations, and urologic critical care. The trainee will also receive education and clinical training in the surgical subspecialties to establish and understand basic principles of pre-, intra-, and postoperative management of patients in pediatric urology and renal transplant surgery. The trainee will also receive education and training in formulating, participating, and analyzing academic research activities. EDUCATIONAL CONFERENCES Required educational conferences are as follows: Morbidity and Mortality Conference. All complications and causes of death in patients admitted to the urologic services are discussed to establish the cause of complications or death and methods to avoid this in the future. Also, the etiology of such complications, natural history, and management of the complications are discussed. One hour conference held monthly. Journal Club. In this conference, select published literature is discussed to understand current trends of management of different diseases as well as the relative merits of various reports in contemporary journals. One hour conference held monthly. Urologic Pathology Lecture Series. In this conference, residents receive education on urologic pathology. One hour conference held monthly. Textbook Conference. This is a systematic review of information from standard textbooks in urology to familiarize residents with prevailing principles and methods of diagnosis and management of urological patients. Residents present subject overviews which are carefully reviewed with faculty members. One hour conference held weekly. Page 32 Department of Urology 2012-2013 Grand Rounds. In-depth presentations of select cases with faculty members as to delineate optimal management approaches to classic disease states Held monthly.. Visiting Professor Conference. Other specialty educational conferences for residents are as follows: Genitourinary Tumor Conference. Held biweekly for one hour. A multidisciplinary conference emphasizing systems related issues as they apply to the care of the patient with genitourinary cancer. Held monthly for one hour at TTH. Held monthly for one hour at SVMMC. Renal Transplant Conference. Held weekly for one hour. A multidisciplinary conference emphasizing systems related issues as they apply to the care of the patient with End Stage Renal Disease. Preoperative Patient Safety & Quality Assurance Conference. Held weekly. Voiding Dysfunction Conference. Held monthly Pediatric Indications Conference. Held weekly Level Specific Goals & Objectives URO II: The education process initiated in the URO I year continues throughout the URO – II year. Residents continue to mature in their clinical diagnostic skills. During this year, URO II residents have the opportunity to be the most senior residents on the urology service at The Toledo Hospital and have six months of dedicated UTMC/ Mercy Children’s Pediatric service at St. Vincent Mercy Medical Center. Faculty strive to enhance clinical confidence. Resident’s must obtain prior approval from attending for absence in coverage. Residents are expected to integrate their base of fundamental knowledge with the wide range of clinical urologic problems encountered at these sites. The URO II resident is the co-senior resident on the service at TTH. During this year, the residents develop a mature attitude towards the responsibility of patient care which is reflected by marked attention to all details of patient management, from admission to discharge planning. Resident management of patients in the outpatient setting is now expeditious and focused. Consults and emergency room coverage (when on call) includes patient evaluation, the ordering of appropriate diagnostic tests, and the formulation of a treatment plan in conjunction with the attending physician. Technical Skills: During this year, URO II residents develop their skills, both endoscopic and open surgical. In many cases, URO II residents are the surgeon or they “first assist” the attending physician and are active participants in all aspects of the surgical case. PATIENT CARE: Goal Page 33 Department of Urology 2012-2013 To provide quality care that is appropriate, effective and compassionate to patients with urological health problems Objectives – 1. Obtain a complete and accurate history and physical examination from patients with genitourinary complaints 2. Interpret and obtain appropriate laboratory studies for the evaluation of urologic disorders 3. Formulate treatment plans based on patient information and preferences for specific genitourinary diseases 4. Apply current scientific evidence using information technology to facilitate the diagnosis and treatment of urologic disease 5. Appropriately counsel and educate patients and their families about specific urologic problems 6. Know the health care services aimed at preventing urologic problems and maintaining health 7. Work with other medical and surgical disciplines and healthcare professionals to provide multidisciplinary care to the urology patient 8. Competently perform all diagnostic and invasive procedures required for the appropriate management of genitourinary disorders in the outpatient setting 9. Perform all urologic surgical procedures including open, endourologic and laparoscopic cases, in a competent manner MEDICAL KNOWLEDGE: Goal Acquire basic scientific and clinical knowledge of the full spectrum of genitourinary disorders and be able to apply this knowledge to the care of the urologic patient Objectives – 1. Know the embryology, anatomy and physiology of the genitourinary system 2. Apply knowledge of the pathophysiology of the urologic disorders to the care of individual patients 3. Obtain and process knowledge about urologic disorders from reading standard urologic sources, current literature, internet sources and didactic teaching sessions 4. Perform well on standardized examinations (both written and oral) assessing fund of basic science and clinical knowledge 5. Dedication to improvement in medical knowledge through a commitment to continued medical education PRACTICE-BASED LEARNING AND IMPROVEMENT: Goal Improve urologic patient care practices by the critical evaluation of current practice patterns and by the appraisal and assimilation of scientific evidence Objectives – 1. Critically analyze on a regular basis current practice experience using a systemic and reliable methodology Page 34 Department of Urology 2012-2013 2. Perform practice-based improvement by implementing a change in practice based on newly acquired clinical information 3. Locate, appraise, and assimilate scientific studies from the urologic literature applicable to patient management 4. Understand scientific study design and statistical analysis to allow evaluation and appraisal of clinical studies 5. Use information technology to access and manage on-line medical information 6. Be an effective teacher of medical students, junior urology residents, and other healthcare professionals INTERPERSONAL AND COMMUNICATION SKILLS: Goal Develop interpersonal and communication (verbal and writing) skills that will allow effective exchange of information with urologic patients, their families, and other healthcare professionals Objectives – 1. Develop rapport with urologic patients and their families 2. Develop effective listening skills and be able to elicit and provide information using appropriate non-verbal, explanatory and patient interview skills 3. Formulate and write coherent and legible notes in the medical record 4. Write clear, concise and comprehensible manuscripts for publication in the urologic literature 5. Prepare and deliver oral or case presentations in a thoughtful, organized and coherent manner 6. Work effectively with others (urologic residents and faculty) as a member/leader of the urology healthcare team PROFESSIONALISM: Goal Be professional by adherence to high ethical standards, professional responsibilities, and sensitivity to the diverse patient population Objectives – 1. Have respect, compassion, and integrity in interactions with patients, their family members, and other healthcare professionals 2. Accept responsibility readily, be industrious and self-motivated, and bring assigned tasks to completion 3. Function as an effective leader of the urology healthcare team 4. Understand and commit to the ethical principles pertaining to provision or withholding of clinical care, confidentiality of patient information, informed consent, and urology business practices Be sensitive and responsive to the urology patients’ culture, age, gender, and disabilities. SYSTEMS-BASED PRACTICE: Goal Be aware of and responsive to the healthcare system and use available resources from this system to optimize the care of urologic patients Objectives – Page 35 Department of Urology 2012-2013 1. Understand how urology patient care practices affect other healthcare professionals within the local, regional, and national healthcare system 2. Describe how these varied types of healthcare systems affect individual urology practice 3. Understand differences between various types of medical practices and delivery systems, especially with regards to healthcare costs and allocation of resources. 4. Readily identify and correct healthcare system deficiencies that may result in less than optimal care of the urology patient 5. Assist urology patients in dealing with healthcare system complexities 6. Practice cost-effective healthcare and resource allocation without compromising quality of patient care 7. Know how to partner with healthcare managers or other providers in efforts to improve coordination and effectiveness of the healthcare system It is the intent of this training program to develop physicians who are clinically competent in urology. Physicians completing this program will be eligible for certification by the American Board of Urology with an ultimate goal of a 100% pass rate on this examination. To achieve this goal, the program has the following additional comprehensive objectives: 1. To provide an educational environment in urology so that postgraduate trainees receive and utilize adequate knowledge and experience to function as surgeons in the field of urology following conclusion of six years of progressive education and training. 2. To provide the trainee the opportunity to learn and understand the fundamentals of basic science as applied to clinical urology. 3. To instill in the trainee a strong sense of honesty, integrity, and compassion in patient care. 4. To instill in the trainee the lifelong discipline to continually learn new developments and changes in patient care so as to serve the patients. 5. To instill in the trainee a sense of responsibility to disseminate new knowledge and teach other health professionals and colleagues. This program is composed of educational conferences and clinical training activities which are essential to the goals and objectives of the program. These essential functions of the program provide the broad background required to establish the basic competency to practice medicine in any field. This residency program is established so that the residents receive a progressive education with increasing responsibilities in the broad field of urology over a period of six years. This program is designed in such a fashion that the trainee receives education for evaluation of the patient, appropriate work-up to establish a diagnosis, management of patients and any complications of the disease or treatment in the broad field of urology; specifically, diseases of the genitourinary system, the comprehensive management of urologic trauma and emergency operations, and urologic critical care. The trainee will also receive education and clinical training in the surgical subspecialties to establish and understand basic principles of pre-, intra-, and postoperative management of patients in pediatric urology and renal transplant surgery. The trainee will also receive education and training in formulating, participating, and analyzing academic research activities. Page 36 Department of Urology 2012-2013 EDUCATIONAL CONFERENCES Required educational conferences are as follows: Morbidity and Mortality Conference. All complications and causes of death in patients admitted to the urologic services are discussed to establish the cause of complications or death and methods to avoid this in the future. Also, the etiology of such complications, natural history, and management of the complications are discussed. One hour conference held monthly. Journal Club. In this conference, select published literature is discussed to understand current trends of management of different diseases as well as the relative merits of various reports in contemporary journals. One hour conference held monthly. Urologic Pathology Lecture Series. In this conference, residents receive education on urologic pathology. One hour conference held monthly. Textbook Conference. This is a systematic review of information from standard textbooks in urology to familiarize residents with prevailing principles and methods of diagnosis and management of urological patients. Residents present subject overviews which are carefully reviewed with faculty members. One hour conference held weekly. Grand Rounds. In-depth presentations of select cases with faculty members as to delineate optimal management approaches to classic disease states Held monthly.. Visiting Professor Conference. Other specialty educational conferences for residents are as follows: Genitourinary Tumor Conference. Held biweekly for one hour. A multidisciplinary conference emphasizing systems related issues as they apply to the care of the patient with genitourinary cancer. Held monthly for one hour at TTH. Held monthly for one hour at SVMMC. Renal Transplant Conference. Held weekly for one hour. A multidisciplinary conference emphasizing systems related issues as they apply to the care of the patient with End Stage Renal Disease. Preoperative Patient Safety & Quality Assurance Conference. Held weekly. Voiding Dysfunction Conference. Held monthly Pediatric Indications Conference. Held weekly Level Specific Goals & Objectives URO III : URO III is research, renal transplantation and infertility. The resident will have ample opportunity to participate in one of the many research projects within the department. At the end Page 37 Department of Urology 2012-2013 of the URO III year it is anticipated that the resident’s activities will culminate in the production of new knowledge worthy of publication within a peer reviewed journal. Clinical education will revolve around all aspects of renal transplantation. The foundations of clinical immunology and immunosuppression will be mastered in this year as well as the elements of organ preservation. Residents will continue to participate in all other scheduled teaching rounds, clinical duties and didactic sessions during this year. A fertility clinic rotation at Genito Urinary Surgeons (Promedica affiliate) is also part of the URO III year. The URO III residents work with the URO IV residents at UTMC to supervise the URO I residents. During this year, the URO III continues to develop advanced surgical skills (including open and laparoscopic surgeries). Residents also continue to develop advanced patient management skills with an emphasis on renal transplant and infertility. Technical Skills: Residents will develop the technical skills for the safe and efficient removal of kidneys during multi-organ retrieval. All aspects of renal transplantation will include the vascular and ureteral anastomoses will be mastered. In addition, the techniques of needle biopsy of transplanted kidneys, implantation and removal of CAPD catheters will be included in this year. Transplant nephrectomy as well as laparoscopic donor nephrectomies will be preformed. PATIENT CARE: Goal To provide quality care that is appropriate, effective and compassionate to patients with urological health problems Objectives – 1. Obtain a complete and accurate history and physical examination from patients with genitourinary complaints 2. Interpret and obtain appropriate laboratory studies for the evaluation of urologic disorders 3. Formulate treatment plans based on patient information and preferences for specific genitourinary diseases 4. Apply current scientific evidence using information technology to facilitate the diagnosis and treatment of urologic disease 5. Appropriately counsel and educate patients and their families about specific urologic problems 6. Know the health care services aimed at preventing urologic problems and maintaining health 7. Work with other medical and surgical disciplines and healthcare professionals to provide multidisciplinary care to the urology patient 8. Competently perform all diagnostic and invasive procedures required for the appropriate management of genitourinary disorders in the outpatient setting 9. Perform all urologic surgical procedures including open, endourologic and laparoscopic cases, in a competent manner MEDICAL KNOWLEDGE: Goal Acquire basic scientific and clinical knowledge of the full spectrum of genitourinary disorders and be able to apply this knowledge to the care of the urologic patient Objectives – Page 38 Department of Urology 2012-2013 1. Know the embryology, anatomy and physiology of the genitourinary system 2. Apply knowledge of the pathophysiology of the urologic disorders to the care of individual patients 3. Obtain and process knowledge about urologic disorders from reading standard urologic sources, current literature, internet sources and didactic teaching sessions 4. Perform well on standardized examinations (both written and oral) assessing fund of basic science and clinical knowledge 5. Dedication to improvement in medical knowledge through a commitment to continued medical education PRACTICE-BASED LEARNING AND IMPROVEMENT: Goal Improve urologic patient care practices by the critical evaluation of current practice patterns and by the appraisal and assimilation of scientific evidence Objectives – 1. Critically analyze on a regular basis current practice experience using a systemic and reliable methodology 2. Perform practice-based improvement by implementing a change in practice based on newly acquired clinical information 3. Locate, appraise, and assimilate scientific studies from the urologic literature applicable to patient management 4. Understand scientific study design and statistical analysis to allow evaluation and appraisal of clinical studies 5. Use information technology to access and manage on-line medical information 6. Be an effective teacher of medical students, junior urology residents, and other healthcare professionals INTERPERSONAL AND COMMUNICATION SKILLS: Goal Develop interpersonal and communication (verbal and writing) skills that will allow effective exchange of information with urologic patients, their families, and other healthcare professionals Objectives – 1. Develop rapport with urologic patients and their families 2. Develop effective listening skills and be able to elicit and provide information using appropriate non-verbal, explanatory and patient interview skills 3. Formulate and write coherent and legible notes in the medical record 4. Write clear, concise and comprehensible manuscripts for publication in the urologic literature 5. Prepare and deliver oral or case presentations in a thoughtful, organized and coherent manner 6. Work effectively with others (urologic residents and faculty) as a member/leader of the urology healthcare team PROFESSIONALISM: Page 39 Department of Urology 2012-2013 Goal Be professional by adherence to high ethical standards, professional responsibilities, and sensitivity to the diverse patient population Objectives – 1. Have respect, compassion, and integrity in interactions with patients, their family members, and other healthcare professionals 2. Accept responsibility readily, be industrious and self-motivated, and bring assigned tasks to completion 3. Function as an effective leader of the urology healthcare team 4. Understand and commit to the ethical principles pertaining to provision or withholding of clinical care, confidentiality of patient information, informed consent, and urology business practices 5. Be sensitive and responsive to the urology patients’ culture, age, gender, and disabilities SYSTEMS-BASED PRACTICE: Goal Be aware of and responsive to the healthcare system and use available resources from this system to optimize the care of urologic patients Objectives – 1. Understand how urology patient care practices affect other healthcare professionals within the local, regional, and national healthcare system 2. Describe how these varied types of healthcare systems affect individual urology practice 3. Understand differences between various types of medical practices and delivery systems, especially with regards to healthcare costs and allocation of resources. 4. Readily identify and correct healthcare system deficiencies that may result in less than optimal care of the urology patient 5. Assist urology patients in dealing with healthcare system complexities 6. Practice cost-effective healthcare and resource allocation without compromising quality of patient care 7. Know how to partner with healthcare managers or other providers in efforts to improve coordination and effectiveness of the healthcare system It is the intent of this training program to develop physicians who are clinically competent in urology. Physicians completing this program will be eligible for certification by the American Board of Urology with an ultimate goal of a 100% pass rate on this examination. To achieve this goal, the program has the following additional comprehensive objectives: 1. 2. 3. To provide an educational environment in urology so that postgraduate trainees receive and utilize adequate knowledge and experience to function as surgeons in the field of urology following conclusion of six years of progressive education and training. To provide the trainee the opportunity to learn and understand the fundamentals of basic science as applied to clinical urology. To instill in the trainee a strong sense of honesty, integrity, and compassion in patient care. Page 40 Department of Urology 2012-2013 4. 5. To instill in the trainee the lifelong discipline to continually learn new developments and changes in patient care so as to serve the patients. To instill in the trainee a sense of responsibility to disseminate new knowledge and teach other health professionals and colleagues. This program is composed of educational conferences and clinical training activities which are essential to the goals and objectives of the program. These essential functions of the program provide the broad background required to establish the basic competency to practice medicine in any field. This residency program is established so that the residents receive a progressive education with increasing responsibilities in the broad field of urology over a period of six years. This program is designed in such a fashion that the trainee receives education for evaluation of the patient, appropriate work-up to establish a diagnosis, management of patients and any complications of the disease or treatment in the broad field of urology; specifically, diseases of the genitourinary system, the comprehensive management of urologic trauma and emergency operations, and urologic critical care. The trainee will also receive education and clinical training in the surgical subspecialties to establish and understand basic principles of pre-, intra-, and postoperative management of patients in pediatric urology and renal transplant surgery. The trainee will also receive education and training in formulating, participating, and analyzing academic research activities. EDUCATIONAL CONFERENCES Required educational conferences are as follows: Morbidity and Mortality Conference. All complications and causes of death in patients admitted to the urologic services are discussed to establish the cause of complications or death and methods to avoid this in the future. Also, the etiology of such complications, natural history, and management of the complications are discussed. One hour conference held monthly. Journal Club. In this conference, select published literature is discussed to understand current trends of management of different diseases as well as the relative merits of various reports in contemporary journals. One hour conference held monthly. Urologic Pathology Lecture Series. In this conference, residents receive education on urologic pathology. One hour conference held monthly. Textbook Conference. This is a systematic review of information from standard textbooks in urology to familiarize residents with prevailing principles and methods of diagnosis and management of urological patients. Residents present subject overviews which are carefully reviewed with faculty members. One hour conference held weekly. Grand Rounds. In-depth presentations of select cases with faculty members as to delineate optimal management approaches to classic disease states Held monthly.. Visiting Professor Conference. Other specialty educational conferences for residents are as follows: Page 41 Department of Urology 2012-2013 Genitourinary Tumor Conference. Held biweekly for one hour. A multidisciplinary conference emphasizing systems related issues as they apply to the care of the patient with genitourinary cancer. Held monthly for one hour at TTH. Held monthly for one hour at SVMMC. Renal Transplant Conference. Held weekly for one hour. A multidisciplinary conference emphasizing systems related issues as they apply to the care of the patient with End Stage Renal Disease. Preoperative Patient Safety & Quality Assurance Conference. Held weekly. Voiding Dysfunction Conference. Held monthly Pediatric Indications Conference. Held weekly Level Specific Goals & Objectives URO IV : URO IV, the Chief Resident (CR) year, is the culmination of the urology residency program. The CR assumes a major role in educational leadership. A diagnosis and management plan is synthesized by the CR prior to consultation with the attending physician, with documentation of the consult completed in a timely manner. The CR reviews junior residents’ assessments of the consults where appropriate. Consults to the emergency room are channeled through the CR prior to enlisting attending physician involvement unless such a pathway leads to delay in patient care management. The CR participates in urology outpatient clinic settings when not involved in the operating room or other aspects of direct patient care. The URO IV resident directly supervises the junior residents at both UTMC and SVMMC as well as the Pre URO resident at SVMMC. They are responsible for leading daily patient rounds as well as distributing the daily work load including case coverage. This administrative role also includes creating the conference calendar and call schedules. Residents in this year guide junior residents in the formulation of a patient care plan in both an inpatient and outpatient setting. Technical Skills: The CR has a major responsibility in all urological surgeries. Upon completion of the URO IV year, the CR is able to demonstrate competence in all aspects of open surgical and endoscopic surgery. PATIENT CARE: Goal To provide quality care that is appropriate, effective and compassionate to patients with urological health problems Objectives – 1. Obtain a complete and accurate history and physical examination from patients with genitourinary complaints Page 42 Department of Urology 2012-2013 2. Interpret and obtain appropriate laboratory studies for the evaluation of urologic disorders 3. Formulate treatment plans based on patient information and preferences for specific genitourinary diseases 4. Apply current scientific evidence using information technology to facilitate the diagnosis and treatment of urologic disease 5. Appropriately counsel and educate patients and their families about specific urologic problems 6. Know the health care services aimed at preventing urologic problems and maintaining health 7. Work with other medical and surgical disciplines and healthcare professionals to provide multidisciplinary care to the urology patient 8. Competently perform all diagnostic and invasive procedures required for the appropriate management of genitourinary disorders in the outpatient setting 9. Perform all urologic surgical procedures including open, endourologic and laparoscopic cases, in a competent manner MEDICAL KNOWLEDGE: Goal Acquire basic scientific and clinical knowledge of the full spectrum of genitourinary disorders and be able to apply this knowledge to the care of the urologic patient Objectives – 1. Know the embryology, anatomy and physiology of the genitourinary system 2. Apply knowledge of the pathophysiology of the urologic disorders to the care of individual patients 3. Obtain and process knowledge about urologic disorders from reading standard urologic sources, current literature, internet sources and didactic teaching sessions 4. Perform well on standardized examinations (both written and oral) assessing fund of basic science and clinical knowledge 5. Dedication to improvement in medical knowledge through a commitment to continued medical education PRACTICE-BASED LEARNING AND IMPROVEMENT: Goal Improve urologic patient care practices by the critical evaluation of current practice patterns and by the appraisal and assimilation of scientific evidence Objectives – 1. Critically analyze on a regular basis current practice experience using a systemic and reliable methodology 2. Perform practice-based improvement by implementing a change in practice based on newly acquired clinical information Page 43 Department of Urology 2012-2013 3. Locate, appraise, and assimilate scientific studies from the urologic literature applicable to patient management 4. Understand scientific study design and statistical analysis to allow evaluation and appraisal of clinical studies 5. Use information technology to access and manage on-line medical information 6. Be an effective teacher of medical students, junior urology residents, and other healthcare professionals INTERPERSONAL AND COMMUNICATION SKILLS: Goal Develop interpersonal and communication (verbal and writing) skills that will allow effective exchange of information with urologic patients, their families, and other healthcare professionals Objectives – 1. Develop rapport with urologic patients and their families 2. Develop effective listening skills and be able to elicit and provide information using appropriate non-verbal, explanatory and patient interview skills 3. Formulate and write coherent and legible notes in the medical record 4. Write clear, concise and comprehensible manuscripts for publication in the urologic literature 5. Prepare and deliver oral or case presentations in a thoughtful, organized and coherent manner Work effectively with others (urologic residents and faculty) as a member/leader of the urology healthcare team PROFESSIONALISM: Goal Be professional by adherence to high ethical standards, professional responsibilities, and sensitivity to the diverse patient population Objectives – 1. Have respect, compassion, and integrity in interactions with patients, their family members, and other healthcare professionals 2. Accept responsibility readily, be industrious and self-motivated, and bring assigned tasks to completion 3. Function as an effective leader of the urology healthcare team 4. Understand and commit to the ethical principles pertaining to provision or withholding of clinical care, confidentiality of patient information, informed consent, and urology business practices 5. Be sensitive and responsive to the urology patients’ culture, age, gender, and disabilities SYSTEMS-BASED PRACTICE: Goal Be aware of and responsive to the healthcare system and use available resources from this system to optimize the care of urologic patients Page 44 Department of Urology 2012-2013 Objectives – 1. Understand how urology patient care practices affect other healthcare professionals within the local, regional, and national healthcare system 2. Describe how these varied types of healthcare systems affect individual urology practice 3. Understand differences between various types of medical practices and delivery systems, especially with regards to healthcare costs and allocation of resources. 4. Readily identify and correct healthcare system deficiencies that may result in less than optimal care of the urology patient 5. Assist urology patients in dealing with healthcare system complexities 6. Practice cost-effective healthcare and resource allocation without compromising quality of patient care 7. Know how to partner with healthcare managers or other providers in efforts to improve coordination and effectiveness of the healthcare system It is the intent of this training program to develop physicians who are clinically competent in urology. Physicians completing this program will be eligible for certification by the American Board of Urology with an ultimate goal of a 100% pass rate on this examination. To achieve this goal, the program has the following additional comprehensive objectives: 1. To provide an educational environment in urology so that postgraduate trainees receive and utilize adequate knowledge and experience to function as surgeons in the field of urology following conclusion of six years of progressive education and training. 2. To provide the trainee the opportunity to learn and understand the fundamentals of basic science as applied to clinical urology. 3. To instill in the trainee a strong sense of honesty, integrity, and compassion in patient care. 4. To instill in the trainee the lifelong discipline to continually learn new developments and changes in patient care so as to serve the patients. 5. To instill in the trainee a sense of responsibility to disseminate new knowledge and teach other health professionals and colleagues. This program is composed of educational conferences and clinical training activities which are essential to the goals and objectives of the program. These essential functions of the program provide the broad background required to establish the basic competency to practice medicine in any field. This residency program is established so that the residents receive a progressive education with increasing responsibilities in the broad field of urology over a period of six years. This program is designed in such a fashion that the trainee receives education for evaluation of the patient, appropriate work-up to establish a diagnosis, management of patients and any complications of the disease or treatment in the broad field of urology; specifically, diseases of the genitourinary system, the comprehensive management of urologic trauma and emergency operations, and urologic critical care. The trainee will also receive education and clinical training in the surgical subspecialties to establish and understand basic principles of pre-, intra-, and postoperative management of patients in pediatric urology and renal transplant surgery. Page 45 Department of Urology 2012-2013 The trainee will also receive education and training in formulating, participating, and analyzing academic research activities. EDUCATIONAL CONFERENCES Required educational conferences are as follows: Morbidity and Mortality Conference. All complications and causes of death in patients admitted to the urologic services are discussed to establish the cause of complications or death and methods to avoid this in the future. Also, the etiology of such complications, natural history, and management of the complications are discussed. One hour conference held monthly. Journal Club. In this conference, select published literature is discussed to understand current trends of management of different diseases as well as the relative merits of various reports in contemporary journals. One hour conference held monthly. Urologic Pathology Lecture Series. In this conference, residents receive education on urologic pathology. One hour conference held monthly. Textbook Conference. This is a systematic review of information from standard textbooks in urology to familiarize residents with prevailing principles and methods of diagnosis and management of urological patients. Residents present subject overviews which are carefully reviewed with faculty members. One hour conference held weekly. Grand Rounds. In-depth presentations of select cases with faculty members as to delineate optimal management approaches to classic disease states Held monthly.. Visiting Professor Conference. Other specialty educational conferences for residents are as follows: Genitourinary Tumor Conference. Held biweekly for one hour. A multidisciplinary conference emphasizing systems related issues as they apply to the care of the patient with genitourinary cancer. Held monthly for one hour at TTH. Held monthly for one hour at SVMMC. Renal Transplant Conference. Held weekly for one hour. A multidisciplinary conference emphasizing systems related issues as they apply to the care of the patient with End Stage Renal Disease. Preoperative Patient Safety & Quality Assurance Conference. Held weekly. Voiding Dysfunction Conference. Held monthly Pediatric Indications Conference. Held weekly Rotation Specific Goals & Objectives for General Urology URO – I (UTMC) Overview: The Uro I Residents have completed two years of general surgery training. At the time of entering the URO 1 level, the resident is expected to know the basic human anatomy, Page 46 Department of Urology 2012-2013 physiology, and pathology of multiple organs. The resident has developed some manual dexterity with surgical instruments and learned to assist with surgical procedures. Goal: To develop a foundation in general urology based on the six core competencies. Objectives for Uro - I 1. Demonstrate ability to interact with urological patients and their families, obtain histories and perform physical examinations. 2. Demonstrate ability to diagnose urological disease. 3. Demonstrate basic understanding of uropathology. 4. Interpret the KUB, IVP, CT, MRI scans of the abdomen, sonography of the GU system and renal scan. 5. Determine treatment plan after adequate history and physical examination and laboratory testing including radiographic studies. 6. Assist and perform urological procedures: (a) Familiarity with all urological equipment, prepare for use and check their condition, and be aware of any potential problems or pitfalls. (b) Able to insert Foley catheter including difficult catheterization, perform cystoscopy and insertion of ureteral stents. (c) Perform minor urological procedures and fulguration of bleeders by endoscopy. (d) Demonstrate ability to be first assistant in minor and major urological procedures. 7. Demonstrate ability to recognize complications following urologic procedures. 8. Demonstrate ability to care for post-op urological patients. 9. Demonstrate ability to interact with patients, patient's families, medical personnel and faculty members. 10. Demonstrate leadership and teaching for residents in the Pre URO years as well as residents from other specialties rotating through urology. They should also be able to teach and set role models for medical students on the urology service. 11. Demonstrate familiarity with basic anatomy and physiology of the genitourinary system. The resident should be able to discuss mechanisms of stone formation, assessments of hypertension, evaluation of genitourinary neoplasms and physiology of obstructive uropathy. 12. Be able to discuss research protocols and have an understanding of basic statistics and evaluation of manuscripts. The resident should be able to present case material in a precise and organized manner. 13. Review and follow the general guidelines, factual knowledge, and technical skills and clinical guidelines commonly expected of individuals trained to practice urology. 14. Review the competency plan of the division and be familiar with the evaluation tools. 15. Prepare and participate in oral exams in-service yearly and score above the 20th percentile. Accomplishment of the above objectives will be facilitated by the activities below. 1. The resident is responsible for the admission of patients to the hospital including a history and physical exam and review of all relevant preoperative workup, assisting in surgery, and follow-up and discharge planning. The resident is to be in close contact with the patient providing up-to-date progress reports and to anticipate any problems that might be Page 47 Department of Urology 2012-2013 encountered in the patient's recovery. Communication with the appropriate attending urologist is essential and mandatory. 2. The resident will be given dedicated time each week to participate in the evaluation and management of patients in the outpatient clinic setting. Assignments to the clinic are designed to identify new patients and to follow-up on post-operative patients who were under the resident's care during the hospitalization. 3. Each resident will be required to begin working on a research project and to lay groundwork for the protocol and conduct of the project. The resident is expected to continue work on the project during clinical residency in urology, to prepare the material for presentation at a regional or national conference and to prepare a manuscript for publication. 4. The resident is required to attend the weekly academic conferences, and to present cases and participate in the meetings. Participation in the M & M, uropathology, radiology, pre-op, Campbell's, Journal Club, Grand, Rounds, GU Tumor, Preoperative Patient Safety & Quality Assurance and Voiding Dysfuction conferences is mandatory. SPECIFIC OBJECTIVES – URO – I (UTMC) The resident will observe, participate and have mentored experience in emergency room urology, including the following: __________ Assist complex Foley catheterization __________ Post-operative evaluation __________ Management and evaluation of hematuria, and assist in simple endoscopic management __________ Evaluation of stone disease __________ Assist in evaluation of urologic trauma __________ Evaluation of urologic emergencies __________ Manage post operative complications presenting to the emergency room The resident will observe, participate and have mentored experience in clinic-based urology, including the following: __________ Evaluation of urologic cancers __________ Evaluation of stone disease, surgical and medical evaluation __________ Evaluation of incontinence __________ Evaluation of impotence __________ Evaluation of voiding dysfunction __________ Evaluation and management of GU infections The resident will observe and perform minor urology procedures, including the following: __________ Cystoscopy of adults and pediatric __________ Stent removal, stent placement, stent change __________ Retrograde pyelogram __________ Testes biopsy __________ Penile biopsy Page 48 Department of Urology 2012-2013 __________ __________ __________ __________ __________ __________ __________ __________ __________ __________ __________ __________ Prostate ultrasound Prostate biopsy Shock wave lithotripsy CMG-EMG Videourodynamics Vasectomy Varicocelectomy Scrotal surgery Circumcision Orchiopexy Orchiectomy TUR bladder biopsy The resident will observe and assist in major urology cases, including the following: __________ Radical prostatectomy __________ Radical cystectomy __________ Continent diversion __________ Procedures for urinary incontinence __________ Radical nephrectomy __________ Donor nephrectomy __________ Percutaneous renal surgery __________ Endourology, including ureteroscopy, laser lithotripsy, incisions of the urinary tract __________ Transurethral surgery, including TURBT and TURP __________ Laparoscopic urology __________ RPLND The resident will work towards development in the six core competencies: Patient Care __________ Communicate effectively and demonstrate caring and respectful behaviors when interacting with patients with urologic disease __________ Gather essential and accurate information about urologic patients __________ Make informed decisions about diagnostic and therapeutic interventions in urology based on patient information and preferences, up-to-date scientific evidence, and clinical judgment of urology faculty __________ Develop and carry out patient management plans for select urologic disorders __________ Counsel and educate patients and their families on urologic diseases __________ Use information technology (on-line journals, CD-rom educational programs, lectures) to support patient care decisions and patient education __________ Perform and assist competently medical and invasive procedures considered essential in outpatient urology __________ Provide health care services aimed at preventing health problems or maintaining health, particularly prostate cancer, bladder cancer, stone disease, impotence, voiding dysfunction Page 49 Department of Urology 2012-2013 __________ Work with health care professionals, including those from other disciplines __________ Provide patient-focused care in the SIU assigned clinics Medical Knowledge __________ Demonstrate an investigatory and analytic thinking approach to clinical situations __________ Know and apply the basic (molecular biology) and clinically supportive sciences (nephrology, human oncology, transplantation) in urology _________ Performance on the annual American Board of Urology In-Training. Failure to score above the 20th percentile will result in a warning and may be grounds for probation Practice-Based Learning and Improvement __________ Analyze practice experience and perform practice-based improvement activities via chart reviews and personal feedback by rotation faculty __________ Locate, appraise, and assimilate evidence from scientific studies related to patients’ health problems __________ Obtain and use information about SIU patients and the larger population from where their patients are drawn in clinical studies __________ Apply knowledge of study designs and statistical methods to the appraisal of clinical studies and other information on diagnostic and therapeutic effectiveness, particularly when presenting at state and national meetings __________ Use information technology to manage information, access on-line medical information __________ Facilitate the learning of medical students and other health care professionals including mid-level providers, RNs, MAs Interpersonal and Communication Skills __________ Create and sustain a therapeutic and ethically sound relationship with patients, particularly ward patients __________ Use effective listening skills and elicit and provide information using effective nonverbal, explanatory, questioning, and writing skills __________ Work effectively with others as a team member or leader of a health care team (urology service) __________ Monitor colleagues for excessive stress and fatigue as taught in lecture series Professionalism __________ Demonstrate respect, compassion, and integrity; a responsiveness to the needs of patients and society that supercedes self-interest; accountability to patients, society, and the profession; and a commitment to excellence and on-going professional development __________ Demonstrate a commitment to ethical principles pertaining to provision or withholding of clinical care, confidentiality of patient information, informed consent, and business practices at all times. __________ Demonstrate sensitivity and responsiveness to patients’ culture, age, gender, and disabilities Page 50 Department of Urology 2012-2013 Systems-Based Practice __________ Understand how their patient care and other professional practices affect other health care professionals, the health care organization, and society and how these elements of the system affect their own practice (chart reviews with rotation faculty) __________ Know how types of medical practice and delivery systems differ from one another, including methods of controlling health care costs and allocating resources (part of clinical lecture series) __________ Practice cost-effective health care and resource allocation that does not compromise quality of care (chart reviews with rotation faculty) __________ Advocate for quality patient care and assist patients in dealing with system complexities __________ Know how to partner with health care managers and health care providers to assess, coordinate, and improve health care and know how these activities can affect system performance (experience on wards and in clinic on system-based performance in urology Rotation Specific Goals & Objectives for General Urology URO – I (SVMMC) Overview: The Uro I Residents have completed two years of general surgery training. At the time of entering the URO 1 level, the resident is expected to know the basic human anatomy, physiology, and pathology of multiple organs. The resident has developed some manual dexterity with surgical instruments and learned to assist with surgical procedures. Goal: To develop a foundation in general urology based on the six core competencies. Objectives for Uro - I 1. Demonstrate ability to interact with urological patients and their families, obtain histories and perform physical examinations. 2. Demonstrate ability to diagnose urological disease. 3. Demonstrate basic understanding of uropathology. 4. Interpret the KUB, IVP, CT, MRI scans of the abdomen, sonography of the GU system and renal scan. 5. Determine treatment plan after adequate history and physical examination and laboratory testing including radiographic studies. 6. Assist and perform urological procedures: (a) Familiarity with all urological equipment, prepare for use and check their condition, and be aware of any potential problems or pitfalls. (b) Able to insert Foley catheter including difficult catheterization, perform cystoscopy and insertion of ureteral stents. (c) Perform minor urological procedures and fulguration of bleeders by endoscopy. (d) Demonstrate ability to be first assistant in minor and major urological procedures. 7. Demonstrate ability to recognize complications following urologic procedures. 8. Demonstrate ability to care for post-op urological patients. 9. Demonstrate ability to interact with patients, patient's families, medical personnel and faculty members. Page 51 Department of Urology 2012-2013 10. Demonstrate leadership and teaching for residents in the Pre URO years as well as residents from other specialties rotating through urology. They should also be able to teach and set role models for medical students on the urology service. 11. Demonstrate familiarity with basic anatomy and physiology of the genitourinary system. The resident should be able to discuss mechanisms of stone formation, assessments of hypertension, evaluation of genitourinary neoplasms and physiology of obstructive uropathy. 12. Be able to discuss research protocols and have an understanding of basic statistics and evaluation of manuscripts. The resident should be able to present case material in a precise and organized manner. 13. Review and follow the general guidelines, factual knowledge, and technical skills and clinical guidelines commonly expected of individuals trained to practice urology. 14. Review the competency plan of the division and be familiar with the evaluation tools. 15. Prepare and participate in oral exams in-service yearly, obtain a minimum (50% of peer group). Accomplishment of the above objectives will be facilitated by the activities below. 1. The resident is responsible for the admission of patients to the hospital including a history and physical exam and review of all relevant preoperative workup, assisting in surgery, and follow-up and discharge planning. The resident is to be in close contact with the patient providing up-to-date progress reports and to anticipate any problems that might be encountered in the patient's recovery. Communication with the appropriate attending urologist is essential and mandatory. 2. The resident will be given dedicated time each week to participate in the evaluation and management of patients in the outpatient clinic setting. Assignments to the clinic are designed to identify new patients and to follow-up on post-operative patients who were under the resident's care during the hospitalization. 3. Each resident will be required to begin working on a research project and to lay groundwork for the protocol and conduct of the project. The resident is expected to continue work on the project during clinical residency in urology, to prepare the material for presentation at a regional or national conference and to prepare a manuscript for publication. 4. The resident is required to attend the weekly academic conferences, and to present cases and participate in the meetings. Participation in the M & M, uropathology, radiology, pre-op, Campbell's, Journal Club, Grand, Rounds, GU Tumor, Pediatric Indications conferences is mandatory. SPECIFIC OBJECTIVES – URO – I (SVMMC) Page 52 Department of Urology 2012-2013 The resident will observe, participate and have mentored experience in emergency room urology, including the following: __________ Assist complex Foley catheterization __________ Post-operative evaluation __________ Management and evaluation of hematuria, and assist in simple endoscopic management __________ Evaluation of stone disease __________ Assist in evaluation of urologic trauma __________ Evaluation of urologic emergencies __________ Manage post operative complications presenting to the emergency room The resident will observe, participate and have mentored experience in clinic-based urology, including the following: __________ Evaluation of urologic cancers __________ Evaluation of stone disease, surgical and medical evaluation __________ Evaluation of incontinence __________ Evaluation of impotence __________ Evaluation of voiding dysfunction __________ Evaluation and management of GU infections The resident will observe and perform minor urology procedures, including the following: __________ Cystoscopy of adults and pediatric __________ Stent removal, stent placement, stent change __________ Retrograde pyelogram __________ Testes biopsy __________ Penile biopsy __________ Prostate ultrasound __________ Prostate biopsy __________ Shock wave lithotripsy __________ CMG-EMG __________ Videourodynamics __________ Vasectomy __________ Varicocelectomy __________ Scrotal surgery __________ Circumcision __________ Orchiopexy __________ Orchiectomy __________ TUR bladder biopsy The resident will observe and assist in major urology cases, including the following: __________ Radical prostatectomy __________ Radical cystectomy __________ Continent diversion __________ Procedures for urinary incontinence __________ Radical nephrectomy Page 53 Department of Urology 2012-2013 __________ Donor nephrectomy __________ Percutaneous renal surgery __________ Endourology, including ureteroscopy, laser lithotripsy, incisions of the urinary tract __________ Transurethral surgery, including TURBT and TURP __________ Laparoscopic urology __________ RPLND The resident will work towards development in the six core competencies: Patient Care __________ Communicate effectively and demonstrate caring and respectful behaviors when interacting with patients with urologic disease __________ Gather essential and accurate information about urologic patients __________ Make informed decisions about diagnostic and therapeutic interventions in urology based on patient information and preferences, up-to-date scientific evidence, and clinical judgment of urology faculty __________ Develop and carry out patient management plans for select urologic disorders __________ Counsel and educate patients and their families on urologic diseases __________ Use information technology (on-line journals, CD-rom educational programs, lectures) to support patient care decisions and patient education __________ Perform and assist competently medical and invasive procedures considered essential in outpatient urology __________ Provide health care services aimed at preventing health problems or maintaining health, particularly prostate cancer, bladder cancer, stone disease, impotence, voiding dysfunction __________ Work with health care professionals, including those from other disciplines __________ Provide patient-focused care in the SIU assigned clinics Medical Knowledge __________ Demonstrate an investigatory and analytic thinking approach to clinical situations __________ Know and apply the basic (molecular biology) and clinically supportive sciences (nephrology, human oncology, transplantation) in urology Practice-Based Learning and Improvement __________ Analyze practice experience and perform practice-based improvement activities via chart reviews and personal feedback by rotation faculty __________ Locate, appraise, and assimilate evidence from scientific studies related to patients’ health problems __________ Obtain and use information about SIU patients and the larger population from where their patients are drawn in clinical studies __________ Apply knowledge of study designs and statistical methods to the appraisal of clinical studies and other information on diagnostic and therapeutic effectiveness, particularly when presenting at state and national meetings __________ Use information technology to manage information, access on-line medical information Page 54 Department of Urology 2012-2013 __________ Facilitate the learning of medical students and other health care professionals including mid-level providers, RNs, MAs Interpersonal and Communication Skills __________ Create and sustain a therapeutic and ethically sound relationship with patients, particularly ward patients __________ Use effective listening skills and elicit and provide information using effective nonverbal, explanatory, questioning, and writing skills __________ Work effectively with others as a team member or leader of a health care team (urology service) __________ Monitor colleagues for excessive stress and fatigue as taught in lecture series Professionalism __________ Demonstrate respect, compassion, and integrity; a responsiveness to the needs of patients and society that supercedes self-interest; accountability to patients, society, and the profession; and a commitment to excellence and on-going professional development __________ Demonstrate a commitment to ethical principles pertaining to provision or withholding of clinical care, confidentiality of patient information, informed consent, and business practices at all times. __________ Demonstrate sensitivity and responsiveness to patients’ culture, age, gender, and disabilities Systems-Based Practice __________ Understand how their patient care and other professional practices affect other health care professionals, the health care organization, and society and how these elements of the system affect their own practice (chart reviews with rotation faculty) __________ Know how types of medical practice and delivery systems differ from one another, including methods of controlling health care costs and allocating resources (part of clinical lecture series) __________ Practice cost-effective health care and resource allocation that does not compromise quality of care (chart reviews with rotation faculty) __________ Advocate for quality patient care and assist patients in dealing with system complexities __________ Know how to partner with health care managers and health care providers to assess, coordinate, and improve health care and know how these activities can affect system performance (experience on wards and in clinic on system-based performance in urology Rotation Specific Goals & Objectives for General Urology URO – II (UTMC) Overview The URO II Urology Resident has completed two years of general surgery and one year of Page 55 Department of Urology 2012-2013 general urology training. At the time of entering the URO II level the resident has reached the objectives as outlined for URO I in Urology. Goal: To continue progression from the foundation built on the URO I year with a broad range of objectives based on the six core competencies Objectives for URO II Residents: 1. Demonstrate ability that the objectives of URO I resident as outlined have been successfully achieved. 2. Perform minor and major urological procedures with supervision: (a) Demonstrate the ability to perform endoscopic procedures such as transurethral resection of the prostate gland, recognition of bladder tumors and resection of bladder tumors. (b) Ability to use laser for urological procedures. (c) Ability to perform minor and major open urological procedures with supervision. (d) Demonstrate ability to be not only the first assistant, but also the surgeon in certain minor and major urological procedures. 3. Demonstrate leadership and teaching for URO I residents and medical students. To have completed all of the objectives for URO I level and be familiar with the embryology of the genitourinary tract, congenital anomalies and evaluation and management of infertility. Understanding of vesicoureteral reflux, adrenal abnormalities and congenital anomalies and evaluation and management of infertility. Understanding of vesicoureteral reflux, adrenal abnormalities and genitourinary infections. Should have an evaluation plan for urinary incontinence and for erectile dysfunction. Accomplishment of the above objectives will be facilitated by the activities below. 1. The resident is responsible for 1) the admission of patients to the hospital including a history and physical exam and review of all relevant pre-operative workup, 2) assisting in surgery, and 3) follow-up and discharge planning. The resident is to be in close contact with the patient providing up-to-date progress reports and to anticipate any problems that might be encountered in the patient's recovery. Communication with the appropriate attending urologist is essential and mandatory. 2. The resident is required to participate in the evaluation and management of patients in the outpatient clinic setting. This includes an opportunity to perform outpatient endoscopy, rectal ultrasound and prostate biopsy, and urodynamic testing. 3. Throughout the year, and during all rotations, the URO II resident will be responsible for the evaluation and management of patients at TTH. They will have a supervising, full-time faculty member or a volunteer clinical faculty member in clinic during their own clinic for assisting in management and decisions. The resident is responsible for the initial history and physical exam, analysis of available laboratory and imaging studies, ordering additional studies, follow-up of results of the tests ordered, discussion of options for treatment with patients and their families, and follow-up after treatment. The resident will participate in the surgeries of patients seen in the clinic and followed in their clinic after surgery. Page 56 Department of Urology 2012-2013 4. The URO II resident will develop the ability to recognize urologic pathologic problems associated with the genitourinary system. The resident will observe, participate and have teaching-assistant based experience in emergency room urology, including the following: SPECIFIC OBJECTIVES - URO II - (UTMC): The resident will observe, participate and have teaching-assistant based experience in emergency room urology, including the following: __________ Post-operative evaluation __________ Evaluation of hematuria __________ Management and evaluation of stone disease __________ Evaluation of pediatric emergencies __________ Evaluation and management of pediatric and adult urologic emergencies __________ Experience with post operative complications The resident will observe, participate and have teaching-assistant based experience in clinicbased urology, including the following: __________ Evaluation of urologic cancers __________ Evaluation of stone disease, surgical and medical evaluation __________ Evaluation of pediatric urology disease __________ Evaluation of incontinence __________ Evaluation of impotence __________ Evaluation of voiding dysfunction __________ Evaluation of infertility __________ Experience with post operative complications The resident will perform and teach minor urology procedures, including the following: __________ Cystoscopy __________ Stent removal __________ Retrograde pyelogram __________ Testes biopsy __________ Penile biopsy __________ Prostate ultrasound __________ Prostate biopsy __________ Cystoscopic and fluoroscopic stent placement __________ Shock wave lithotripsy __________ CMG-EMG __________ Vasectomy __________ Varicocelectomy _________ Vasovasostomy _________ Scrotal surgery, including hernia/hydrocoele, orchiopexy _________ Videourodynamics Page 57 Department of Urology 2012-2013 The resident will perform and teach major urology cases, including the following: _________ Radical prostatectomy _________ Radical cystectomy _________ Continent diversion _________ Procedures for urinary incontinence _________ Radical nephrectomy _________ Donor nephrectomy _________ Percutaneous renal surgery _________ Endo-urology _________ Transurethral surgery, including TURBT and TURP _________ Laparoscopic urology _________ Pediatric urology including ureteral reimplantation, bladder augmentation, pediatric endourology, portions of hypospadias, pyeloplasty, major reconstructive procedures The resident will work towards development in the six core competencies: Patient Care _________ Communicate effectively and demonstrate caring and respectful behaviors when interacting with patients with urologic disease _________ Gather essential and accurate information about urologic patients _________ Make informed decisions about diagnostic and therapeutic interventions in urology based on patient information and preferences, up-to-date scientific evidence, and clinical judgment of urology faculty _________ Develop and carry out patient management plans for select urologic disorders _________ Counsel and educate patients and their families on urologic diseases _________ Use information technology (on-line journals, CD-rom educational programs, lectures) to support patient care decisions and patient education _________ Perform and assist competently medical and invasive procedures considered essential in outpatient urology _________ Provide health care services aimed at preventing health problems or maintaining health, particularly prostate cancer, bladder cancer, stone disease, impotence, voiding dysfunction _________ Work with health care professionals, including those from other disciplines Medical Knowledge _________ _________ Demonstrate an investigatory and analytic thinking approach to clinical situations Know and apply the basic (molecular biology) and clinically supportive sciences (nephrology, human oncology, transplantation) in urology _________ Analyze practice experience and perform practice-based improvement activities via chart reviews and personal feedback by rotation faculty Practice-Based Learning and Improvement Page 58 Department of Urology 2012-2013 _________ _________ _________ _________ _________ Locate, appraise, and assimilate evidence from scientific studies related to patients’ health problems Obtain and use information about SIU patients and the larger population from where their patients are drawn in clinical studies Apply knowledge of study designs and statistical methods to the appraisal of clinical studies and other information on diagnostic and therapeutic effectiveness, particularly when presenting at state and national meetings Use information technology to manage information, access on-line medical information Facilitate the learning of medical students and other health care professionals including mid-level providers, RNs, MAs Interpersonal and Communication Skills _________ _________ _________ _________ Create and sustain a therapeutic and ethically sound relationship with patients, particularly ward patients Use effective listening skills and elicit and provide information using effective nonverbal, explanatory, questioning, and writing skills Work effectively with others as a team member or leader of a health care team (urology service) Monitor colleagues for excessive stress and fatigue as taught in lecture series Professionalism _________ _________ _________ Demonstrate respect, compassion, and integrity; a responsiveness to the needs of patients and society that supercedes self-interest; accountability to patients, society, and the profession; and a commitment to excellence and on-going professional development Demonstrate a commitment to ethical principles pertaining to provision or withholding of clinical care, confidentiality of patient information, informed consent, and business practices at all times. Demonstrate sensitivity and responsiveness to patients’ culture, age, gender and disabilities Systems-Based Practice _________ _________ _________ _________ _________ Understand how their patient care and other professional practices affect other health care professionals, the health care organization, and society and how these elements of the system affect their own practice (chart reviews with rotation faculty) Know how types of medical practice and delivery systems differ from one another, including methods of controlling health care costs and allocating resources (part of clinical lecture series) Practice cost-effective health care and resource allocation that does not compromise quality of care (chart reviews with rotation faculty) Advocate for quality patient care and assist patients in dealing with system complexities Know how to partner with health care managers and health care providers to assess, coordinate, and improve health care and know how these activities can Page 59 Department of Urology 2012-2013 affect system performance (experience on wards and in clinic on system-based performance in urology) Rotation Specific Goals & Objectives for Pediatric Urology URO – II (SVMMC) Overview The URO II Urology Resident has completed two years of general surgery and one year of general urology training. At the time of entering the URO II level the resident has reached the objectives as outlined for URO I in Urology. Goal: To build on the foundation of the URO I year, have a dedicated pediatric rotation and progress to the next level of training. Objectives for URO II Residents: 1. Demonstrate ability that the objectives of URO I resident as outlined have been successfully achieved. 2. Perform minor and major pediatric urological procedures with supervision: (a) Demonstrate the ability to perform endoscopic procedures such as transurethral resection of the urethral valves, recognition of ureteralocele and intra vesical urethral abnormalities. (b) Ability to use laser for urological procedures. (c) Ability to perform minor and major open urological pediatric procedures with supervision. (d) Demonstrate ability to be not only the first assistant, but also the surgeon in certain minor and major urological procedures. 3. Demonstrate leadership and teaching for URO I residents and medical students. To have completed all of the objectives for URO I level and be familiar with the embryology of the genitourinary tract, and congenital anomalies Understanding of vesicoureteral reflux, adrenal abnormalities and congenital anomalies and evaluation and management of infertility. Understanding of vesicoureteral reflux, adrenal abnormalities and genitourinary infections. Should have an evaluation plan for urinary incontinence and for voiding dysfunction. Accomplishment of the above objectives will be facilitated by the activities below. 1. The resident is responsible for 1) the admission of patients to the hospital including a history and physical exam and review of all relevant pre-operative workup, 2) assisting in surgery, and 3) follow-up and discharge planning. The resident is to be in close contact with the patient providing up-to-date progress reports and to anticipate any problems that might be encountered in the patient's recovery. Communication with the appropriate attending urologist is essential and mandatory. 2. The resident is required to participate in the evaluation and management of patients in the Page 60 Department of Urology 2012-2013 outpatient clinic setting. This includes an opportunity to perform outpatient endoscopy, abdominal ultrasound and prostate biopsy, and urodynamic testing. 3. Throughout the year, and during all rotations, the URO II resident will be responsible for the evaluation and management of pediatric patients at SVMMC. They will have a supervising, full-time faculty member or a volunteer clinical faculty member in clinic during their own clinic for assisting in management and decisions. The resident is responsible for the initial history and physical exam, analysis of available laboratory and imaging studies, ordering additional studies, follow-up of results of the tests ordered, discussion of options for treatment with patients and their families, and follow-up after treatment. The resident will participate in the surgeries of patients seen in the clinic and followed in their clinic after surgery. 4. The URO II resident will develop the ability to recognize urologic pathologic problems associated with the genitourinary system. SPECIFIC OBJECTIVES – URO II – (SVMMC): The resident will observe, participate and have teaching-assistant based experience in emergency room urology, including the following: __________ Post-operative evaluation __________ Evaluation of hematuria __________ Management and evaluation of stone disease __________ Evaluation of pediatric emergencies __________ Evaluation and management of pediatric and adult urologic emergencies __________ Experience with post operative complications The resident will observe, participate and have teaching-assistant based experience in clinicbased urology, including the following: __________ Evaluation of voiding dysfunction __________ Evaluation of testicle & hernia __________ Evaluation of pediatric urology disease __________ Evaluation of infection __________ Evaluation of hypospadias __________ Evaluation of UPI obstruction __________ Evaluation of intense reflux __________ Experience with post operative complications The resident will perform and teach minor urology procedures, including the following: __________ Cystoscopy __________ Stent removal __________ Retrograde pyelogram __________ Testes biopsy __________ Prostate biopsy __________ Cystoscopic and fluoroscopic stent placement __________ Shock wave lithotripsy __________ CMG-EMG Page 61 Department of Urology 2012-2013 __________ Varicocelectomy _________ Scrotal surgery, including hernia/hydrocoele, orchiopexy _________ Videourodynamics The resident will perform and teach major urology cases, including the following: _________ UPI obstruction repair _________ Continent diversion _________ Procedures for urinary incontinence _________ Nephrectomy _________ Percutaneous renal surgery _________ Endo-urology _________ Transurethral surgery _________ Laparoscopic urology _________ Major reconstructive procedures The resident will work towards development in the six core competencies: Patient Care _________ Communicate effectively and demonstrate caring and respectful behaviors when interacting with patients with urologic disease _________ Gather essential and accurate information about urologic patients _________ Make informed decisions about diagnostic and therapeutic interventions in urology based on patient information and preferences, up-to-date scientific evidence, and clinical judgment of urology faculty _________ Develop and carry out patient management plans for select urologic disorders _________ Counsel and educate patients and their families on urologic diseases _________ Use information technology (on-line journals, CD-rom educational programs, lectures) to support patient care decisions and patient education _________ Perform and assist competently medical and invasive procedures considered essential in outpatient urology _________ Provide health care services aimed at preventing health problems or maintaining health, particularly prostate cancer, bladder cancer, stone disease, impotence, voiding dysfunction _________ Work with health care professionals, including those from other disciplines _________ To provide patient-focused care in the pediatric clinic while at SVMMC Medical Knowledge _________ _________ Demonstrate an investigatory and analytic thinking approach to clinical situations Know and apply the basic (molecular biology) and clinically supportive sciences (nephrology, human oncology, transplantation) in urology Practice-Based Learning and Improvement _________ _________ Analyze practice experience and perform practice-based improvement activities via chart reviews and personal feedback by rotation faculty Locate, appraise, and assimilate evidence from scientific studies related to patients’ health problems Page 62 Department of Urology 2012-2013 _________ _________ _________ _________ Obtain and use information about patients and the larger population from where their patients are drawn in clinical studies Apply knowledge of study designs and statistical methods to the appraisal of clinical studies and other information on diagnostic and therapeutic effectiveness, particularly when presenting at state and national meetings Use information technology to manage information, access on-line medical information Facilitate the learning of medical students and other health care professionals including mid-level providers, RNs, MAs Interpersonal and Communication Skills _________ _________ _________ _________ Create and sustain a therapeutic and ethically sound relationship with patients, particularly ward patients Use effective listening skills and elicit and provide information using effective nonverbal, explanatory, questioning, and writing skills Work effectively with others as a team member or leader of a health care team (urology service) Monitor colleagues for excessive stress and fatigue as taught in lecture series Professionalism _________ _________ _________ Demonstrate respect, compassion, and integrity; a responsiveness to the needs of patients and society that supercedes self-interest; accountability to patients, society, and the profession; and a commitment to excellence and on-going professional development Demonstrate a commitment to ethical principles pertaining to provision or withholding of clinical care, confidentiality of patient information, informed consent, and business practices at all times. Demonstrate sensitivity and responsiveness to patients’ culture, age, gender and disabilities Systems-Based Practice _________ _________ _________ _________ _________ Understand how their patient care and other professional practices affect other health care professionals, the health care organization, and society and how these elements of the system affect their own practice (chart reviews with rotation faculty) Know how types of medical practice and delivery systems differ from one another, including methods of controlling health care costs and allocating resources (part of clinical lecture series) Practice cost-effective health care and resource allocation that does not compromise quality of care (chart reviews with rotation faculty) Advocate for quality patient care and assist patients in dealing with system complexities Know how to partner with health care managers and health care providers to assess, coordinate, and improve health care and know how these activities can affect system performance (experience on wards and in clinic on system-based performance in urology) Page 63 Department of Urology 2012-2013 Rotation Specific Goals & Objectives for Transplant, Infertility & Research URO – III (UTMC) Overview The URO III resident has demonstrated competence in all requirements for URO I and URO II years and should be familiar with the entire spectrum of genitourinary disease. This year offers an opportunity to work in renal transplantation as well as general urology and having research experience. There’s also an opportunity to work at an outpatient fertility clinic to gain extra expertise in the management of the infertile patient. The expectation at this level of training is the independent evaluation of management of patients in the hospital and in the clinic. Specialty clinics both in renal transplantation and infertility will be managed with attending and volunteer faculty. The resident will rotate on clinical services in conjunction with the chief resident at the University of Toledo Medical Center. Goal: To build on the foundation of the URO I & URO II years and progress to the next level of training based on the six core competencies. Prepare to be a chief resident. Objectives for URO III Residents: Objectives and responsibilities of URO III in Urology will have input and will have assignments to the renal transplant service. The resident trained each year will also have time available for independent research pursuits. The responsibilities are: 1. 2. 3. 4. 5. 6. 7. 8. Developing an on call schedule for covering renal transplantation Participating in operative cases that deal with the removal of donated organs in both the living related and deceased environment. The involvement of the resident will be dependent upon his demonstrated level of expertise in surgical skills. Teaching of medical students in the operating room and the outpatient clinic and providing back up for on-call residents as deemed necessary. Teaching and conference responsibilities include participation in the transplant evaluation clinic and in the transplant morbidity and mortality conference, in addition to the transplant operations meeting. The resident will also be responsible for attending all other general urology conferences as provided by the schedule. Will participate in all aspects of renal transplantation including vascular and anastamosis and ureteral re-implantation. The resident will participate in transplant nephrectomy and secondary surgeries on transplant as deemed necessary. Administrative responsibilities entail the smooth coverage of the transplant service with the appropriate on-call schedules. Residents will also be responsible for picking cases for presentation in the TOPS meeting and the morbidity and mortality meetings as they relate to transplantation. Evaluation of research opportunities and participating in independent research either at the basic science level or at the chart review and database mining level. Participating in an outpatient infertility evaluation clinic under the appropriate guidance of a specially trained Urologist in infertility. Specific objectives: Page 64 Department of Urology 2012-2013 1. 2. 3. 4. 5. 6. 7. The resident will gain teaching experience and emergency room urology as it relates to transplantation including Foley catheter placement in a complicated system, postoperative evaluation, evaluation of fever of unknown origin, evaluation of stone disease in the transplant patient, evaluation of the management of rejection, experience with complications associated with transplantation. The resident will gain experience in minor urology procedures including cystoscopy, stent removal, retrograde polygram, transplant renal biopsy percutaneously. In addition, testes biopsy, vericosolectomy and . The resident will perform major urology cases including renal transplantation, the harvesting of renal organs. Ureteral re-implantation Transplant nephrectomy Reconstructive surgery in the transplant period Donor nephrectomy Involved in independent research with interactions with IAWL or IRB as deemed necessary. Project planning including assessment of proper power of the study. Data collation and integration. Manuscript preparation and presentation SPECIFIC OBJECTIVES - URO III - (UTMC) The resident will gain teaching experience in emergency room urology, including the following: __________ Complex foley catheterization __________ Post-operative evaluation __________ Evaluation of hematuria __________ Evaluation of stone disease __________ Evaluation of pediatric emergencies __________ Evaluation of adult urologic emergencies __________ Experience with complications such as rejection The resident will gain experience in minor urology procedures, including the following: __________ Cystoscopy __________ Stent removal __________ Retrograde pyelogram __________ Testes biopsy __________ Varicocelectomy __________ Scrotal surgery ___________Transplant renal biopsy The resident will perform major urology cases, including the following: __________ Renal transplant __________ Renal procurment __________ Uteral implantation __________ Procedures for urinary incontinence __________ Transplant nephrectomy __________ Percutaneous renal surgery Page 65 Department of Urology 2012-2013 __________ Basic endo-urology __________ Transurethral surgery, including TURBT and TURP The resident will work towards development in the six core competencies Patient Care __________ Communicate effectively and demonstrate caring and respectful behaviors when interacting with patients with urologic disease __________ Gather essential and accurate information about urologic patients __________ Make informed decisions about diagnostic and therapeutic interventions in urology based on patient information and preferences, up-to-date scientific evidence, and clinical judgment of urology faculty __________ Develop and carry out patient management plans for select urologic disorders __________ Counsel and educate patients and their families on urologic diseases __________ Use information technology (on-line journals, CD-rom educational programs, lectures) to support patient care decisions and patient education __________ Perform and assist competently medical and invasive procedures considered essential in outpatient urology __________ Provide health care services aimed at preventing health problems or maintaining health, particularly prostate cancer, bladder cancer, stone disease, impotence, voiding dysfunction __________ Work with health care professionals, including those from other disciplines __________ Provide patient-focused care in the uro-oncology clinic and stone clinic while at clinics assigned. Transplant and Infertility Medical Knowledge __________ Demonstrate an investigatory and analytic thinking approach to clinical situations __________ Know and apply the basic and clinically supportive sciences in urology Page 66 Department of Urology 2012-2013 Practice-Based Learning and Improvement __________ Analyze practice experience and perform practice-based improvement activities via chart reviews and personal feedback with the rotation faculty __________ Locate, appraise, and assimilate evidence from scientific studies related to patients’ health problems __________ Obtain and use information about patients and the larger population from where their patients are drawn in clinical studies __________ Apply knowledge of study designs and statistical methods to the appraisal of clinical studies and other information on diagnostic and therapeutic effectiveness, particularly when presenting at state and national meetings __________ Use information technology to manage information, access on-line medical information __________ Facilitate the learning of medical students and other health care professionals including mid-level providers, RNs, MAs Interpersonal and Communication Skills __________ Create and sustain a therapeutic and ethically sound relationship with patients, particularly ward patients __________ Use effective listening skills and elicit and provide information using effective nonverbal, explanatory, questioning, and writing skills __________ Work effectively with others as a team member or leader of a health care team (urology service) __________ Monitor colleagues for excessive stress and fatigue as taught in lecture series Professionalism __________ Demonstrate respect, compassion, and integrity; a responsiveness to the needs of patients and society that supercedes self-interest; accountability to patients, society, and the profession; and a commitment to excellence and ongoing professional development __________ Demonstrate a commitment to ethical principles pertaining to provision or withholding of clinical care, confidentiality of patient information, informed consent, and business practices at all times __________ Demonstrate sensitivity and responsiveness to patients’ culture, age, gender, and disabilities Page 67 Department of Urology 2012-2013 Systems-Based Practice __________ Understand how their patient care and other professional practices affect other health care professionals, the health care organization, and society andhow these elements of the system affect their own practice __________ Know how types of medical practice and delivery systems differ from one another, including methods of controlling health care costs and allocating resources (part of clinical lecture series) __________ Practice cost-effective health care and resource allocation that does not compromise quality of care __________ Advocate for quality patient care and assist patients in dealing with system complexities __________ Know how to partner with health care managers and health care providers to assess, coordinate, and improve health care and know how these activities can affect system performance (experience on wards and in clinic on system-based performance in urology) Rotation Specific Goals & Objectives for General Urology URO – IV (UTMC) Overview The Chief Resident will have demonstrated competence in all of the requirements for URO I, URO II and URO III, and should be familiar with the entire spectrum of genitourinary diseases. The expectation at this level of training is the independent evaluation and management of patients in the hospitals and in the clinic. Tailored supervision by the faculty for advice and oversight is expected because he or she will have matured in both judgment and technical skill to work independently. The Chief Resident will have administrative and teaching responsibilities, and will serve as a role model for the junior residents. The duties and expectation of the Chief Resident are the same as those outlined for the junior urology residents; however, the Chief Resident will have leadership and administrative responsibilities within the Division of Urology. Goal: Successful completion of URO I, URO II and URO III levels. Graduation from the residency program. Objectives for URO IV – (Chief) The Chief Resident in Urology will be the Administrative Chief and not be assigned to any particular clinic service. The Chief Resident will be responsible for: Page 68 Department of Urology 2012-2013 1) The resident on-call schedule. 2) In participation with the program chair, develop plan for resident coverage in periods of shortage of residents. 3) Resident coverage of operative cases on the basis of available manpower, level of resident experience, educational value of the cases, and service assignments. 4) The smooth transition of patient care responsibilities to the on-call resident. 5) Teaching medical students in the operating room and in the outpatient clinic settings, and providing backup for the on-call resident. 6) Teaching and conference responsibilities will be conducted with the approval of the Program Director. The Chief Resident has the responsibility to select cases for his or her own operating room experience on the basis of educational need and to complete the entire spectrum of operative cases by the time residency training is completed. Administrative responsibilities entail oversight of the resident on-call schedule and monitoring the selection and approval of vacation time for the resident staff. The Chief Resident will make every effort to resolve any conflict within the resident staff. Only those conflicts that are unresolved at that level will be brought to the attention of the Program Director. The selection of cases and topics for conferences are the responsibility of the Chief Resident. He or she will insure that the resident assigned to a case or topic has made adequate preparations, and will be prepared to make additional comments or fill in on any deficiencies at the time of the conference. SPECIFIC OBJECTIVES - URO IV- (UTMC): The resident will gain teaching experience in emergency room urology, including the following: __________ Complex foley catheterization __________ Post-operative evaluation __________ Evaluation of hematuria __________ Evaluation of stone disease __________ Evaluation of pediatric emergencies __________ Evaluation of adult urologic emergencies __________ Experience with complications The resident will gain experience in minor urology procedures, including the following: __________ Cystoscopy __________ Stent removal __________ Retrograde pyelogram __________ Testes biopsy __________ Penile biopsy __________ Varicocelectomy __________ Scrotal surgery The resident will perform major urology cases, including the following: Page 69 Department of Urology 2012-2013 __________ __________ __________ __________ __________ __________ __________ __________ __________ Radical prostatectomy Radical Cystectomy Continent diversion Procedures for urinary incontinence Radical nephrectomy Percutaneous renal surgery Basic endo-urology Transurethral surgery, including TURBT and TURP Pediatric urology The resident will work towards development in the six core competencies Patient Care _________ Communicate effectively and demonstrate caring and respectful behaviors when interacting with patients with urologic disease _________ Gather essential and accurate information about urologic patients _________ Make informed decisions about diagnostic and therapeutic interventions in urology based on patient information and preferences, up-to-date scientific evidence, and clinical judgment of urology faculty _________ Develop and carry out patient management plans for select urologic disorders _________ Counsel and educate patients and their families on urologic diseases _________ Use information technology (on-line journals, CD-rom educational programs, lectures) to support patient care decisions and patient education _________ Perform and assist competently medical and invasive procedures considered essential in outpatient urology _________ Provide health care services aimed at preventing health problems or maintaining health, particularly prostate cancer, bladder cancer, stone disease, impotence, voiding dysfunction _________ Work with health care professionals, including those from other disciplines _________ To provide patient-focused care in the pediatric clinic and stone clinic while at SVMMC Medical Knowledge _________ _________ Demonstrate an investigatory and analytic thinking approach to clinical situations Know and apply the basic (molecular biology) and clinically supportive sciences (nephrology, human oncology, transplantation) in urology _________ Analyze practice experience and perform practice-based improvement activities via chart reviews and personal feedback by rotation faculty Locate, appraise, and assimilate evidence from scientific studies related to patients’ health problems Obtain and use information about patients and the larger population from where their patients are drawn in clinical studies Apply knowledge of study designs and statistical methods to the appraisal of clinical studies and other information on diagnostic and therapeutic effectiveness, particularly when presenting at state and national meetings Practice-Based Learning and Improvement _________ _________ _________ Page 70 Department of Urology 2012-2013 _________ _________ Use information technology to manage information, access on-line medical information Facilitate the learning of medical students and other health care professionals including mid-level providers, RNs, MAs Interpersonal and Communication Skills _________ _________ _________ _________ Create and sustain a therapeutic and ethically sound relationship with patients, particularly ward patients Use effective listening skills and elicit and provide information using effective nonverbal, explanatory, questioning, and writing skills Work effectively with others as a team member or leader of a health care team (urology service) Monitor colleagues for excessive stress and fatigue as taught in lecture series Professionalism _________ _________ _________ Demonstrate respect, compassion, and integrity; a responsiveness to the needs of patients and society that supercedes self-interest; accountability to patients, society, and the profession; and a commitment to excellence and on-going professional development Demonstrate a commitment to ethical principles pertaining to provision or withholding of clinical care, confidentiality of patient information, informed consent, and business practices at all times. Demonstrate sensitivity and responsiveness to patients’ culture, age, gender and disabilities Systems-Based Practice _________ _________ _________ _________ _________ Understand how their patient care and other professional practices affect other health care professionals, the health care organization, and society and how these elements of the system affect their own practice (chart reviews with rotation faculty) Know how types of medical practice and delivery systems differ from one another, including methods of controlling health care costs and allocating resources (part of clinical lecture series) Practice cost-effective health care and resource allocation that does not compromise quality of care (chart reviews with rotation faculty) Advocate for quality patient care and assist patients in dealing with system complexities Know how to partner with health care managers and health care providers to assess, coordinate, and improve health care and know how these activities can affect system performance (experience on wards and in clinic on system-based performance in urology) Rotation Specific Goals & Objectives for General Urology URO – IV (SVMMC) Overview Page 71 Department of Urology 2012-2013 The Chief Resident will have demonstrated competence in all of the requirements for URO I, URO II and URO III, and should be familiar with the entire spectrum of genitourinary diseases. The expectation at this level of training is the independent evaluation and management of patients in the hospitals and in the clinic. Tailored supervision by the faculty for advice and oversight is expected because he or she will have matured in both judgment and technical skill to work independently. The Chief Resident will have administrative and teaching responsibilities, and will serve as a role model for the junior residents. The duties and expectation of the Chief Resident are the same as those outlined for the junior urology residents; however, the Chief Resident will have leadership and administrative responsibilities within the Division of Urology. Goal: Successful completion of URO I, URO II and URO III levels. Graduation from the residency program. Objectives for URO IV – (Chief) The Chief Resident in Urology will be the Administrative Chief and not be assigned to any particular clinic service. The Chief Resident will be responsible for: 1) The resident on-call schedule. 2) In participation with the program chair, develop plan for resident coverage in periods of shortage of residents. 3) Resident coverage of operative cases on the basis of available manpower, level of resident experience, educational value of the cases, and service assignments. 4) The smooth transition of patient care responsibilities to the on-call resident. 5) Teaching medical students in the operating room and in the outpatient clinic settings, and providing backup for the on-call resident. 6) Teaching and conference responsibilities will be conducted with the approval of the Program Director. The Chief Resident has the responsibility to select cases for his or her own operating room experience on the basis of educational need and to complete the entire spectrum of operative cases by the time residency training is completed. Administrative responsibilities entail oversight of the resident on-call schedule and monitoring the selection and approval of vacation time for the resident staff. The Chief Resident will make every effort to resolve any conflict within the resident staff. Only those conflicts that are unresolved at that level will be brought to the attention of the Program Director. The selection of cases and topics for conferences are the responsibility of the Chief Resident. He or she will insure that the resident assigned to a case or topic has made adequate preparations, and will be prepared to make additional comments or fill in on any deficiencies at the time of the conference. SPECIFIC OBJECTIVES - URO IV- (SVMMC): The resident will gain teaching experience in emergency room urology, including the following: __________ Complex foley catheterization __________ Post-operative evaluation __________ Evaluation of hematuria __________ Evaluation of stone disease Page 72 Department of Urology 2012-2013 __________ Evaluation of pediatric emergencies __________ Evaluation of adult urologic emergencies __________ Experience with complications The resident will gain experience in minor urology procedures, including the following: __________ Cystoscopy __________ Stent removal __________ Retrograde pyelogram __________ Testes biopsy __________ Penile biopsy __________ Varicocelectomy __________ Scrotal surgery The resident will perform major urology cases, including the following: __________ Radical prostatectomy __________ Radical Cystectomy __________ Continent diversion __________ Procedures for urinary incontinence __________ Radical nephrectomy __________ Percutaneous renal surgery __________ Basic endo-urology __________ Transurethral surgery, including TURBT and TURP __________ Pediatric urology The resident will work towards development in the six core competencies Patient Care _________ Communicate effectively and demonstrate caring and respectful behaviors when interacting with patients with urologic disease _________ Gather essential and accurate information about urologic patients _________ Make informed decisions about diagnostic and therapeutic interventions in urology based on patient information and preferences, up-to-date scientific evidence, and clinical judgment of urology faculty _________ Develop and carry out patient management plans for select urologic disorders _________ Counsel and educate patients and their families on urologic diseases _________ Use information technology (on-line journals, CD-rom educational programs, lectures) to support patient care decisions and patient education _________ Perform and assist competently medical and invasive procedures considered essential in outpatient urology _________ Provide health care services aimed at preventing health problems or maintaining health, particularly prostate cancer, bladder cancer, stone disease, impotence, voiding dysfunction _________ Work with health care professionals, including those from other disciplines _________ To provide patient-focused care in the pediatric clinic and stone clinic while at SVMMC Page 73 Department of Urology 2012-2013 Medical Knowledge _________ _________ Demonstrate an investigatory and analytic thinking approach to clinical situations Know and apply the basic (molecular biology) and clinically supportive sciences (nephrology, human oncology, transplantation) in urology _________ Analyze practice experience and perform practice-based improvement activities via chart reviews and personal feedback by rotation faculty Locate, appraise, and assimilate evidence from scientific studies related to patients’ health problems Obtain and use information about patients and the larger population from where their patients are drawn in clinical studies Apply knowledge of study designs and statistical methods to the appraisal of clinical studies and other information on diagnostic and therapeutic effectiveness, particularly when presenting at state and national meetings Use information technology to manage information, access on-line medical information Facilitate the learning of medical students and other health care professionals including mid-level providers, RNs, MAs Practice-Based Learning and Improvement _________ _________ _________ _________ _________ Interpersonal and Communication Skills _________ _________ _________ _________ Create and sustain a therapeutic and ethically sound relationship with patients, particularly ward patients Use effective listening skills and elicit and provide information using effective nonverbal, explanatory, questioning, and writing skills Work effectively with others as a team member or leader of a health care team (urology service) Monitor colleagues for excessive stress and fatigue as taught in lecture series Professionalism _________ _________ _________ Demonstrate respect, compassion, and integrity; a responsiveness to the needs of patients and society that supercedes self-interest; accountability to patients, society, and the profession; and a commitment to excellence and on-going professional development Demonstrate a commitment to ethical principles pertaining to provision or withholding of clinical care, confidentiality of patient information, informed consent, and business practices at all times. Demonstrate sensitivity and responsiveness to patients’ culture, age, gender and disabilities Systems-Based Practice _________ _________ Understand how their patient care and other professional practices affect other health care professionals, the health care organization, and society and how these elements of the system affect their own practice (chart reviews with rotation faculty) Know how types of medical practice and delivery systems differ from one another, including methods of controlling health care costs and allocating resources (part of clinical lecture series) Page 74 Department of Urology 2012-2013 _________ _________ _________ Practice cost-effective health care and resource allocation that does not compromise quality of care (chart reviews with rotation faculty) Advocate for quality patient care and assist patients in dealing with system complexities Know how to partner with health care managers and health care providers to assess, coordinate, and improve health care and know how these activities can affect system performance (experience on wards and in clinic on system-based performance in urology) Page 75 Department of Urology 2012-2013 CLINICAL TRAINING The clinical portion of the education is implemented so that a resident experiences a progressive exposure and responsibility in the examination, establishment of diagnosis, management of patients, and management of unexpected complications. The educational conferences are the foundation upon which the resident will build the knowledge of patient management. The clinical training is a progressive, concentrated, experiential training very carefully designed so that a resident, at the completion of residency training, becomes a safe, knowledgeable, and compassionate surgeon. During each year of the residency experience, clinical competence will be assessed on a quarterly basis by supervisory faculty based on direct observation at bedside, in the operating room, the out-patient clinics, and on work and teaching rounds. This information is recorded on evaluation forms, reviewed, and maintained in the resident file. General Competencies: It is expected that, during the training program, residents will become competent in the following six areas at the level expected of an independent surgical practitioner: patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice. Listed below are specific knowledge, skills, and attitudes required, as defined by the Accreditation Council for Graduate Medical Education (ACGME). 1. Patient Care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health. Urology residents must demonstrate manual dexterity appropriate for their training level and be able to develop and execute patient care plans. 2. Medical Knowledge about established and evolving biomedical, clinical, and cognate (e.g., epidemiological and social-behavioral) sciences and the application of this knowledge to patient care. Urology residents are expected to critically evaluate and demonstrate knowledge of pertinent scientific information. Page 76 Department of Urology 2012-2013 3. Practice-Based Learning and Improvement that involves investigation and evaluation of their own patient care, appraisal and assimilation of scientific evidence, and improvements in patient care. Urology residents are expected to critique personal practice outcomes and demonstrate recognition of the importance of lifelong learning in surgical practice. 4. Interpersonal and Communication Skills that result in effective information exchange and teaming with patients, their families, and other health professionals. Urology residents are expected to communicate effectively with other health care professionals, counsel and educate patients and families, and effectively document practice activities. 5. Professionalism, as manifested through a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population. Urology residents are expected to maintain high standards of ethical behavior, demonstrate a commitment to continuity of patient care, and demonstrate sensitivity to age, gender, and culture of patients and other health care professionals. 6. Systems-Based Practice as manifested by actions that demonstrate an awareness of and response to the larger context and system of health care and effectively call on system resources to provide optimal care. Residents are expected to practice high quality, cost-effective patient care; demonstrate knowledge of risk-benefit analysis; and demonstrate an understanding of the role of different specialists and other health care professionals in overall patient management. The following specifies the competency, the associated skill(s) required, and the corresponding evaluation methods utilized by the University of Toledo Urologic Residency Program. Page 77 Department of Urology 2012-2013 Patient Care Caring and respectful behavior: Checklist, patient survey Interviewing: Checklist, patient survey, simulated model Informed decision-making: Checklist, oral examination, chart simulated recall Develop and carry out patient management plans: Counsel and educate patients and families: Chart simulated recall, checklist Perform routine history and physical examination: Checklist, simulation model, chart review Perform procedures appropriate for level: Medical Procedures Checklist, case log, chart simulated recall Preventive health services: Checklist, case logs, records review Work within a team: Checklist, 360 evaluation Checklist, patient survey, simulated model Medical Knowledge Investigatory and analytic thinking: Oral examination, Chart simulated recall, Portfolio Knowledge and application of basic sciences: MCQ examination, oral examination, portfolio Practice-Based Learning and Improvement Analyze own practice for needed improvements: Portfolio, checklist Use of evidence from scientific studies: Portfolio, checklist, standard oral exam, chart simulated recall Application of research/statistical Checklist, Portfolio Page 78 Department of Urology 2012-2013 methods: Use of information technology: Portfolio, check list Facilitate learning of others: Checklist, 360 rating Interpersonal Communication Skills Respectful, altruistic: Checklist, patient survey, simulated model Ethically sound practice: Patient survey, checklist Sensitive to cultural, age, gender, disability issues: Simulated model, patient survey, checklist Systems-Based Practice Understand interaction of their practices with the larger system: Portfolio, Check list Knowledge of practice and delivery systems: Portfolio Practice cost-effective care: Checklist Advocate for patients within the health care system: Checklist, portfolio Goals & Objectives PGY 1 & 2- Surgery Prelim Education: During the first two years of urologic residency, the foundation for the care of the surgical patient is laid. Emphasis is placed on preoperative preparation and postoperative management. Preoperative preparation includes the taking of an accurate history and performing a detailed physical examination. Interpretation of pertinent lab data, EKGs, and radiographs is emphasized. In the postoperative period, fluid and electrolyte replacement, pain management, prevention of postoperative complications, drain management, and discharge planning are among the areas of emphasis. Page 79 Department of Urology 2012-2013 Resident participation in weekly urology and other specialty conferences is required. Patient Care Responsibilities: Increasing responsibility for patient care is delegated as competency develops during the first two years. Emphasis is placed on pre- and postoperative management. During the first two years, residents work closely with senior resident. Daily legible documentation of patient care is done within the framework of cost-effective delivery of care. Surgical skills, such as the proper handling of tissues, are emphasized in the operating room environment. Increasing opportunity for participation within the operating room is assumed as resident competency and skill increase. Technical Skills: It is anticipated that the skills needed for the proper handling of tissues will be developed within the first two years. Methods for incising tissue and wound closure are learned. The proper and appropriate use of different sutures is taught. Exposure to the techniques of plastic and vascular surgery is included in these first two years of training and serves as a basis for the reconstructive urologic techniques that will be encountered later in residency training. Basic endoscopic skills are introduced. Evaluation: Residents are evaluated by attending physicians as well as clinic support and hospital staff. Residents meet biannually with the Residency Program Director to discuss evaluations and attainment of educational goals. In-Service Examination: Residents are expected to participate in the in-service examination. Goals & Objectives PGY 3 - 6 Education: Education during the PGY-3 rotations includes the first steps in mastery of all aspects of the clinical activities for both adult and pediatric urology. During this time, the resident is expected to develop the core of clinical and basic sciences knowledge needed for the care of patients with urologic diseases. Examples of this knowledge include mastering the fundamentals of the interpretation of urologic imaging as intravenous pyelography, coaxial tomography, and renal ultrasonography. Familiarity with invasive examination of the genitourinary tract, cystoscopy, ureteroscopy, and transrectal ultrasonography is also developed. Core knowledge of the diagnosis and staging of urologic malignancies, diagnosis of calculus disease, forms of incontinence, as well as embryologic and pediatric urologic problems are developed through supervised patient contact and structured didactic sessions. Residents are expected to complete their first reading and study of the standard textbook of urology by the end of the academic year. The education process initiated in the PGY -3 year continues throughout the PGY-4 year. Residents continue to mature in their clinical diagnostic skills. The PGY- 4 has six months of dedicated pediatric service. They also have the opportunity to be the most senior residents on the urology service at Toledo Hospital. Page 80 Department of Urology 2012-2013 The PGY – 5 is the Transplant Research Year. The resident will have ample opportunity to participate in one of the many research projects within the department. Clinical education will revolve around all aspects of renal transplantation. The foundations of clinical immunology and immunosuppression will be mastered in this year as well as the elements of organ preservation. A fertility clinic rotation at Genito Urinary Surgeons (TTH affiliate) is also part of the PGY 5 year. Residents will continue to participate in all other scheduled teaching rounds, clinical duties, didactic sessions and on call activities during this year. The chief year, PGY -6 is the culmination of the residency training program. The chief resident will assume a major role in education leadership. It is expected that the chief resident will serve as a role model for junior residents and students, providing guidance in understanding the pathophysiology and management of urologic disease. General Urology Clinics: Goal 1 Perform a complete interview and accurate history from patients with urologic disorders encountered in the urology outpatient clinic setting Objectives – 8. Using appropriate and effective interview techniques, elicit and characterize an accurate history of the present illness from patients presenting with genitourinary complaints 9. Develop effective listening skills and be able to elicit and provide information using appropriate nonverbal and explanatory skills 10. Formulate and write coherent and legible notes in the medical record 11. Formulate treatment plans based on patient information and preferences for specific genitourinary diseases 12. Appropriately counsel and educate patients and their families about specific urologic problems 13. Be empathetic, understanding, compassionate and honest in dealings with patients and their families 14. Be sensitive and responsive to the urology patients’ culture, age, gender, and disabilities Goal 2 Perform a detailed and appropriately focused urologic physical examination Objectives – 7. Discuss and demonstrate ability to perform a detailed examination of the following genitourinary organ systems: a) Abdominal examination of the kidneys (inspection, palpation, percussion and auscultation) Page 81 Department of Urology 2012-2013 b) Inspection, percussion and palpation of the bladder c) Inspection and palpation of the penis d) Inspection, palpation and transillumination of the scrotum and its contents, including the testis, testicular tunics and adnexa, spermatic cord, and vas deferens 8. Discuss and demonstrate ability to perform a detailed male rectal examination to include: a) Assessment of the anal sphincter and lower rectum b) Prostate palpation to characterize its size, consistency, mobility, and the presence/absence of abnormalities, such as nodules or induration 9. Discuss and demonstrate an appropriate vaginal and rectovaginal examination in the female 10. Be able to perform and interpret a focused neuro-urologic examination 11. Demonstrate ability to recognize visually and to palpate enlarged lymph nodes in regions related to genitourinary disease and to discuss their importance relative to differential diagnosis to various disorders 12. When performing physical examination, to be sensitive and responsive to the patients’ culture, age and gender Goal 3 Accurate performance and interpretation of commonly performed urologic laboratory studies Objectives – 3. Demonstrate ability to perform and interpret the following laboratory studies a) routine urinalysis b) residual urine measurements c) expressed prostatic secretions d) semen analysis 4. Interpret and discuss the following laboratory studies a) serum PSA level and free/total PSA b) urinary electrolyte studies c) serum electrolyte studies and acid-base analysis d) serum creatinine and BUN e) creatinine clearance Goal 4 Performance and accurate interpretation of radiographic studies in the outpatient clinic setting Objectives – Page 82 Department of Urology 2012-2013 3. Be able to competently perform and interpret the following radiographic studies a) plain films of the kidney, ureters and bladder (KUB) b) intravenous pyelogram (IVP) c) retrograde pyelogram d) retrograde urethrogram e) voiding cystourethrogram (VCUG) f) transrectal prostatic ultrasound 4. Be able to accurately interpret an abdominal/pelvic CT scan, MRI scan, renal ultrasound and radionuclide studies of the genitourinary tract Goal 5 Performance of diagnostic and therapeutic procedures encountered in the urology outpatient clinic Objectives – 2. Be able to perform the following outpatient procedures a) transrectal ultrasound-guided prostate biopsy b) flexible and rigid cystoscopy c) suprapubic tube placement d) vasectomy e) spermatic cord and penile block f) circumcision g) intravesical administration of chemotherapeutic or immunotherapeutic agents h) urethral dilation Goal 6 Competent care and evaluation of the pre-operative and post-operative urologic patient Objectives – 13. Perform and write clear, legible and an appropriately detailed history and physical examination on all pre-operative patients 14. Prepare and write clear and detailed admission orders 15. Assess and discuss the operative and anesthetic risks of surgical procedures 16. Obtain informed consent for all surgical procedures 17. Understand the indications for obtaining consultation with other health care specialists prior to the surgical procedure in select patients 18. Discuss the physiologic response of the normal patient to surgical procedures and factors that modify these responses 19. Discuss and evaluate wound healing as it relates to surgical incisions 20. Treat and evaluate pain in a safe and effective manner in the post-surgical patient Page 83 Department of Urology 2012-2013 21. Discuss and evaluate the role of pharmacological agents, singly or in combination, and apply this knowledge to the care of the surgical patient 22. Understand the influence of other diseases and co-morbidities upon surgical care 23. Recognize and correct nutritional deficits in the surgical patient 24. Recognize and deal effectively with the psychological and emotional problems associated with anxiety imposed by urologic surgery ERECTILE DYSFUNCTION AND INFERTILITY : Goal 1 – Be proficient in the diagnosis, evaluation and treatment of patients with erectile dysfunction. Objectives 7. Describe the normal development and demonstrate the anatomy and function of the penis and male urethra 8. Describe the normal physiology of penile erection 9. List the etiologies of erectile dysfunction 10. Discuss common medical disorders associated with erectile dysfunction 11. Describe, in depth, the evaluation of patients with erectile dysfunction, including a sexual history, medical history, surgical history, physical examination, laboratory evaluation, and specialized testing 12. Describe, in detail, the various treatments of erectile dysfunction to include the following: a. medical treatment b. intracavernosal injection c. vacuum constriction devices d. psychological and sexual therapy e. surgical procedures implantation of penile prosthesis microvascular arterial bypass procedures Goal 2 – Demonstrate ability to diagnose, evaluate and treat patients with idiopathic priapism and prolonged penile erection secondary to intracavernosal injection of vasoactive drugs Objectives 8. Describe the normal development and surgical anatomy of the penis 9. Discuss disturbances in the mechanism of normal erection resulting in priapism 10. List and describe the various etiologic factors in priapism 11. Demonstrate the ability to take a pertinent history and physical examination in patients with idiopathic or PIP-induced priapism 12. Demonstrate knowledge of the diagnostic studies that are helpful in establishing the etiology of priapism Page 84 Department of Urology 2012-2013 13. Describe the vascular shunting procedures used in the treatment of priapism 14. Discuss the complications of each therapeutic method and appropriate treatment of these complications Goal 3 – Understand the basic science of male reproductive physiology and infertility Objectives 9. Demonstrate an understanding of the hypothalamic-pituitary-gonadal (HPG) axis and its endocrine control of testicular function 10. Identify the hormones involved in the HPG axis, their origins, function, reciprocal interrelationships and feedback control 11. List the endocrinopathies, both exogenous and endogenous, that may interfere with the normal testicular axial relationships and specify the nature of these alterations 12. Describe the anatomy, physiology, and pathophysiology of the male reproductive tract, spermatogenesis, sperm transport, and capacitation 13. Identify the sequence of sperm maturation, the cell types found within and between the seminiferous tubules and the time sequence of spermatogenesis 14. Describe the mechanism of ejaculation, including neurologic control and the anatomic structures involved 15. Identify disease states that interfere with ejaculation and the manner in which these states disrupt normal ejaculatory mechanisms 16. Describe the difference between emission and ejaculation Goal 4 Competent diagnosis, evaluation, and treatment of patients with male infertility Objectives 8. List the important components of a historical review in males presenting with infertility 9. Describe the components of the physical examination of infertile males 10. List the specific laboratory studies that should be obtained as part of the male infertility evaluation and the manner in which abnormal results may contribute to or reflect the extent of infertility 11. Select the surgical diagnostic techniques used in patients with male infertility including vasography, rectal sonography, and testicular biopsy 12. Identify exogenous drugs that may suppress fertility, ejaculation, and erectile dysfunction 13. Identify the appropriate surgical or medical therapies for patients with male infertility and defend the rationale and indications for clinical application of these modalities 14. List and describe, in detail, the assisted reproductive techniques commonly used in patients with male factor infertility Page 85 Department of Urology 2012-2013 UROLITHIASIS: Goal 1 Know the etiology and pathophysiology of urinary tract stone disease Objectives 6. Understand the epidemiology of urolithiasis to include the following: Geographic distribution of urinary calculus incidence in this country and the world Incidence in relation to race, sex, age, and climatic factors The effects of dietary and fluid intake on occurrence 7. Describe the crystalline architecture of urinary calculi and theoretical factors affecting crystallization 8. Describe the part played by matrix in the architecture and possible prevention or initiation of stone formation 9. Describe the role of urinary tract obstruction in the etiology of urolithiasis 10. Present a working classification of the etiology of stone disease to include the following: Renal tubular syndromes Enzyme disorders Hypercalcemic conditions Hypercalciuric states Uric acid lithiasis Secondary urolithiasis Iatrogenic urolithiasis Goal 2 Be proficient in the evaluation and diagnosis of a patient with urolithiasis Objectives 7. Elicit a history compatible with stone disease from a patient including a list of pertinent problems referable to stone formation 8. Discuss the information to be gained from urinalysis including the appearance of typical crystals 9. Know the relationship of stone formation to urinary bacteria and pH 10. Select appropriate serum studies in the evaluation of stone disease including assessment of serum creatinine, calcium, phosphate, and uric acid. 11. Describe the role of stone analysis in the diagnosis and treatment of patients with stone disease Page 86 Department of Urology 2012-2013 12. Have an in-depth knowledge of the radiographic evaluation of patients with stone disease, including the use of both plain film radiography and the CT urolithiasis study Goal 3 Select appropriate management strategies for patients with stone disease Objectives 5. Describe the role of dietary restriction and fluid intake modifications 6. Discuss, in detail, the medical therapy of patients with metabolic stone disease 7. Discuss, in detail, and perform various procedures used in the treatment of stone disease to include the following: ESWL Percutaneous nephrolithotomy Pyelolithotomy Ureteroscopy Cystolithotomy Lithopaxy 8. Given a patient with recurrent stone disease, develop a plan for follow-up care including metabolic evaluation, appropriate treatment by diet, fluid intake or medications and subsequent evaluation by radiographic studies Goal 4 Demonstrate competence in the use of ESWL in the treatment of urolithiasis Objectives 8. List the types of ESWL machines available, including the sources of energy, methods of coupling energy to patient, and the methods for imaging and targeting stones 9. Describe the physics of shock wave stone fragmentation, including the absorption of energy at the acoustical interface, internal reflections of shock wave within the stone, and cavitation bubbles 10. List the indications and contraindications for the use of ESWL 11. Be familiar with pre-lithotripsy management including the indications for pretreatment stents and selection of methods of anesthesia 12. Demonstrate ability to treat various stone types and describe initial energy levels used, total energy delivered, and the use of contrast to assist stone targeting 13. Discuss the post-treatment management of patients treated with ESWL 14. List the complications and risks of ESWL Goal 5 Develop competence in the use of endourologic techniques to treat upper urinary tract stones Page 87 Department of Urology 2012-2013 Objectives 12. Describe the surface relationships of the kidney and the structures traversed when a needle is passed into the renal pelvis through a posterior calyx 13. Know the intrarenal anatomy important to percutaneous renal access 14. Discuss the equipment commonly used in endourology, including guidewires, balloon dilators, stents, stone baskets and lithotriptors 15. Demonstrate knowledge of the various types of fluoroscopy equipment and the risks of fluoroscopy 16. Understand the technique of percutaneous nephrostomy placement, the use of fluoroscopy or ultrasound for guidance and the potential complications of this access procedure 17. Know the methods and instruments used for stone removal including forceps, baskets, and various grabbers, and know which stones can be removed with each 18. Discuss various methods of power lithotripsy, including ultrasound, electrohydraulic and laser lithotripsy 19. Know the complication of percutaneous stone removal and understand methods for their management 20. Discuss the appropriate selection of patients for percutaneous lithotripsy as compared to ESWL 21. Discuss the use of percutaneous stone dissolution and describe various chemolytic agents 22. List the complications specific to various types of stone dissolution techniques Goal 6 Develop competence in the use of endourologic techniques to treat lower urinary tract stones Objectives 6. Demonstrate ability to perform both rigid and flexible ureteroscopy in the treatment of ureteral and renal stones 7. Understand the use of baskets, forceps, and other devices for ureteroscopic stone removal 8. Have a thorough knowledge of lithotripsy methods used via the ureteroscope to fragment ureteral stones 9. Describe the immediate and long-term complications of ureteroscopy, including extravasation, ureteral stricture, and avulsed ureter 10. Discuss the indications for ureteroscopic stone extraction as compared to the use of ESWL in the treatment of ureteral stones PEDIATRIC UROLOGY: Page 88 Department of Urology 2012-2013 Goal 1 Diagnose, evaluate and treat pediatric patients with adrenal disease Objectives 7. Understand the physiology of the normal adrenal 8. Recognize the clinical manifestations of the adrenal-genito (A-G) syndromes 9. Institute appropriate diagnostic steps in evaluation of the A-G syndrome 10. Institute treatment of the A-G syndrome 11. Counseling of families of patients with the A-G syndrome 12. Recognize, evaluate and treat patients with benign and malignant neoplasms of the adrenal, including adrenal hemorrhage, adrenal adenoma, pheochromocytome, and neuroblastoma. Goal 2 Diagnose, evaluate and treat patients with space-occupying lesions of the kidney Objectives 5. Diagnose and manage the spectrum of cystic disease of the kidney 6. Diagnose Wilm’s tumor of the kidney 7. Understand the role of adjuvant therapies for the management of patients with Wilm’s disease 8. Understand the surgical approach to patients with Wilm’s tumor Goal 3 Develop expertise in the management of UPJ anomalies Objectives 6. Understand the role of prenatal ultrasound in the diagnosis of UPJ obstruction 7. Recognize the clinical spectrum of presentation of UPJ obstruction 8. Understand the role of renal nuclear scan in the management of patients with UPJ obstruction 9. Understand the various surgical approaches to the management of patients with UPJ obstruction 10. Understand followup strategies in patients having undergone repair Goal 4 Be familiar with the diagnosis and management of ureteral anomalies Objectives 6. Understand the embryology and physiology of the normal ureter 7. Recognize the clinical spectrum of the megaureter 8. Understand management strategies for the patient with a megaureter Page 89 Department of Urology 2012-2013 9. Recognize the clinical implication of the Meyer Weigert rule 10. Know the surgical options in the management of patients with ureteral duplication and associated renal anomalies Goal 5 Manage vesico-ureteral reflux Objectives 5. Know the classification system for vesico-ureteral reflux 6. Know and interpret the radiographic studies for the diagnosis of vesico-ureteral reflux 7. Understand the non-operative management of vesico-ureteral reflux 8. Know the surgical indications and techniques for the treatment of vesico-ureteral reflux Goal 6 Manage pediatric voiding dysfunction Objectives 8. Understand the role of urodynamics in the pediatric population 9. Know the options for management of the patient with enuresis 10. Understand the role of the urologist in the multidisciplinary management of patients with meningomyelocele 11. Understand the role of vesical augmentation in the patient with the neurogenic bladder 12. Understand the Mitrofanoff technique 13. Understand the indications for the Malone procedure 14. Discuss and understand the indications and surgical options for bladder neck reconstruction Goal 7 Management of pediatric undescended testicle Objectives 5. Know the embryology of the testes and testicular descent 6. Understand the indications for BHCG use in the management of the undescended testes 7. Know the indications for the use of laparoscopy in the management of patients with nonpalpable testes 8. Understand the surgical principals involved with the repair of the undescended testicle Goal 8 Page 90 Department of Urology 2012-2013 Management of the patient with ambiguous genitalia Objectives 4. Understand the full spectrum of the biochemical and genetic disorders which lead to intersex 5. Know the appropriate diagnostic steps in managing the patient with intersex 6. Understand the surgical management of the patient with intersex Goal 9 Management of the patient with urethral abnormalities Objectives 4. Understand the embryology of the urethra 5. Classify the various degrees of hypospadias 6. Become adept in the surgical management of the hypospadiac urethra UROLOGIC ONCOLOGY: Goal 1 Know how to diagnose, evaluate and treat patients with kidney cancer Objectives 10. Understand the normal development, function and surgical anatomy of the kidney 11. Identify and discuss the gross and histopathologic features of the various types of renal tumors 12. Discuss the natural history and epidemiology of kidney cancer 13. Know the paraneoplastic syndromes that may be associated with renal cell carcinoma 14. Know and discuss the clinical and pathological staging systems used for renal cancer, and identify the prognosis as a function of the TNM stage of disease 15. Discuss the evaluation and plan a course of therapy for selected patients with various stages of renal cell carcinoma 16. Demonstrate the ability to select the best surgical approach (radical vs partial vs laparoscopic nephrectomy) in patients with kidney cancer 17. Discuss adjuvant therapy for patients with renal cancer including the roles of radiotherapy, chemotherapy and the use of biologic response modifier therapies 18. Identify and discuss the appropriate follow-up, including the role of radiographic imaging, of patients after radical or partial nephrectomy for renal cancer Goal 2 Competent diagnosis, evaluation and treatment of patients with cancer of the renal pelvis and ureter Page 91 Department of Urology 2012-2013 Objectives 11. Understand the normal development, function and anatomy of the ureter and renal pelvis 12. Discuss the theories regarding the etiology of cancer of the renal pelvis and ureter, and know the natural history and risk factors for tumor progression 13. Know the histopathologic features of transitional cell carcinoma of the upper urinary tract, including evaluation of urinary cytology 14. Demonstrate the ability to elicit a history compatible with cancer of the upper urinary tract and discuss findings on physical examination 15. List and be able to interpret the appropriate laboratory studies necessary to diagnose and stage cancer of the renal pelvis and ureter 16. Accurately select and interpret imaging studies of the upper urinary tract 17. Demonstrate competence in evaluation of the ureter and renal pelvis using endoscopic techniques 18. Discuss the rationale for various surgical procedures used in the treatment of patients with ureteral or renal pelvic cancer, including the indications of nephronsparing approaches in selected patients 19. Discuss the rationale, methodology, agents used and potential toxicities of intracavitary agents used in the treatment of superficial tumors 20. For patients with invasive or metastatic tumors of the upper urinary tract, discuss the role and potential toxicities of systemic chemotherapy Goal 3 Competent diagnosis, evaluation and treatment of patients with cancer of the bladder Objectives 13. Understand the embryology, normal development, function and anatomy of the bladder 14. Discuss the epidemiology of the various forms of bladder cancer, the concepts of initiation and promotion of carcinogenesis and risk factors for bladder cancer development 15. Know the natural history of superficial and muscle invasive bladder cancer 16. Know and discuss the clinical and pathological staging systems used for bladder cancer, and identify the prognosis as a function of the TNM stage of disease 17. Demonstrate the ability to recognize the signs and symptoms of patients with bladder cancer and be able to perform a bimanual examination of the bladder under anesthesia 18. Demonstrate the ability to interpret the results of laboratory and imaging studies in the diagnosis and staging of bladder cancer 19. Demonstrate competence in the performance of urethroscopy and cystoscopy in the evaluation and follow-up of patients with bladder cancer 20. Describe the endoscopic approaches to treatment of bladder cancer Page 92 Department of Urology 2012-2013 21. Know and discuss the indications, efficacy, and complications associated with the use of intravesical therapies 22. Know and discuss the role of open surgical therapy for patients with bladder cancer, and discuss the role of lymph node dissection 23. Describe the various types of urinary diversion and considerations of their suitability in the context of extent of disease and patient preferences 24. Discuss the role of radiotherapy and chemotherapy in the treatment (adjuvant and therapeutic) of advanced bladder cancer Goal 4 Be proficient in the diagnosis, evaluation and treatment of patients with prostate cancer Objectives 13. Understand the embryology, normal development, function and anatomy of the prostate 14. Discuss the pathophysiology and theories regarding the etiology of prostate cancer 15. Know the gross and microscopic histopathology of prostate cancer and be able to differentiate these from other common histologic entities 16. Discuss the natural history and epidemiology of prostate cancer 17. Elicit a detailed and appropriate history from patients with prostate cancer 18. Demonstrate an ability to perform a digital rectal examination, including location and size of induration or nodules, pelvic sidewall and seminal vesicle extension of cancer 19. Discuss the appropriate diagnostic and staging studies used to evaluate cancer of the prostate and interpret their results 20. Demonstrate the ability to perform an adequate transrectal ultrasound and biopsy of the prostate, and understand the rationale for various biopsy strategies 21. Discuss the risks, complications, and benefits of the various treatment options for prostate cancer, and demonstrate the ability to select appropriate patients for each treatment modality 22. Discuss with patients and families the prognosis and complications associated with prostate cancer treatment and understand the medical and psychological management of these complications 23. Know the appropriate follow-up regimens for patients after radical prostatectomy and radiation therapy for prostate cancer 24. Discuss the indications and controversies surrounding the use of adjuvant therapy after definitive therapy (radical prostatectomy or radiotherapy) Goal 5 Competent diagnosis, evaluation and treatment of patients with testicular cancer Objectives Page 93 Department of Urology 2012-2013 13. Understand the embryology, normal development, function and surgical anatomy of the testis and paratesticular structures 14. Know and discuss the lymphatic drainage of the testicle and the pattern of lymphatic progression of disease to the retroperitoneum 15. Discuss various factors in the possible etiology of testis cancer 16. Know and differentiate the gross and histopathologic features of seminomatous, nonseminomatous and non-germ cell tumors 17. Demonstrate the ability to elicit a history compatible with testicular cancer 18. Perform a complete and accurate physical examination of patients with testicular cancer, including evaluation for lymphadenopathy or gynecomastia 19. List the appropriate diagnostic and staging studies used to evaluate cancer of the testicle or be able to interpret the results of these studies 20. Discuss the use of serum tumor markers in patients with testis cancer 21. Interpret testicular ultrasound and abdominal/pelvic CT findings in patients with testis cancer 22. Discuss the relative roles of retroperitoneal lymph node dissection and surveillance in patients with Stage I nonseminomatous testis cancer 23. Understand and discuss the selection of radiotherapy for the treatment of patients with testis cancer 24. Discuss various chemotherapeutic agents used in the treatment of advanced testis cancer and their relative value, depending on tumor type and stage Goal 6 Competent diagnosis, evaluation and treatment of patients with penile cancer Objectives 9. Understand the embryology, normal development, function and surgical anatomy of the penis and urethra 10. Discuss the incidence, epidemiology and potential etiologic factors of penile cancer 11. Identify and discuss treatment and follow-up of premalignant penile lesions 12. Know and use the TNM staging system for squamous cell carcinoma of the penis 13. Demonstrate an appropriate examination of the penis and inguinal lymph nodes in patients diagnosed with penile cancer 14. Describe the surgical treatment options and their applicability to various stages of penile cancer 15. Discuss the strategies and indications for inguinal lymph node dissection 16. Discuss the roles of radiotherapy and chemotherapy in the treatment of local and advanced penile cancer Goal 7 Understand the role of chemotherapeutic agents in the treatment of genitourinary malignancies Page 94 Department of Urology 2012-2013 Objectives 6. Classify the commonly used chemotherapy agents used in urologic cancers 7. Discuss the pharmacology of the various types of chemotherapeutic drugs used in the treatment of urologic cancers 8. Describe the current chemotherapeutic regimens for genitourinary cancers 9. Know the specific complications of chemotherapy, both immediate and long-term, and treatment of these conditions 10. Discuss the treatment results and expected response rates of chemotherapy regimens used for the treatment of various genitourinary malignancies Goal 8 Understand the role of radiotherapy in the treatment of genitourinary malignancies Objectives 8. Discuss the physical properties of ionizing radiation, including the fundamental units used to describe the interaction of radiation matter and the differences in penetration and absorption between different types of radiation 9. Know the differences between external beam and interstitial radiotherapy 10. Discuss the isotopes used for interstitial radiotherapy, including differences in energy emitted, half-lives and the clinical utilization of each 11. Discuss the biologic factors impacting the effectiveness of radiotherapy 12. Demonstrate a basic understanding of radiotherapy principles as it relates to genitourinary malignancy 13. Discuss the commonly employed curative and palliative radiotherapeutic doses, schedules and fields for urologic tumors 14. Demonstrate knowledge of potential complications of radiotherapy, both in general and those associated with the treatment of specific urologic tumors Renal Transplantation: Goal 1 Evaluate patients who are potential recipients of a renal transplant Objectives: 8. Understand the pathologic states that lead to ESRD 9. Recognize co-morbid states which influence outcomes of renal transplantation. 10. Evaluate the suitability of potential renal transplant recipients 11. Understand the systems-based issues surrounding the acquisition of a renal transplant 12. Know the various immunosuppressive agents and their potential toxicities Page 95 Department of Urology 2012-2013 13. Manage patients post transplantation immunosuppressive regimens 14. Perform renal transplantation with special emphasis of FEMALE UROLOGY: Goal 1 Understand the normal development, function and surgical anatomy of the female urethra, bladder and pelvis Objectives 5. Describe and explain the developmental processes by which the urethra progresses to tubular form and the hormonal influences in urethra development 6. Describe female urethral function by which urinary incontinence is maintained and the functional role of secondary structures, such as striated muscle 7. Know the blood, lymphatic, and nerve supply of the female bladder and urethra 8. Understand the normal anatomy and support of the female pelvis, including all involved organs and the supporting ligaments, muscle and fascia Goal 2 Competent evaluation, diagnosis and treatment of females presenting with urinary incontinence Objectives 6. Perform and demonstrate a complete medical history applicable of female patients presenting with urinary incontinence 7. Demonstrate an appropriate and complete physical examination of women with incontinence 8. Describe the laboratory studies that may assist with the diagnosis of women with incontinence 9. Demonstrate the ability to chose and carry out the appropriate therapy for the following conditions associated with female incontinence: Stress incontinence due to anatomical changes Stress incontinence due to sphincteric damage Urge incontinence and bladder instability Neurogenic bladder dysfunction Urinary retention and obstruction Urethral diverticula 10. Understand the role of pelvic floor neuromodulation in the treatment of patients with refractory voiding dysfunction due to pelvic floor dysfunction Goal 3 Page 96 Department of Urology 2012-2013 Know how to perform urodynamic studies in patients with voiding dysfunction Objectives 6. Discuss the value and indications for urodynamic evaluation of the lower urinary tract 7. Have an in-depth knowledge of the relationship of specific part of the urodynamic study to the filling/storage and emptying phases of micturition 8. Demonstrate the ability to independently set up and perform filling and voiding cytometry and be able to identify and interpret all of the following: Urinary flow rate Residual urine volume Flow patterns Bladder compliance Involuntary bladder contractions Abnormal bladder sensation Leak point pressures Bethanechol supersensitivity test Pressure/flow studies 9. Demonstrate the ability to independently set up and perform videourodynamics 10. Demonstrate the ability to independently set up and perform electromyography utilizing both needle and patch electrodes Goal 4 Know how to evaluate, diagnose and treat patients with pelvic pain syndromes, including interstitial cystitis Objectives: 12. Demonstrate an understanding of the epidemiologic aspects of interstitial cystitis 13. Be familiar with the common theories regarding the pathogenesis of interstitial cystitis 14. List the typical symptoms of interstitial cystitis in men and women 15. Discuss the differential diagnosis of the symptoms of interstitial cystitis 16. Be familiar with the cystoscopic findings in patients with interstitial cystitis and the indications and limitations of bladder biopsy 17. Explain the therapeutic rationale for the various treatments used in interstitial cystitis and be familiar with their benefits, efficacy and side-effects 18. List the systemic and intravesical pharmacotherapies used to treat interstitial cystitis 19. Know the role of bladder hydrodistention in patients with interstitial cystitis 20. Know the role of pelvic floor neuromodulation in the treatment of patients with interstitial cystitis and other pelvic pain syndromes 21. Know the role of surgical therapy for patients with refractory interstitial cystitis Page 97 Department of Urology 2012-2013 22. Demonstrate proper selection of interstitial cystitis patients for surgical therapies Goal 5 Be competent in the diagnosis and treatment of patients with vesicovaginal and ureterovaginal fistulae Objectives 8. List the signs and symptoms commonly associated with vesicovaginal (VVF) and ureterovaginal (UVF) fistulae 9. Describe the pathogenesis of VVF, including iatronic, post-irradiation and obstetric trauma induced fistulae 10. Describe the important components of the history and physical examination in patients with VVF and UVF 11. Distinguish between VVF and UVF using historical and diagnostic techniques 12. Discuss the surgical principles involved in repair of these fistulas including the biology of wound repair and the preparation of tissues for surgery 13. Describe the conservative management of VVF and UVF 14. Discuss in detail the surgical repair options for patients with VVF or UVF UROLOGIC SURGERY: Goal 1 Know the background, indications and potential complications of several commonly performed urologic operative procedures Objectives 2. Describe the rationale and indications for surgery, and list the complications associated with the following surgical procedures: Nephrectomy Partial nephrectomy Pyeloplasty Ureteroureterostomy Ureteroneocystostomy Augmentation cystoplasty Transureteroureterostomy Boari flap and psoas hitch Ileal conduit Ileal neobladder Goal 2 Develop and refine basic surgical techniques required for performance of some of the commonly performed surgical cases in urology Page 98 Department of Urology 2012-2013 Objectives: 2. Describe specific surgical techniques applicable to the following operative procedures: Nephrectomy Partial nephrectomy Ureteroureterostomy Ureteroneocystostomy Augmentation cystoplasty Transureteroureterostomy Boari flap and psoas hitch Ileal conduit Ileal neobladder Goals & Objectives The Toledo Hospital/St. Vincent Mercy Medical Center (site specific) Goals & Objectives PGY- 1 & 2 – Surgery Prelim Education: During the first two years of urology residency training, residents rotate on the clinical services at The Toledo Hospital (TTH), St. Vincent Mercy Medical Center (SVMMC) and St. Luke’s Hospital During these rotations, the foundation for urologic care of the patient is laid. Emphasis is placed on preoperative preparation and postoperative management in both the inpatient and outpatient settings. Preoperative preparation includes the taking of an accurate history and performing a detailed physical examination. Interpretation of pertinent lab data, EKGs, and radiographs is emphasized as they relate to planned surgical intervention. In the postoperative period, fluid and electrolyte replacement, pain management, prevention of postoperative complications, drain management, and discharge planning are among the areas of training emphasis. Patient Care Responsibilities: Increasing responsibility for patient care is delegated to the resident as competency develops during the first two years. During the first two years, residents work closely with senior residents. Legible daily documentation of patient care is done within the framework of cost-effective delivery of care. The management of consultations and the expeditious communication with referring services is emphasized. Surgical skills, such as the proper handling of tissues, are taught in the operating room environment. Increasing opportunity for participation within the operating room is assumed as resident competency and skill matures. An opportunity to work in an outpatient setting is afforded to the residents at Parkway Urology Center, a urologic outpatient center, affiliated with The Toledo Hospital parent system of ProMedica, Inc. Residents learn to obtain a complete history and physical examination in a Page 99 Department of Urology 2012-2013 timely fashion, and prepare patients for surgery with special attention to the patient’s concurrent medical problems as these effect the approach to solving a specific urologic problem. Technical Skills: Skills needed for the proper handling of tissues are developed within the first two years. Methods for incising tissue and wound closure are learned. Accurate and appropriate use of different sutures is taught. Basic endoscopic skills are introduced. Residents learn to use both rigid and flexible endoscopes for diagnostic procedures. Residents gain experience in the bedside management of patients with acute urologic problems. Evaluation: Residents are evaluated by attending physicians as well as by others (360 evaluation) with whom the resident works for the care of the patient. Goals & Objectives PGY –3 Education: Education during the PGY-3 rotations includes the first steps in mastery of all aspects of the clinical activities for both adult and pediatric urology. During this time, the resident develops the core of clinical and basic sciences knowledge required to care for patients with urologic diseases. In conjunction with the faculty at The Toledo Hospital and St. Vincent Mercy Medical Center, the residents master the fundamentals of the interpretation of urologic imaging, such as intravenous pyelography, coaxial tomography, and renal ultrasonography. The resident will also develop familiarity with invasive examination of the genitourinary tract, cystoscopy, ureteroscopy, and transrectal ultrasonography. Resident core knowledge of the diagnosis and staging of urologic malignancies, diagnosis of calculus disease, forms of incontinence, as well as embryologic and pediatric urologic problems develop through supervised patient contact and structured didactic sessions. Residents can expect their accumulating knowledge to be "tested" by faculty questions that assess the depth of resident knowledge of the clinical problem at hand. Patient Care Responsibility: PGY-3 residents are directly supervised by the Chief Resident. Daily rounds (except when off call on weekends, vacations and holidays) are made in conjunction with the Chief Resident. Efficient, expeditious and compassionate care-giving is developed. Residents are expected to develop basic bedside skills, such as suprapubic tube placement, use of filiforms and followers, catheter guides and flexible cystoscopy. Emergency room coverage and consultations are performed when on call in conjunction with the Chief Resident. Outpatient evaluations at Parkway Urology Center are of great importance in the PGY-3 training as a way to develop timely and cost-effective skills in the diagnosis and management of patients. Costs of patient management (pharmaceutical and lab expenses, etc.) are reviewed with the Chief Resident and attending physician in a prospective manner. Proper documentation of care in a problem-oriented and legible manner is emphasized. Technical Skills: In general, PGY-3 residents participate in all endoscopic and open procedures. Principals of surgical handling of tissues and basic endoscopic skills are further developed. Residents are expected to “first assist” on procedures commensurate with their level of surgical training and “second assist” on more technically advanced open cases. Page 100 Department of Urology 2012-2013 Evaluation: Residents are evaluated by attending physicians as well as support staff. Goals & Objectives PGY-4 Education: The education process initiated in the PGY-3 year continues throughout the PGY-4 year. Residents continue to mature in their clinical diagnostic skills. During this year, PGY-4 residents have the opportunity to be the most senior residents on the urology service at The Toledo Hospital and have six months of dedicated UT/Mercy Children’s Pediatric service at St. Vincent Mercy Medical Center. Faculty strive to enhance clinical confidence. Resident’s must obtain prior approval from attending for absence in coverage. Residents are expected to integrate their base of fundamental knowledge with the wide range of clinical urologic problems encountered at these sites. Patient Care Responsibilities: The PGY-4 resident is supervised by the attending at TTH and SVMMC Pediatric Urology service. During this year, the residents develop a mature attitude towards the responsibility of patient care which is reflected by marked attention to all details of patient management, from admission to discharge planning. Resident management of patients in the outpatient setting is now expeditious and focused. Consults and emergency room coverage (when on call) includes patient evaluation, the ordering of appropriate diagnostic tests, and the formulation of a treatment plan in conjunction with the attending physician. Technical Skills: During this year, PGY-4 residents develop their skills, both endoscopic and open surgical. In many cases, PGY-4 residents are the surgeon or they “first assist” the attending physician and are active participants in all aspects of the surgical case. Evaluation: Residents are evaluated by attending physicians as well as support staff. Goals & Objectives PGY – 5 Education: PGY – 5 is a year emphasizing research and renal transplantation. The resident will have ample opportunity to participate in one of the many research projects within the department. At the end of the PGY – 5 year it is anticipated that the resident’s activities will culminate in the production of new knowledge worthy of publication within a peer reviewed journal. Clinical education will revolve around all aspects of renal transplantation. The foundations of clinical immunology and immunosuppression will be mastered in this year as well as the elements of organ preservation. A fertility clinic rotation at the Genito Urinary Surgeons, Inc (TTH affiliate) which is held the fourth Wednesday of the month is also included during the PGY 5 year. Residents will continue to participate in all other scheduled teaching rounds, clinical duties, didactic sessions and on-call activities during this year. Patient Care Responsibilites: The PGY – 5 residents work with the PGY – 6 residents at UTMC to supervise the PGY – 3 residents. During this year, the PGY – 5 continues to develop advanced surgical skills (including open and laparoscopic surgeries). Residents also continue to Page 101 Department of Urology 2012-2013 develop advanced patient management skills with an emphasis on renal transplant and infertility. Technical Skills: Residents will develop the technical skills for the safe and efficient removal of kidneys during multi-organ retrieval. All aspects of renal transplantation will include the vascular and ureteral anastomoses will be mastered. In addition, the techniques of needle biopsy of transplanted kidneys, implantation and removal of CAPD catheters will be included in this year. Transplant nephrectomy as well as laparoscopic donor nephrectomies will be preformed. Evaluation: residents are evaluated by attending physicians as well as support staff Goals & Objectives PGY-6 Education: PGY-6, the Chief Resident (CR) year, is the culmination of the urology residency program. The CR assumes a major role in educational leadership. A diagnosis and management plan is synthesized by the CR prior to consultation with the attending physician, with documentation of the consult completed in a timely manner. The CR reviews junior residents’ assessments of the consults where appropriate. Consults to the emergency room are channeled through the CR prior to enlisting attending physician involvement unless such a pathway leads to delay in patient care management. The CR participates in urology outpatient clinic settings when not involved in the operating room or other aspects of direct patient care. Patient Care Responsibilites: The PGY – 6 resident directly supervises the PGY 3 & 4 residents at both UTMC and SVMMC as well as the PGY- 1 resident at SVMMC. They are responsible for leading daily patient rounds as well as distributing the daily work load including case coverage. This administrative role also includes creating the conference calendar and call schedules. Residents in this year guide junior residents in the formulation of a patient care plan in both an inpatient and outpatient setting. Technical Skills: The CR has a major responsibility in all urological surgeries. Upon completion of the PGY-6 year, the CR is able to demonstrate competence in all aspects of open surgical and endoscopic surgery. Evaluation: Residents are evaluated by attending physicians as well as clinic support staff. Page 102 Department of Urology 2012-2013 RESIDENT PROMOTION PROCESS The Department of Urology Resident Evaluation Committee (chaired by the program director) will review the clinical and academic performance and progress of each resident on a quarterly basis. Annually, the Department of Urology faculty will review the performance and progress of the resident during the academic year so as to assist the committee in determining his/her suitability for promotion or graduation. The program director will meet with the resident at a minimum of every six months to discuss performance evaluation. In the event that serious deficits are identified in the resident’s performance, meetings with the program director should be more frequent. The resident should be advised of deficits in performance by attendings with whom they work so as to receive timely feedback and opportunity for remediation. Department measures for resident evaluation are as follows: 1. Patient care and management on each rotation as documented by the faculty survey forms. Major performance deficits will result in a warning and may be grounds for probation. 2. Attendance at departmental academic conferences (Morbidity and Mortality, Lecture Series, etc.) which are mandatory for residents. Failure to attend more than 75% of any of these conferences will result in a warning and may be grounds for probation. 3. Performance on the annual American Board of Urology In-Service Exam. Failure to score above the 20th percentile will result in a warning and may be grounds for probation. 4. Performance on the annual Department of Urology Mock Oral Examination. Failure on either of these examinations will result in a warning and may be grounds for probation. 5. Contributions to the academic and scholarly mission of the Department. This will be evaluated by student and resident teaching, conference presentation and participation, and overall faculty assessment surveys. Major performance deficits will result in a warning and may be grounds for probation. 6. Compliance with all hospital and departmental record-keeping and documentation requirements. This includes timely completion of operative dictation, medical records, case lists (surgical operative logs), and Morbidity and Mortality reports. A pattern of lateness and noncompliance will result in a warning and may be grounds for probation. 7. Personal integrity, which includes strict avoidance of substance abuse, theft, lying, cheating, and unexplained absences. Failure to follow this standard will result in a warning and may be grounds for probation. Page 103 Department of Urology 2012-2013 When a resident receives a warning, a remedial program will be instituted in an attempt to correct the particular deficit(s). Failure to meet departmental standards after a resident has received a warning may result in a request to the Associate Dean for Graduate Medical Education to convene a hearing to evaluate the resident for placement on probation. Failure to meet departmental standards after a resident has been placed on probation will result in his/her expulsion from the program. The department reserves the right to summary expulsion of a resident from the program for severe infractions of departmental standards. If a resident is placed on probation and/or recommended for expulsion from the program, he/she may appeal in writing to the program director within fourteen (14) days of notification. An attempt to resolve the appeal should be accomplished within thirty (30) days. If the resident is not satisfied with the resolution proposed by the program director, he/she may submit an appeal to the Associate Dean for Graduate Medical Education, in accordance with the Due Process policies of the Medical College of Ohio. CALL/WORKING ENVIRONMENT Each hospital provides residents with on-call sleeping, lounge, library, and meal facilities. In-house resident call is not permitted to be more frequent than every third night (on average) for the duration of the program. Residents are not to average more than eighty (80) hours of work per week, barring exceptional patient care needs. Residents are provided (on average) one day out of seven free of all clinical responsibilities. The program director monitors working hours closely, but residents are also expected to report when working hours are excessive. (See attached Policy) CHIEF RESIDENTS The chief residents are primarily responsible for ensuring timely preparation of the resident call schedule, coordinating the visiting professor Case Management conferences, correcting resident call and coverage conflicts, and, in general, responsible for addressing administrative duties of the residency program operation under the supervision of the program director. Page 104 Department of Urology 2012-2013 RESIDENT RESPONSIBILITIES Communication: A key to the successful practice of medicine in general, and urology in particular, is prompt and effective communication with patients and their families and referring physicians. In general, residents are expected to: Discuss diagnostic and therapeutic plans and risks with patients and their families. Communicate plans and progress of all patients with attending surgeons, including any serious problems as they occur (including at night and on weekends). Notify referring physicians upon admission, operation, and discharge of their patients from the hospital. Medical Records: Complete patient care documentation is a requirement, and dictation is to be done on a timely basis. The following procedures are also outlined in the Medical College Hospital Physician’s Manual: A. The history and physical examination must be recorded in the patient’s chart within 24 hours of the patient’s admission. B. The discharge summary should include the following items in the order listed: 1. Patient name. 2. Patient 6-digit number. 3. Date of discharge. 4. Narrative summary, which should be a short summary of the patient’s hospitalization, including the reason for admission. 5. Hospital complications. 6. Consultations obtained. 7. Condition of patient at discharge. 8. Disposition. 9. Recommendations, including medications, diet, activity, and followup care. Discharge summaries must be dictated within 24 hours after discharge. C. All operative procedures must be dictated within 24 hours of surgery, preferably immediately following the procedure. D. All entries into the medical record must be legible and in black ink. E. All verbal orders are to be signed within 24 hours. F. All medical student notes must be countersigned by the resident or attending physician within 24 hours. Page 105 Department of Urology 2012-2013 Referrals and Consultations: Residents should respond promptly to all requests for patient referral or urologic consultations. Residents should promptly contact the responsible attending physician and the hospital Admitting Department, or the Urology Clinic when appropriate, to facilitate the referral. A faculty attending surgeon is assigned to urology/transplantation call each day. The “on-call” period rotates at 8:00 a.m. For the purposes of assigning a responsible attending, consult or referral is considered to be “received” at the time that a request is made to a member of the Department of Urology (resident, attending, or office). Consults directed to a specific attending are presented to that attending, not the attending on call. In-patient consultations are to be seen by the senior resident on the day of request. After evaluating the patient and writing an initial note, the senior resident should contact the appropriate attending surgeon who will complete the consultation. Emergency Room consults will be seen promptly under the direction of the senior resident and will be discussed with or seen by the responsible surgical attending prior to final disposition. Consult/referral patients will remain assigned to the responsible attending surgeon unless responsibility for the patient’s care is accepted by another attending surgeon. Arranging of transfers between attendings in the Department of Urology will not be delegated to residents, but will be done by direct communication between attendings. Clinics Residents should attend all clinics on services to which they are assigned. Every effort should be made for a resident to see patients, both preoperatively and postoperatively, for whom they are the responsible operating surgeon under faculty supervision. A resident from the appropriate service must be present at the start of all clinics and remain for the duration of the clinic until all patients have been seen, unless otherwise approved by the attending surgeon. Residents should report to the appropriate attending surgeons covering the clinic regarding all diagnostic and therapeutic decisions on outpatients. It is the responsibility of the resident to write or dictate a clinic note, order appropriate diagnostic studies, schedule inpatient ambulatory surgical procedures, and communicate with referring physicians, unless otherwise handled by the attending surgeon. Orders Residents are responsible for all patient orders, including admission, preoperative, postoperative, and discharge orders. Telephone orders must be signed as soon as Page 106 Department of Urology 2012-2013 possible, and no later than 24 hours after ordered. All orders must be dated and timed. Discharge orders should be written on the day prior to the anticipated discharge. Rounds Residents are expected to round at least once daily. These rounds should endeavor to appropriately incorporate the contribution of attending staff, nurses, and medical students in efficient diagnostic assessment and therapeutic planning for patient care. A computer printout of the service patient census, including name, hospital number, diagnosis, date of admission, operative procedure and date, surgeon, and referring physician, should be updated daily. The senior resident is expected to see that the progress of each patient is discussed daily with an attending surgeon. Progress Notes Daily notes (dated and timed) should be entered into the progress note section of the chart. Progress notes by medical students should be critiqued and must be countersigned by the resident. Notes should be brief but informative about patient condition, planned diagnostic or therapeutic measures, and discharge planning. Preoperative Notes For elective cases, the operating resident will review the chart (including X-rays, lab, and pathology) and discuss the operative plan with the attending surgeon prior to the operation. For inpatient elective cases, a preoperative note must be written by the resident surgeon in the progress section of the chart with 24 hours prior to operation and only after the patient has been examined by the same resident. It should include: Preoperative diagnosis and basis for diagnosis. Planned operation and indications. Surgeon. Anesthesia. Pertinent laboratory data. Blood/X-ray requests. Operative risks and indications of risks. Potential complications discussed. Signed consent. For outpatient elective cases, the charts will be reviewed the day prior to surgery and a preoperative checklist completed. It should include: 1. History & Physical /Consent completed 2. Pertinent laboratory data 3. Blood/X-ray requests Page 107 Department of Urology 2012-2013 4. Consults obtained Operating Room (OR) Schedule The responsible resident should review the OR schedule daily to ensure that all planned cases are listed. Residents should review the anatomy and technique of elective cases in standard atlases or by videotape. If you have not read before an elective case, do not plan to operate. If possible, briefly discuss the case with the attending surgeon on the day prior to the operation. Operating Room (OR) Etiquette A resident should be present in the OR area 10 minutes before induction of anesthesia (7:20 a.m. for 7:30 a.m. case). All anticipated instruments, supplies, and special equipment should be requested of the scrub and circulating nurses. The entire operative sequence should be briefly reviewed with the scrub nurse. Special anesthetic needs and patient positioning should be reviewed with the anesthesiologist. The roles of the operating surgeon and first and second assistants should be determined and clearly understood preoperatively. Professional behavior is expected at all times in the OR. Required preoperative preparation includes: Preoperative note and consent complete. Latest clinic note and lab results on chart. Relevant patient X-ray reports on chart. X-rays on view box. Operative Notes: Unless otherwise designated, the responsible resident should fill out an operative note (dated and timed) in the progress note section immediately following operation, to include: Preoperative diagnosis. Postoperative diagnosis. Operation. Surgeons and assistants. Anesthesia. Findings. Complications. Condition. Of note, a simple diagram of the operation performed (when appropriate) is very helpful. Page 108 Department of Urology 2012-2013 Operative Report Dictation: An operative note is dictated immediately upon completion of the operation. Usually this task is delegated to the operating resident, although the attending may wish to dictate the note himself/herself. The operative report should be brief but should cover all salient points of the procedure, including: Patient data. Preoperative and postoperative diagnoses. Operative procedure. Operating surgeon and assistants. Anesthesia. Operative findings. Operative procedure. Sponge and needle counts. Condition of patient. Statement that “the attending surgeon was present for the entire procedure” or “for all major portions of the procedure,” as the case may be. Operative Experience Record: All operative experience of residents is maintained on a computer database through the ACGME web site. These procedures will be entered into your personal record and kept on computer file, and you may review your experience at any time by requesting a “procedure work sheet” from the Residency Office. http://www.acgme.org/caselogs Page 109 Department of Urology 2012-2013 University of Toledo Department of Urology Name of Policy: Effective Date: Supervising Lines of Responsibility 04/2010 Policy Statement The Department of Urology Residency Program must ensure adequate supervision to facilitate patient care Purpose To delineate how and when residents should contact supervisors to ensure patient safety 1. All physicians (including resident physicians) are authorized and expected to do whatever is considered necessary to preserve life in the event of a life-threatening emergency. In the event of a life-threatening emergency, resident physicians should take whatever action deemed necessary to preserve life while someone else summons help from any available senior resident or faculty member. 2. All patients cared for in the UTMC Urology Residency Program are cared for under the direction of a designated faculty attending urologist. The specific level of faculty supervision will vary depending on the level of training and skill of the resident, the complexity of the care rendered, and the wishes of the responsible attending urologist. The level of supervision required for an individual procedure will be determined on an individual basis between the resident and the responsible faculty member unless a defined level of supervision is mandated by institutional or service policy. 3. Significant patient care decisions and events are to be discussed with the appropriate attending urologist. If the responsible attending surgeon is unavailable, contact the attending urologist on call for the appropriate service for the day. Although residents are responsible for their individual actions and senior residents are responsible for the performance of their service, overall responsibility for patient care always rests with the attending urologist. 4. Authority for supervision may be delegated, at the discretion of the attending urologist, to more senior urology residents. In general, the senior urology resident assigned to the service will be in charge of the service and is expected to assume a leadership role. Except in emergencies, the “chain-of-command” of junior resident senior resident attending urologist should be followed regarding patient care decisions. Under some circumstances, junior residents may work directly with attending surgeons. In these instances, the junior resident must keep the senior Page 110 Department of Urology 2012-2013 resident informed of significant events regarding the service. Individual resident assignments are to be made by the senior resident at the start of each rotation. 5. Attending urologists are responsible for ensuring that coverage is available for their patients by another attending urologist during their absence. Approved by: Steven H. Selman, M.D. ______________________________ Chairman & Program Director Page 111 Department of Urology 2012-2013 EDUCATION General: Residents develop knowledge and judgmental skills though a combination of didactic teaching in conferences and active participation in conferences and seminars, ward rounds, self-directed reading, audiovisual instruction, and attendance at local, regional, and national meetings. Attendance at teaching conferences is mandatory and attendance is documented, as stipulated by the Residency Review Committee for Urology. All conferences begin and end promptly at the appointed time. Seventy-five percent attendance is required of all residents at required conferences. Conference Schedule: Day Monday Friday Wednesday Time 5:00 pm – 6:00 pm 7:00 am – 8:30 am 7:00am -8:30am Conference Urology Chapter Review Campbell’s textbook & Quiz Journal Club Pathology Review M&M Indications/Grand Rounds GU Tumor Board Frequency Weekly Monthly 4th Friday of month 1st Wed 3rd Wed 2nd & 4th Wed DEPARTMENT OF UROLOGY RESIDENCY CONFERENCES DESCRIPTIONS **** 1. M&M – Wednesday, monthly M&M conferences cover all cases from the preceding calendar month, e.g. July M&M covers June 1 – 30 time period) from each hospital rotation site (MCO, MCH, SVMMC, TTH). Standardized forms case discussions are to be completed by urology residents from each service and signed by faculty moderator. ALL cases are to be listed on the form (including cases without M&M). 2. Grand Rounds – Wednesday, monthly Each resident to present a case with images. . Page 112 Department of Urology 2012-2013 3. Journal Club – Wednesday, monthly Chief resident will assign journal articles as early as possible. All articles are to be read by all residents to enhance discussion. 4. Chapter conferences – Monday, weekly Entire year chapter assignments, from Campbell’s textbook. All residents are expected to have read each chapter and discuss. 5. Pathology Conferences – Wednesday, monthly Held 4th Friday of the month. Dr. Lius De Las Casas - moderator 6. AUA Update conference will be scheduled per Chief Resident, covering assorted topics not covered in above lectures. 7. Quizzes – every Monday preceding conference 8. Technical Skills Lab – Monthly 9. Preoperative Patient Safety & Quality Assurance Conference – Weekly 10. Pediatric Indications - Weekly Urology Library: The Department of Urology maintains a library of major urological and surgical journals and textbooks, instructional videotapes. All residents are encouraged to use the library as a quiet study room. Materials should not be removed from the library. Priorities for library use are: 1. Formal resident or student conferences. 2. Scheduled departmental meetings that cannot be accommodated in other areas. 3. Informal educational meetings, lunches, or rounds. 4. Individual study. Use of the library is scheduled through the Department of Urology administrative office ( ext 3584). Residency Office and Lounge: Page 113 Department of Urology 2012-2013 The Urology Residency Office and Lounge are designed to provide an area for the facilitation of preparation of conferences and other teaching experiences, computer access for documenting procedures on the ACGME case log website, etc. Society Membership: Residents are encouraged to join appropriate professional societies such as the American Urologic Association, North-Central AUA, and Ohio Urological Society. Attendance at the Northwest Ohio Urologic meetings is required. Resident Research Presentations and Urology Review Courses: Residents are required to engage in clinical or laboratory research. With prior approval, residents will be reimbursed for attending any meeting at which they present a peerreviewed paper. In addition, chief residents will be reimbursed for travel and expenses to a major surgical meeting. Medical Student Teaching: Residents have a major role in teaching junior medical students assigned to their service. It is the policy of the Department of Urology that medical students rotate in the department for an educational opportunity and not in a service role. Thus, every effort should be made to provide students with time to learn, read, and develop basic skills in evaluation and management of surgical patients. Residents should make an effort to teach students at every opportunity, including rounds, clinics, and in the operating room. In the latter circumstances, students should participate only during selected parts of the operation in which they can learn or perform simple procedures, such as suturing the skin. Students are expected to attend all lectures and major conferences. At no time should a student miss a lecture or conference because of a commitment in the operating room or on the wards. Page 114 Department of Urology 2012-2013 RESEARCH AND EDUCATIONAL PROJECTS General: Each resident is encouraged to carry out clinical research with a faculty mentor, and submit the work for publication or presentation at a peer-reviewed meeting. Residents who are contemplating a career in academic urology should consider preparing for fellowship training. Clinical Research: Urology residents are encouraged to engage in clinical research during their training under the supervision of a faculty member of their choice. Such research may involve a chart review of a particular clinical problem, the report of a new operation or therapy, the impact of the surgical skill lab on operative technique, etc. Whatever subject is chosen, the resident should follow the steps necessary in carrying out quality research, including proper IRB approval, a careful description of the problem, appropriate review of the literature, definition of the variables to be recorded, gathering of data, data analysis, appropriate statistical analysis, generating a paper for presentation or publication, and solicitation of appropriate consultation and critique at each step of the process. Laboratory Research: Residents should choose a laboratory experience under an experienced investigator in a urologic or other clinical discipline or in a basic science laboratory. The resident must discuss funding for such research experience with the program director and, preferably, should work in a laboratory funded by extramural grant support. RESIDENT SELECTION Selection: Residents are selected for admission to the Department of Urology educational program based on several factors, including: 1. Eligibility for appointment in accordance with UTMC GME policy. 2. Academic and research achievement. 3. Evaluation of clinical performance and recommendations. 4. Demonstrated commitment to a urologic career. 5. Proficiency in written and spoken English sufficient for patient care. 6. Personal interview. Page 115 Department of Urology 2012-2013 Except under special circumstances approved by the program director, all applications for residency training are accepted through the ERAS system. Categorical positions are filled through the NRMP and AUA Match in January. A complete application includes a basic ERAS application, three recommendations, Dean’s letter, transcript, USMLE score, ECFMG transcript (if applicable), and previous ABUITE scores (if applicable). Selected applicants are invited for interview by e-mail or mail. AMERICAN BOARD OF UROLOGY IN-TRAINING EXAMINATION (ABUITE) Each year, all urology residents take the American Board of Urology In-Training Examination (ABUITE) on the first Saturday in November. This multiple-choice test of approximately 160 questions covers a wide variety of clinical and basic science topics in urology. The examination permits evaluation of performance as a percentile compared to PGY peers throughout the country. All residents should develop a systematic reading program throughout their training (and professional career). Such self-directed learning, Basic Science conferences, and Clinical Science conferences are all designed to assist residents in solidifying their cognitive knowledge. It is the goal of the Department of Urology to have residents perform at or above the national average (50th percentile) on the In-Training Examinations. Residents who perform at less than the 20th percentile are placed on academic warning status, and repeated poor performance may result in grounds for probation, particularly if other deficiencies exist. Resident Evaluation of Faculty, Rotation & Program Name of Policy: Resident Evaluation of Faculty, Rotation & Program Date: 4/2010 Policy Each resident will complete a confidential written evaluation of faculty and rotation twice a year. Purpose These constructive critiques are used to improve educational opportunities and faculty development, which will enhance resident training. In addition, the Program Director meets with the urology residents individually and a resident – Page 116 Department of Urology 2012-2013 elected representative participates in the Urology faculty meetings to exchange information and solicit constructive recommendations for improving the residency. All evaluations by residents are valued and taken seriously and in confidence. The evaluations are collected in a confidential manner and forwarded to the Program Director with a confidential summary to each faculty member. Approved by : Steven H. Selman, M.D. _______________________ Program Director & Chairman STIPENDS R1 $47,010 R2 $48,655 R3 $50,315 R4 $51,618 R5 $53,167 R6 $56,405 LICENSURE Residents should complete the USMLE examination series (USMLE steps I, II, and III) by the end of the R2 year. Residents who have not successfully passed steps I, II, and III by the end of the R3 year may not continue on the residency program. A medical license Page 117 Department of Urology 2012-2013 is not required for participation in the residency program. All residents must obtain a temporary Ohio license before beginning patient care at the Medical College Hospital or any of the affiliated hospitals. Temporary licensure packets will be issued in the Spring to allow enough time to process in order to begin residency on July 1. MOONLIGHTING NO moonlighting is allowed without written permission of the Program Director. Department of Urology Name of Policy : Moonlighting Effective Date : July 1, 2006 Policy No : 005 Policy “Moonlighting” is not formally recognized by the Urology Residency program of the University of Toledo, College of Medicine, Moonlighting is defined as any physician activity outside of the recognized residency training requirements. Purpose 1. To assure that residency education continues to be a full – time endeavor. 2. To assure that moonlighting does not interfere with the ability of the resident to achieve the goals and objectives of the educational program. 3. To maintain compliance with the ACGME Institutional Requirements. Procedure There is NO moonlighting allowed for any resident of the Urology Residency Program at the University of Toledo College of Medicine. Approved by: Steven H. Selman, M.D. Page 118 Department of Urology 2012-2013 __________________________Chairman, Department of Urology Steven H. Selman, M.D. __________________________Program Director, Department of Urology IDENTIFICATION The University of Toledo Medical Center and all affiliate hospitals require picture-type identification badges to be worn by the house staff at all times. I.D. cards will be issued by the campus police department. DRESS The expected dress for urology residents in the hospital includes: Gentlemen are expected to wear full-length trousers, dress shirt, tie, and a white laboratory coat. Shorts are unacceptable. Ladies are expected to wear dresses, skirts or dress slacks and a blouse, and a white laboratory coat. Shorts are unacceptable. Scrub suits are not to be worn during the day except when occasionally necessary “between cases” and then a white coat must be worn over the scrubs. VACATION Vacation time is granted as follows: PGY-1 3 weeks PGY 2 or above 4 weeks 15 working days 20 working days First year residents will take their vacation time in three separate one-week blocks. Second year residents or above will take their vacations in four one-week blocks. For every five week days requested, two weekend days of vacation will be granted. All vacation requests may be turned in to the Residency Office as of July 1 and will be granted on a first-come, first-served basis. Only one resident may be away from a given service during any given period. Deadline for all requests will be November 1. There will be no vacations granted during the last two weeks of June without permission of the Program Director. No vacations will be granted during the AUA or North-Central AUA Page 119 Department of Urology 2012-2013 meetings or in-service examination unless special approval is received from the Program Director. Residents who choose to interview for jobs or fellowships must do so during their allotted vacation time. It is the residents’ responsibility to budget their vacation time so that they have an appropriate number of days available for interviews. Leave for interviews must be approved in advance with a leave request form. Department of Urology Name of Policy: Leave of Absence Effective Date: 7/2007 Policy To ensure that the residency program provides residents with a written policy in compliance with ACGME and American Board of Urology requirements concerning the effect of leave of absence on satisfying the criteria for completion of the residency program. Purpose To ensure residents are aware of the effects concerning leaves of absence, for any reason, satisfying the criteria for completion of the residency program and to delineate restrictions and consequences of time away from resident training. 1. The resident is entitled to leaves of absence for vacation, health, medical and professional reason. The University of Toledo’s policies regarding leaves of absence are included in the University of Toledo policy. 2. The resident will be given three weeks ( 15 customary working days) of vacation leave during year one ( 1 ) and ( 4 ) weeks ( 20 customary working days) for two ( 2 ) and above. The vacation leave will not accumulate from year to year. 3. The resident is allowed up to three ( 3 ) weeks ( 15 customary working days ) of sick leave per year with pay. Sick leave will not accumulate from year to year. 4. The resident may attend a national meeting, conference or seminar for professional development purposes for up to seven ( 7 ) days with the permission of the Program Director. 5. The American Board of Urology requires Urology residents to work a minimum of (46) forty six weeks per year. That is, one year of credit must include at least (46) forty six weeks of full-time urologic education. Vacation or leave time may not be accumulated to reduce the total training requirement. If a circumstance occurs in which a resident does Page 120 Department of Urology 2012-2013 6. 7. 8. 9. not work the required (46)forty six weeks, the program director must submit a plan to the American Board of Urology for approval on how training will be made up, which may require an extension of the residency. The program director will determine each year if this requirement has been met. The resident is entitled to leaves of absence for medical and other reasons permitted by law. Any circumstances outside the purview of this policy will be decided on an individual basis by the Resident Education Committee. The Department of Urology abides by the Institutional Policy Leave of Absence including Maternity / Paternity Leave. For additional questions any resident may have regarding a leave of absence, shall be directed to the Human Resource Department at the University of Toledo. Approved by: Steven H. Selman, M.D. ________________________ Chairman & Program Director Page 121 Department of Urology 2012-2013 I have read the University of Toledo (UTMC) Department of Urology Resident Manual, including but not limited to the Goals and Objectives, Clinical Training, and Resident Promotion Process for the General Urology Residency at MCO; I agree with and accept these as a prerequisite to my training in this program. _______________________________________ Signature Date _______________________________________ Type or Print Name Page 122 Department of Urology 2012-2013