Contributors & References
advertisement
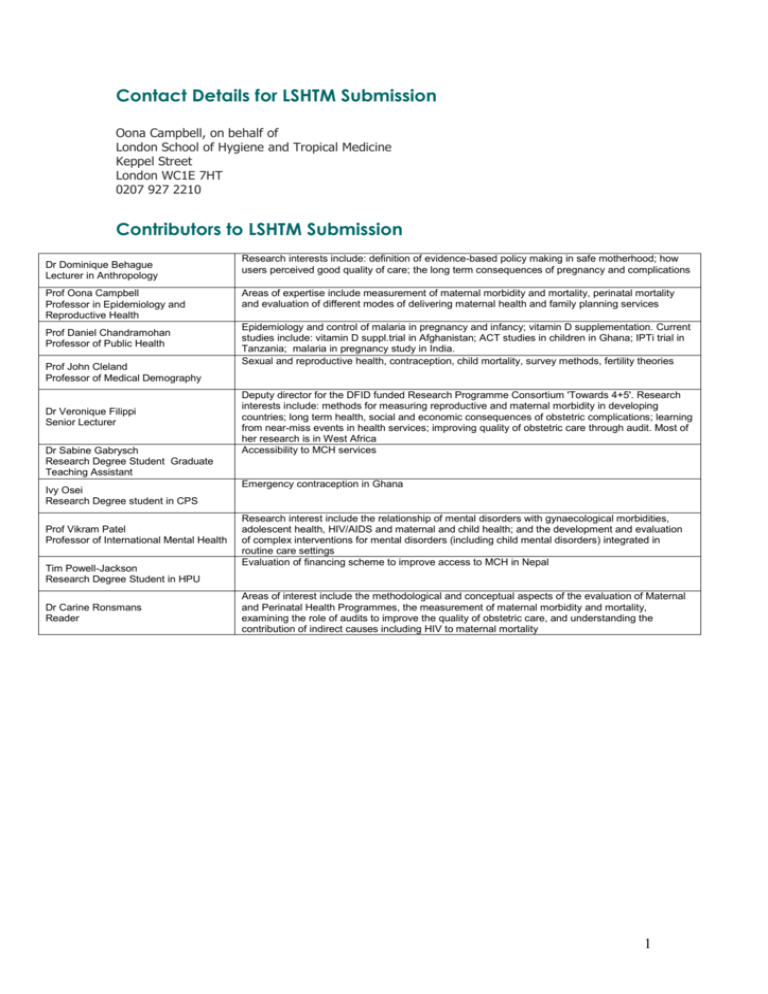
Contact Details for LSHTM Submission Oona Campbell, on behalf of London School of Hygiene and Tropical Medicine Keppel Street London WC1E 7HT 0207 927 2210 Contributors to LSHTM Submission Dr Dominique Behague Lecturer in Anthropology Prof Oona Campbell Professor in Epidemiology and Reproductive Health Prof Daniel Chandramohan Professor of Public Health Prof John Cleland Professor of Medical Demography Dr Veronique Filippi Senior Lecturer Dr Sabine Gabrysch Research Degree Student Graduate Teaching Assistant Ivy Osei Research Degree student in CPS Prof Vikram Patel Professor of International Mental Health Tim Powell-Jackson Research Degree Student in HPU Dr Carine Ronsmans Reader Research interests include: definition of evidence-based policy making in safe motherhood; how users perceived good quality of care; the long term consequences of pregnancy and complications Areas of expertise include measurement of maternal morbidity and mortality, perinatal mortality and evaluation of different modes of delivering maternal health and family planning services Epidemiology and control of malaria in pregnancy and infancy; vitamin D supplementation. Current studies include: vitamin D suppl.trial in Afghanistan; ACT studies in children in Ghana; IPTi trial in Tanzania; malaria in pregnancy study in India. Sexual and reproductive health, contraception, child mortality, survey methods, fertility theories Deputy director for the DFID funded Research Programme Consortium 'Towards 4+5'. Research interests include: methods for measuring reproductive and maternal morbidity in developing countries; long term health, social and economic consequences of obstetric complications; learning from near-miss events in health services; improving quality of obstetric care through audit. Most of her research is in West Africa Accessibility to MCH services Emergency contraception in Ghana Research interest include the relationship of mental disorders with gynaecological morbidities, adolescent health, HIV/AIDS and maternal and child health; and the development and evaluation of complex interventions for mental disorders (including child mental disorders) integrated in routine care settings Evaluation of financing scheme to improve access to MCH in Nepal Areas of interest include the methodological and conceptual aspects of the evaluation of Maternal and Perinatal Health Programmes, the measurement of maternal morbidity and mortality, examining the role of audits to improve the quality of obstetric care, and understanding the contribution of indirect causes including HIV to maternal mortality 1 References Aboagye, PK, Hailemichael G, Asare GO, Mitchell EMH, Addy J. (2007). Assessment of the readiness to offer contraceptive a comprehensive abortion care in the Greater Accra, Eastern and Ashanti regions of Ghana. Chapel Hill NC, Ipas, Adewuya, AO, Ola, BO, Aloba, OO, et al (2008) Impact of postnatal depression on infants' growth in Nigeria. J Affect Disord, 108, 191-193. Adisasmita A, Deviany PE, Nandiaty F, Stanton C, Ronsmans C. (2008). Obstetric near miss and deaths in public and private hospitals in Indonesia. BioMed Central Pregnancy and Childbirth, 8:10 Afenyadu D and Goparaju L. (2003). Adolescent sexual and reproductive health behaviour in Dodowa, Ghana, report submitted to Centre for Development and Population Activities. Ahiadeke, C. (2001). Incidence of Induced abortion in southern Ghana. International Family Planning Perspective, 27(2):96-101 & 108 Anoop S, Saravanan B, Joseph A, Cherian A, Jacob K. (in press). Maternal depression and low maternal intelligence as risk factors for malnutrition in children: a community based casecontrol study from South India. Arch Dis Child Appleby L, Warner R, Whitton A, et al (1997) A controlled study of fluoxetine and cognitive behaviour counselling in the treatment of postnatal depression. British Medical Journal, 314, 932-936. Araya R, Rojas G, Fritsch R, Gaete J, Simon G, Peters TJ. (2003). Treating depression in primary care among low-income women in Santiago, Chile: a randomised controlled trial. Lancet, 361:995-1000. Baggaley, RF, Ganaba, R, Filippi, V, et al (2007) Detecting depression after pregnancy: the validity of the K10 and K6 in Burkina Faso. Trop Med Int Health, 12, 1225-1229. Bang R, Bang A, et al. (2004). "Maternal morbidity during labour and the puerpurium in rural homes and the need for medical attention: a prospective observational study in Gadchiroli, India." BJOG: an International Journal of Obstetrics and Gynaecology 111: 231-238. Béhague, D, and Storeng K. (2008). "Collapsing the vertical-horizontal divide in public health: lessons from an ethnographic study of evidence-based policy making in maternal health." American Journal of Public Health Apr(98): 4. Bolton P, Bass J, Neugebauer R, Verdeli H, Clougherty K, Wickramaratne P, et al. (2003) Group interpersonal psychotherapy for depression in rural Uganda. JAMA, 289:3117-24. Brugha TS, Wheatley S, Taub NA, Culverwell A, Friedman T, Kirwan P, etal. (2000). Pragmatic randomized trial of antenatal intervention to prevent postnatal depression by reducing psychosocial risk factors. Psychol Med, 30:1273-81. Chandran M, Tharyan P, Muliyil J, Abraham S. (2002). Post-partum depression in a cohort of women from a rural area of Tamil Nadu, India. Incidence and risk factors. Br J Psychiatry, 181:499-504. Clarke EE. (2004). The experience of starting a poison control centre in Africa – the Ghana experience. Toxicology, 198(103):267-72 2 Cleland J, Bernstein S, Ezeh A, Faundes A, Glasier A, Innis J (2006) Family planning: the unfinished agenda The Lancet 368: 1810-1827 Collumbien M, Gerressu M, Cleland J. (2004)Non-use and use of ineff ective methods of contraception In Ezzati M, Lopez AD, Rodgers A, Murray CJL eds. Comparative quantifi cation of health risks: global and regional burden of disease attributable to selected major risk factors. Geneva: World Health Organization, 1255–320. Cooper P, Landman M, Tomlinson M, Molteno C, Swartz L, Murray L. (2002). The impact of a mother-infant intervention in an indigent periurban South African context: a pilot study. Br J Psychiatry, 180: 76-81. ECAF Consortium. Emergency contraception: a means to improve women’s reproductive health in Africa? Ongoing Elliott SA, Leverton TJ, Sanjack M, Turner H, Cowmeadow P, Hopkins J, et al. (2000). Promoting mental health after childbirth: a controlled trial of primary prevention of postnatal depression. Br J Clin Psychol, 39:223-41. Filippi V, Ronsmans C, Gandaho T, Graham W, Alihonou E, and Santos P (2000). Women’s reports of severe (near-miss) obstetric complications in Benin. Studies in Family Planning, 31(4):309-324. Filippi V, Ganaba R, Baggaley RF, Marshall T, Storeng K, Sombié I, Ouattara F, Ouedraogo T, Akoum M, Meda N. (2007).Women's health after a severe obstetric complication: Results from a longitudinal study in Burkina Faso. Lancet. 370: 1329-37 Filippi V, Ronsmans C, Gohou V, Goufodji S, Lardi M, Sahel A, Saizonou J, De Brouwere V. (2005). Maternity wards or emergency obstetric rooms? Incidence of near-miss events in African hospitals. Acta Obstetrica et Gynaecologica Scandinavica, 84:11-16 Gandhi MN, Welz T, Ronsmans C. (2004). An audit of life-threatening maternal morbidity in rural South Africa using ‘near-miss’ criteria adapted for primary level hospitals. International Journal of Gynecology and Obstetrics, 87:180-187 Ghana Demographic and Health Survey (2003). Ghana Statistical Service, Accra, Ghana, Noguchi Memorial Institute for Medical Research, Legon, Ghana, and ORC Macro, Calverton, Maryland, USA Ghana Statistical Service(GSS), Health Research Unit, Ministry of Health, and ORC Macro. 2003. Ghana Service Provision Assessment 2002. Calverton, Maryland: Ghana Statistical Service and ORC Macro Gohou V, Ronsmans C, Kacou L, Yao K, Bacci A, Filippi V. (2004). Responsiveness to lifethreatening obstetric emergencies in two hospitals in Abidjan, Côte d’Ivoire. Tropical Medicine and International Health, 9:406-415 Hanlon, C., Medhin, G., Alem, A., et al (2008) Detecting perinatal common mental disorders in Ethiopia: validation of the self-reporting questionnaire and Edinburgh Postnatal Depression Scale. J Affect Disord, 108, 251-262. Harpham, T., Huttly, S., De Silva, M. J., et al (2005) Maternal mental health and child nutritional status in four developing countries. J Epidemiol Community Health, 59, 1060-1064 Henry, R. and Fayorsey, C. (2002). Coping with Pregnancy: Experiences of Adolescents in Ga Mashi, Accra, Calverton, MD, USA: ORC Macro. 3 Holden JM, Sagovsky R, Cox J. (1989). Counselling in a general practice setting: controlled study of health visitor intervention in treatment of postnatal depression. BMJ, 298:223-6. Holden J. (1996) The role of health visitors in postnatal depression. Int.Rev.Psychiatry, 8, 7986. Hurt LS, Alam N, Dieltiens G, Aktar N, Ronsmans C.(2008). Duration and magnitude of mortality after pregnancy in rural Bangladesh. International Journal of Epidemiology, 37:397404 Klein, R. (2000). "From evidence-based medicine to evidence-based policy?" Journal of health services research and policy 5(2): 65-6. Konje JC, Obisesan KA, Ladipo OA. (1992). Health and economic consequences of septic induced abortion.Int J Gynaecol Obstet, Mar;37(3):193-7 Lanata C. (2001). Children’ health in developing countries: issues of coping, child neglect and marginalization. In: Leon D,Walt G, eds. Poverty, inequality and health. Oxford: Oxford University Press, 137-58. Lawn J, Tinker A, et al. (2006). "Where is maternal and child health now?" The Lancet 368(9542): 7-9. Mills A. (2005). "Mass campaigns versus general health services: what have we learnt in 40 years about vertical versus horizontal approaches?" Bulletin of the World Health Organization 83(4): 315-316. Murray L, Cooper P. (1997). Effects of postnatal depression on infant development. Arch Dis Child, 77:99-101. Obed SA, and Wilson JB. (1999). Uterine perforation from induced abortion at Korle –Bu Teaching Hospital, Accra, Ghana: A five year review. West African Medical Journal, 72(12):774-7 Patel V, Rodrigues M, De Souza N. (2002). Gender, poverty and post-natal depression: a cohort study from Goa, India. Am J Psychiatry, 159:43-7. Patel V, De Souza N, Rodrigues M. Postnatal depression and infant growth and development in low-income countries: a cohort study from Goa, India. Arch Dis Child 2003;88:34-7. Patel V, Chisholm D, Rabe-Hesketh S, Dias-Saxena F, Andrew G, Mann A. (2003). The efficacy and cost-effectiveness of a drug and psychological treatment for common mental disorders in general health care in Goa, India: a randomised controlled trial. Lancet, 361:339. Patel V, and Kirkwood B. (2008). workers. Lancet, 372, 868-9. Treating maternal depression with community health Pattinson R et al. (2003). Can enquiries into severe acute maternal morbidity act as a surrogate for maternal death enquiries? British Journal of Obstetrics and Gynaecology, 110:889-893 Prince M, Patel V, Saxena S, et al (2007) No health without mental health. Lancet, 370, 859877. Rahman A, Harrington R, Bunn J. (2002). Can maternal depression increase infant risk of illness and growth impairment in developing countries? Child Care Health Dev, 28:51-6. 4 Rahman A, Iqbal Z, Harrington R. (2003). Life events, social support and depression in childbirth: perspectives from a rural community in the developing world. Psychol Med, 33:1161-7. Rahman A, Lovel H, Bunn J, Iqbal Z, Harrington R. (2004). Mothers’ mental health and infant growth: a case-control study from Rawalpindi, Pakistan. Child Care Health Dev, 30:21-7. Rahman A, Malik A, Sikander S, et al (2008) Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. Lancet, 372, 902-909 Regmi S, Sligl W, Carter D, Grut W, Seear M. (2002). A controlled study of postpartum depression among Nepalese women: validation of the Edinburgh postpartum depression scale in Kathmandu. Trop Med Int Health, 7:378-82. Rojas G, Fritsch R, Solis J, et al (2007) Treatment of postnatal depression in low-income mothers in primary-care clinics in Santiago, Chile: a randomised controlled trial. Lancet, 370, 1629-1637 Ronsmans C, Filippi V. Reviewing severe maternal morbidity: learning from survivors from life-threatening complications. World Health Organization. Beyond the Numbers: Reviewing Deaths and Complications to Make Pregnancy Safer, Geneva: WHO; 2004:103-124 Ronsmans C, Achadi E, Cohen S, Zazri A. (1997). Women's recall of obstetric complications in South Kalimantan, Indonesia. Studies in Family Planning, 28:203-214 Ronsmans C, Scott S, Adisasmita A, Deviany P, Nandiaty F. (In press). Population-based incidence of pregnancy-related illness and mortality (PRIAM) in two districts in West Java, Indonesia. British Journal of Obstetrics and Gynaecology Sackett D, Rosenberg W, et al. (1996). "Evidence-based medicine: what it is and what it isn't." British Medical Journal 312(71-2). Stones W, Lim W, et al. (1991). "An investigation of maternal morbidity with identification of life-threatening 'near miss' episodes." Health Trends 23(1): 13-14. Van Gool K, Lancsar E, et al. (2002). "Diagnosis and prognosis of Australia's health information for evidence-based policy." Journal of health services research and policy 7(Supplement 1): S40-5. Walt G, Lush L, et al. (2004). "International organizations in transfer of infectious diseases: Iterative loops of adoption, adaptation, and marketing." Governance - An International Journal of Policy and Administration 17(2): 189-210. Wickberg B, Hwang CP. (1996). Counselling of postnatal depression: a controlled study on a population based Swedish sample. J Affect Disord, 39: 209-16. 5