Chapter 29 MATERNAL-FETAL TESTING
advertisement
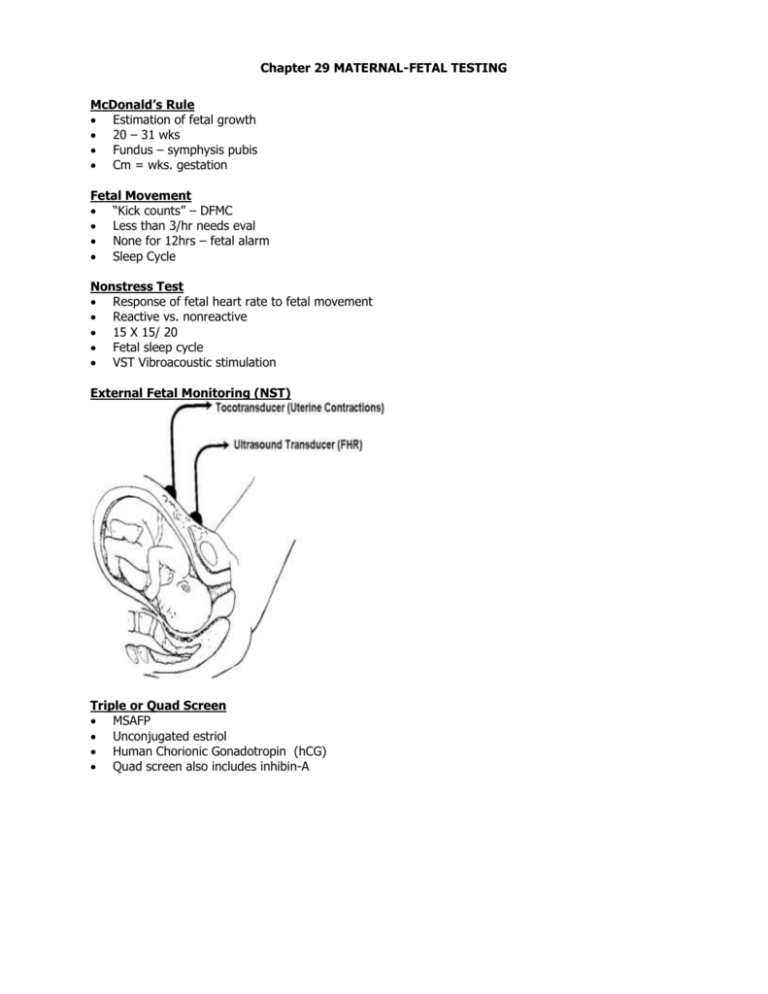
Chapter 29 MATERNAL-FETAL TESTING McDonald’s Rule Estimation of fetal growth 20 – 31 wks Fundus – symphysis pubis Cm = wks. gestation Fetal Movement “Kick counts” – DFMC Less than 3/hr needs eval None for 12hrs – fetal alarm Sleep Cycle Nonstress Test Response of fetal heart rate to fetal movement Reactive vs. nonreactive 15 X 15/ 20 Fetal sleep cycle VST Vibroacoustic stimulation External Fetal Monitoring (NST) Triple or Quad Screen MSAFP Unconjugated estriol Human Chorionic Gonadotropin (hCG) Quad screen also includes inhibin-A Neural Tube Defects (NTD) Nonclosure of neural tube Affects brain and spine Spina bifida ( 50%) o Occulta o Cystica: myelomeningocele,myelocele o Anencephaly (40%) most severe o Myelomeningocele FETAL PROFILE OF ANECEPHALY o Encephalocele (10%) Dx: AFP in amniotic fluid, acetylcholinesterase 28 days¯ p conception, o spina bifida occulta from incomplete closure of one or more vertbera without protrusion of spinal cord or meninges o may have dimple or depression, tuft of hair, port wine stain o may have no neuro deficit X, foot weakness, bowel/bladder disturbance Neuro deficit below level of contents in external sac in myelomeningocele, paralysis, incont. Clubfoot, hydrocephalus (90%), poss. Mental retardation. Rx: Surgery to close defect, can not reverse neuro def. CAUSE: isolated birth defect, teratogen, multiple malformation, chromosomal T13 or 18. Lack of folic acid. Inc in N and S Carolina Maternal serum Alpha-fetoprotein (MSAFP) Produced by fetal liver Screening tool 16 –18 wks Correlate with gestational age, maternal age,weight, race, Type I DM in NTD, multifetal pregnancy, intestinal atresia Contraction Stress Test (CST) FHR and UC monitoring Initiate UC via nipple stimulation or infusion of oxytocin Assess for uteroplacental insufficiency Positive, negative, suspicious Hyperstimulation Contraindications Persistent and consistent late decels occuring with> 50%UC’s is positive test Hyperstim. >90 sec or q. 2min Contraindications: PTL, Pl Pr, Pl abr, classical scar, etc Chorionic Villi Sampling (CVS) Genetic/chromosomal testing Earlier diagnosis (10-12 wks) and rapid results but more risk that amniocentesis Transcervical or transabdominal o RhOGam for Rh¯ mothers Percutaneous Umbilical Blood Sampling (PUBS) PUBS = cordocentesis Direct access to fetal circulation Needle into fetal umbilical vessel Inherited blood disorders, isoimmunization, fetal infection, acid base, karyotyping, fetal blood type, rbc and platelets Intrauterine transfusion Kleihauer-Betke o to determine if blood is fetal in origin RhO Gam for Rh¯ Done at 18 wks, need specialists Amniocentesis Analysis of amniotic fluid Biologic: Chromosomes Chemical: AFP, bilirubin, lecithin/sphingomyelin (L/S) ratio (3rd trimester) After week 14 – 2nd trimester Complications < 1% After wk 14:uterus is abdominal organ, more amniotic fluid Dx: genetic, congenital (NTD), pulmonary maturity, fetal hemolytic disease how long does it take to get results? RhOgam for Rh¯ neg mothers Ultrasound Use of sound waves to produce real time images in three dimension. When sound strikes an object, echo is returned Transabdominal or transvaginal o Transvag useful early on: ectopic pregnancies, monitor devel embryo, id abnormalities and est GA Multiple indications and uses Limited or comprehensive o Limited: confirm pregnancy, fetal viability, multipl gestation. presentation, locate placenta, malformations, amniotic fluid vol. o Comprehensive: abnl fetus, abnl exam, poly or oligo,elev AFP, Hx of abnl offspring Also needed for cvs, pubs, amnio.detect maternal abnl, est or confirm dates, IUGR, macrosomia, pl previa, abrutio placenta, BPP, AF assessment, placental maturity,fetal well being Full bladder for abd US when it is an abdominal organ (after 1st trimester). Pelvic tilt for transv. p.819 for chart Multiple gestation FHR activity 6 –7 weeks by ehco o 10 –12 weeks by Doppler GA determination : o Gestational sac 8 wks o CRL 7 – 12 wks o BPD after 12 wks o Femur after 12 wks Serial measurements in later gestational age 2, preferably 3 plotted against nl growth curvesbetw 2432 wks teilds est error of 10days +/_ Fetal nuchal translucency (FNT) 10 - 14 wks o Greater than 3mm – genetic disorder or anomaly Placental position and function o Seen 14 – 16 wks low lying until 3rd trimester o Graded 0 –3 o Calcium deposits/ postterm Normal Nuchal Translucency Abnormal Nuchal Translucency Ultrasound Placenta Ultrasound Fetal Head Ultrasound Fetal Body Ultrasound Fetal Head Fetal US US Placenta/UC Fetal Growth Poor maternal weight gain IUGR Chronic infections DM HTN Macrosomic Symmetric IUGR reflects chronic or longstanding insult:low genetic growth, intrauterine infection, malnutrition, smoking, chromosomal abnormality Asymmetric IUGR: placental insufficiency D/T HTN, CV, renal disease Macrosomic >4000gm, dystocia, traumatic injury, asphyxia. Infant diabetic mother, assymetric HC nl, increased fat and muscle in shoulders and abd Biophysical Profile Noninvasive dynamic fetal assessment o Fetal breathing movements (FBM) o Fetal movements o Fetal tone o Fetal Heart Rate (FHR) o Amniotic fluid volume (AFV) Graded 0 - 10 See handout First Fight I LOVE YOU






