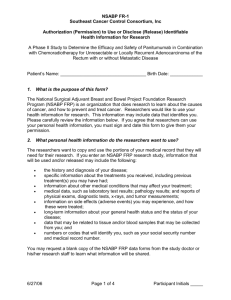
NSABP FR-1 (7.28.06) - Southeast Clinical Oncology Research
advertisement

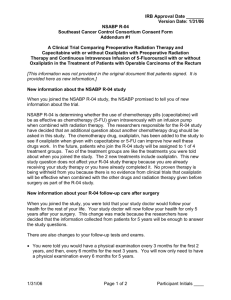
IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form A Phase II Study to Determine the Efficacy and Safety of Panitumumab in Combination with Chemoradiotherapy for Unresectable or Locally Recurrent Adenocarcinoma of the Rectum With or Without Metastatic Disease What is a research study? This is a clinical trial, a type of research study. Your study doctor will explain the clinical trial to you. Clinical trials include only people who choose to take part. Please take your time to make your decision about taking part. You may discuss your decision with your friends and family. You can also discuss it with your health care team. If you have any questions, you can ask your study doctor for more explanation. Why have I been asked to take part in this study? You are being asked to take part in this study because you have cancer of the rectum that will not be removed by surgery at this time. Your doctor has told you that other treatments, including a combination of drugs and radiation therapy, are recommended at this time. Who is conducting the study? The National Surgical Adjuvant Breast and Bowel Project (NSABP) Foundation Research Program (FRP) is conducting the study. (The NSABP institution must supply appropriate information as to who is conducting the trial locally.) Why is this study being done? There are several reasons why this study is being done: To learn how rectal cancer tumors such as yours respond to a combination of chemotherapy drugs plus another new drug called panitumumab given before radiation therapy begins and then along with radiation therapy of the pelvis. The chemotherapy drugs used in this study are oxaliplatin and capecitabine. Both are commonly used to treat rectal cancer. Panitumumab is an investigational drug (still being researched) and is a type of drug called a monoclonal antibody. Panitumumab attaches to an area found on normal cells and on cancer cells called an epidermal growth factor receptor. When panitumumab attaches to this area on the cell, it blocks a protein called epidermal growth factor (EGF) from being able to attach to the cell. When EGF is blocked, the growth of the cell slows down or stops. Panitumumab may also help radiation therapy work better. 6/27/06 Page 1 of 16 Participant Initials _____ IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form To determine if adding panitumumab to chemotherapy and radiation therapy will help decrease the size of your rectal cancer. To learn if your tumor will respond well enough to the panitumumab, chemotherapy, and radiation therapy treatments to make it possible for your surgeon to remove your tumor by surgery. To learn about the side effects of panitumumab when combined with chemotherapy and with the combination of chemotherapy and radiation therapy. How many people will take part in the study? About 65 people will take part in this study. What will happen if I take part in this research study? Before you begin the study: You will need to have the following exams, tests or procedures to find out if you can be in the study. These exams, tests, and procedures are part of regular cancer care and may be done even if you do not join the study. If you recently have had any of these tests, exams, or procedures listed below, they may not need to be repeated. This will be up to your study doctor. medical history and physical exam an examination by a surgeon to be sure you are not a candidate for surgery at this time blood tests to check your blood counts and how well your kidneys and liver are working CT scan of your chest CT or MRI scan of your abdomen and pelvis PET scan of your whole body endoscopic exam (a procedure using a scope to examine your rectum and colon) pregnancy test (if you are a woman of childbearing potential) You will also need the following blood test which is not part of regular cancer care and are being done for the purpose of this study: blood test to measure the amounts of calcium, potassium, and magnesium in your blood. During the study: If the exams, tests, and procedures listed above show that you can be in the study, and you choose to take part, you will begin study treatment within 2 weeks after joining the study. Your study treatment will be divided into two parts. 7/28/06 Part 1: During the first part, you will be treated with the drugs oxaliplatin, capecitabine, and panitumumab. You will receive these study drugs beginning every 14 days. The 14 days between the first day you receive your therapy and the next time you receive your therapy is called a cycle. On the first day of each cycle, you will receive panitumumab through a vein. This will take about 30-60 minutes. After receiving panitumumab, oxaliplatin will be given through a vein. This will take about 2 hours. 6/27/06 Page 2 of 16 Participant Initials _____ IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form Also, on the same day, you will begin taking another chemotherapy drug called capecitabine. Capecitabine is taken by mouth with a full glass of water twice a day about 30 minutes after eating breakfast and dinner. You will take capecitabine for the first 7 days of each 14-day cycle. Your doctor may ask you to keep track of the capecitabine pills you take by writing in a diary or on a calendar. After taking capecitabine for 7 days, you will have 7 days without treatment. The oxaliplatin, capecitabine, and panitumumab will be repeated every 14 days for 4 cycles. Part 1 of your therapy will take about 8 weeks. After you complete the first part of your study treatment, you will have a rest period of about 1 to 2 weeks. Part 2: During the second part of your treatment, you will receive panitumumab and capecitabine in addition to radiation therapy to your pelvis which includes the rectal tumor area. You will receive radiation therapy 5 days out of every 7 days (usually Monday through Friday) for about 6 weeks. On the first day of each week, you will receive panitumumab through a vein over a period of about 30-60 minutes. You will receive panitumumab once a week for 6 weeks. Also on the first day of each week, you will again begin taking capecitabine by mouth twice a day with a full glass of water about 30 minutes after eating breakfast and dinner. During this part of your treatment, you will take capecitabine 5 days a week on the days you are scheduled to receive radiation therapy (for about 6 weeks). If, for some reason, you miss your regularly scheduled radiation therapy treatment, you will still take the capecitabine doses for that day. Your doctor may ask you to write in a diary or on a calendar to record each dose of capecitabine that you take. Because these drugs are being given at the same time as radiation therapy, the doses of both capecitabine and panitumumab are lower than the doses used during Part 1 of therapy. 6/27/06 Page 3 of 16 Participant Initials _____ IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form A summary of your study treatment is outlined below: TREATMENT – PART 1 Panitumumab + Oxaliplatin given through a vein on Day 1 every 14 days for 4 cycles + Capecitabine taken by mouth twice a day on Days 1 through 7 every 14 days for 4 cycles TREATMENT – PART 2 Radiation Therapy 5 days a week for about 6 weeks + Panitumumab given through a vein once a week for 6 weeks + Capecitabine taken by mouth twice a day for 5 days a week on the days you are scheduled to receive radiation therapy (about 6 weeks) Surgery may or may not follow the completion of study therapy. During Part 1 of your study therapy: You will have the following tests and exams. They are part of regular cancer care. physical exam before every cycle of therapy blood tests to check your blood counts before every cycle blood test to check how well your kidneys and liver are working every other cycle You will also have the following test every 4 weeks which is not part of regular cancer care and is being done for the purpose of this study: blood test to check the levels of magnesium, potassium, and calcium in your blood After you complete the first part of your therapy: You will have the following tests and exams. These tests and exams will be done before you begin radiation therapy. They are part of regular cancer care. physical exam blood tests to check your blood counts and how well your kidneys and liver are working CT scan to help plan your radiation therapy treatments 6/27/06 Page 4 of 16 Participant Initials _____ IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form You will also have the following test which is not part of regular cancer care and is being done for the purpose of this study: Blood test to check the levels of magnesium, potassium, and calcium in your blood During Part 2 of your study therapy: While you are receiving capecitabine, panitumumab, and radiation therapy, you will have the following tests and exams at least every 2 weeks. They are part of regular cancer care. a physical exam blood tests to check your blood counts blood tests to check how well your kidneys and liver are working You will also have the following test every 2 weeks which is not part of regular cancer care and are being done for the purpose of this study: blood test to check the levels of magnesium, potassium, and calcium in your blood After your study therapy: About 4-6 weeks after completion of your study therapy, you will have the following tests and procedures. All of these are part of regular cancer care with the exception of the blood tests to check the levels of magnesium, potassium, and calcium in your blood and the PET scan. physical exam blood tests to check your blood counts and how well your kidneys and liver are working blood tests to check the levels of magnesium, potassium, and calcium in your blood CT scan of your chest (if you had any areas of tumor in your chest before you joined the study.) CT scan or MRI of your abdomen and pelvis If the CT scan or MRI of your abdomen and pelvis shows your rectal tumor has not decreased in size, your doctor will discuss further treatment options with you. If the CT scan or MRI of your abdomen and pelvis shows your pelvic tumor has decreased in size or shows no signs of remaining tumor in your pelvis, and your study doctor and surgeon recommend surgery to remove tissue from the area where your tumor had been, then your study doctor will schedule a PET scan before surgery. You will also have an examination of your rectum using a scope to look closely at the area where your rectal tumor had been to confirm your tumor's response to the study therapy (this may be done at the time of your surgery). 6/27/06 Page 5 of 16 Participant Initials _____ IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form If the CT scan or MRI of your abdomen and pelvis shows your pelvic tumor has decreased in size or shows no signs of remaining tumor, and your doctor has determined it is not in your best interest to have surgery to remove your rectal tumor, you will then be scheduled to have a PET scan, as well as a repeat CT or MRI scan of your abdomen and pelvis, about 6 weeks later to again check your tumor’s response to the study therapy. If the PET scan and repeat CT scan or MRI show that your tumor has responded well enough to the study treatment, your doctor will schedule an examination of your rectum using a scope to check the area where your tumor was located to confirm whether or not there is visible rectal tumor remaining. If surgery is performed: You will have a doctor’s visit to see how you are doing about 8 weeks after your surgery. Whether or not you have surgery: We would like to continue to check on your health status about 12, 18, and 24 months from the time you joined the study. How long will I be in the study? You will be in the study for 2 years. During that time, your study therapy will last for about 4 months, unless your cancer gets worse or you or your doctor decide you should stop. You will have tests and exams to check how your cancer responded to the therapy during the 1-3 months after you complete your radiation therapy. The NSABP would like to keep track of your medical condition about every 6 months for 2 years from the time you joined the study. Can I stop being in the study? Yes. You can decide to stop at any time. Tell the study doctor if you are thinking about stopping or decide to stop. He or she will tell you how to stop safely. It is important to tell the study doctor if you are thinking about stopping so any risks from the study therapy can be evaluated by your doctor. Another reason to tell your doctor that you are thinking about stopping is to discuss what follow-up care and testing will be most helpful for you. You can choose to withdraw in one of two ways. In the first way, you can stop your study treatment, but still allow the study doctor to report your health status to the NSABP Foundation Research Program until 2 years after you jointed the study. In the second, you can stop your study treatment and request that no new information be reported to the NSABP. 6/27/06 Page 6 of 16 Participant Initials _____ IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form Can anyone else stop me from being in the study? Your study doctor may stop you from taking part in this study at any time if he or she believes it is in the best interest for your health, if you do not follow the study rules, or if the study is stopped by the NSABP. What side effects or risks can I expect from being in the study? You may have side effects while on the study. Everyone taking part in the study will be watched carefully for any side effects. However, doctors do not know all the side effects that may happen. Side effects may be mild or very serious. Your healthcare team may give you medicines to help lessen side effects. Many side effects go away soon after you stop taking the study therapy. In some cases, side effects can be serious, longlasting, or may never go away. There is also a risk of death. You should talk to your study doctor about any side effects that you have while taking part in the study. Risks and side effects related to oxaliplatin include those which are: Likely These side effects occur in 25% or more of patients receiving oxaliplatin: Nerve problems that are usually temporary, but some may be longlasting. These may be made worse by exposure to cold temperature and cold objects Pain, tingling, burning, or numb feeling (pins and needles) in hands, feet, or area around mouth or throat, which may cause problems walking or performing the activities of daily living. Trouble swallowing or saying words, jaw tightness, odd feelings in the tongue, chest pressure, or a feeling of not being able to swallow or breathe without having any physical reason for this. Abdominal pain or cramps Temporary loss of hair Nausea Vomiting Diarrhea Fatigue Sores in mouth, throat, and esophagus, (the tube that goes from the mouth to the stomach) Low platelet count (which may lead to increased bruising or bleeding) Lowered red blood cell count (may lead to tiredness, weakness and shortness of breath) Low white blood cell count (may lead to infection) Cough Time away from work Side effects that occur in 10-24% of patients receiving oxaliplatin. Changes in blood tests that may indicate liver injury Fever 6/27/06 Page 7 of 16 Loss of appetite Infection Participant Initials _____ IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form Less Likely These side effects occur in 3-9% of patients receiving oxaliplatin: Headache Blistering, peeling, redness, swelling, tingling, numbness, and/or pain of the palms of hands and bottoms of feet Rash Inflammation of the veins Allergic reaction (including itching, hives, skin rash, fever, chills, muscle stiffening, sinus congestion, or swelling) Intestinal blockage Bowel wall changes (that may require hospitalization) Irritation of the intestines GI ulcers and bleeding Problems with hearing Visual changes (including blindness that lasts less than a minute) Rapid heartbeat Irregular movements Constipation Taste changes Shortness of breath Pain in muscles, bones, or joints Changes (high or low) in blood pressure Hot flashes/flushing Dehydration Fever with a low white blood cell count Chest pain Dizziness Mood changes (including depression) Blood clots Changes in blood test that may indicate kidney damage Hiccups Weight loss Eye problems (including redness and irritation) Poor coordination and balance Difficulty sleeping Rare, but Serious These side effects occur in less than 3% of patients receiving oxaliplatin: Changes in the lungs (including inflammation, thickening, scarring, and possible lung failure) A breakdown of red blood cells and kidney failure known as hemolytic uremic syndrome Severe allergic reaction including shortness of breath, low blood pressure, wheezing, chest tightness, and severe breathing problems 6/27/06 Page 8 of 16 Liver damage that may be permanent, including a serious form called “venoocclusive disease” which can cause swelling of the abdomen, painful swelling of the liver and yellowing of the skin Skin and tissue damage in the area surrounding the catheter where the chemotherapy is injected Irregular heartbeat Clots that form in the blood and use up the substances needed to stop bleeding Participant Initials _____ IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form Risks and side effects related to capecitabine include those which are: Likely These side effects occur in 25% or more of patients taking capecitabine: Diarrhea (can be very severe and lifethreatening) Nausea Vomiting Loss of appetite Sores in mouth, throat, and esophagus (these may cause difficulty in swallowing and/or heartburn) Redness, swelling, pain, numbness, tingling, cracking, blistering, and peeling of the hands and feet (handfoot syndrome) Eye problems Tiredness Abdominal pain Skin problems (rash, itching, and dryness) Changes in liver function tests Time away from work Change in ability to perform activities of daily living Low white blood cell count (may lead to infection) These side effects occur in 10-24% of patients taking capecitabine: Fever Headache Swelling Mouth discomfort Pain including back pain Tingling in the arms and feet (peripheral neuropathy) Constipation Eye irritation Less Likely These side effects occur in 3-9% of patients taking capecitabine: Dehydration Weakness Dizziness Nail changes Cough Shortness of breath Depression Hair loss 6/27/06 Page 9 of 16 Decreases in hemoglobin (the part of the blood cells that carry oxygen) Fever with a low white blood cell count Skin discoloration Gastrointestinal bleeding Mood changes Taste changes Difficulty sleeping Participant Initials _____ IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form Rare, but Serious These side effects occur in less than 3% of patients taking capecitabine: Heart problems Chest pain Low platelet count that may lead to increased bruising or bleeding Infection Changes in blood pressure Blood clots Risk and side effects related to panitumumab include those which are: 7/28/06 Likely These side effects occur in 25% or more of patients receiving panitumumab: Skin Rash. One of the most common side effects to occur with panitumumab is a mild to moderate skin rash. Over 90% of all patients experience some skin rash during therapy with panitumumab. This rash commonly resembles acne. The rash often appears on the face and upper chest but can affect any area of the skin. Some patients have experienced itching or pain with the rash. You should avoid being in the sun for extended periods of time because sunlight can make the rash worse. It is recommended that you wear sunscreen as well as protective clothing and a hat when outdoors. If you develop a rash, your study doctor may decide to treat the rash with medications or may hold the panitumumab until the rash gets better. The rash usually goes away once the panitumumab is discontinued. Diarrhea Dry skin Itching Decreased amount of magnesium in the blood 7/28/06 ● 7/28/06 These side effects occur in 10-24% of patients receiving panitumumab: 7/28/06 7/28/06 ● ● Sores in the mouth, throat, and the esophagus which is the tube that goes from the mouth to the stomach Infection of the nail bed (fingers or toes) Fissures (small cracks or splitting) of the skin on the fingertips or toes Cough Shortness of breath 6/27/06 Page 10 of 16 Participant Initials _____ IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form 7/28/06 Less Likely These side effects that occur in 3-9% of patients receiving panitumumab: 7/28/06 ● 7/28/06 Eye problems (including increased tearing, redness, itchiness, dry eyes, and blurred vision) Swelling in hands or feet Rare, but Serious These side effects occur in less than 3% of patients receiving panitumumab: 7/28/06 7/28/06 7/28/06 Decreased amount of calcium in the blood Lung complications (known as pneumonitis or fibrosis) ● Abnormal collection of fluid in the space between the lung and the wall of the chest cavity (pleural effusion) ● Blood clots in the legs Blood clot that could travel to the lungs Stroke Heart attack Severe skin infection ● Allergic reaction (including itching, hives, fever, chills, flushing, wheezing, shortness of breath, irregular heartbeat, drop in blood pressure, sweating, and swelling around your mouth and eyes) Reaction during the infusion (such as fever, chills that can be severe, low blood pressure, wheezing, nausea, and rash and itching) Risks related to radiation therapy: Your radiation therapy doctor will explain the side effects that may result from your radiation therapy. The drugs given in this study may make these side effects more severe. 10/30/06 Risks related to fertility and pregnancy: The drugs in this study as well as the radiation therapy, can be harmful to an unborn baby. Therefore, women should not become pregnant and men should not father a baby while on this study. Both men and women must use a reliable method of birth control while participating in this study. Reliable methods of birth control are considered to be: abstinence (not having sex), oral contraceptives, Intrauterine Device (IUD), Norplant, tubal ligation, hysterectomy or vasectomy of the partner (with confirmed negative sperm counts) in a monogamous relationship (same partner). An acceptable, although less reliable method involves the careful use of condoms and spermicidal foam or gel and/or cervical cap or sponge. Both male and female patients should ask about counseling and more information about preventing pregnancy. Female patients who feel they might be pregnant, even though they practiced birth control, must notify the study doctor immediately. A pregnancy test may be performed. 6/27/06 Page 11 of 16 Participant Initials _____ IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form Male patients should also inform the study doctor immediately if their sexual partners become pregnant while the patient is receiving treatment. Pregnant women and nursing mothers are excluded from participation in this study. If a woman becomes pregnant, she will be withdrawn from the study. If a man fathers a child, there may be potential risk to the unborn baby; therefore, female sexual partners of men on treatment should use an adequate form of birth control. Men and women should continue to take contraceptive precautions for at least 6 months after their last dose of panitumumab. Women should not breastfeed a baby while on this study and for at least 6 months after the last dose of panitumumab. Since most methods of birth control are not 100% reliable, if you are a sexually active woman of childbearing potential, a blood pregnancy test within 7 days of study entry is required. Secondary Malignancies: A number of established chemotherapeutic drugs have an inherent (basic) risk of causing secondary cancers and/or leukemias (cancer of the white blood cells). Certain drugs in use today, not currently known to be associated with this risk, may be shown at a later time to result in the development of these secondary cancers and/or leukemias, which may not be reversible. For more information about risks and side effects, ask your study doctor. Are there benefits to taking part in the study? Taking part in this study may or may not make your health better. While doctors hope these drugs will be effective in treating rectal cancer, there is no proof of this yet. We do know that the information from this study will help doctors learn more about these drugs as a treatment for cancer. This information could help future cancer patients. What other choices do I have if I do not take part in this study? Your other choices may include: Getting treatment or care for your cancer without being in a study Taking part in another study Getting no treatment Talk to your doctor about your choices before you decide if you will take part in this study. 10/30/06 Will my medical information be kept private? We will do our best to make sure that the personal information in your medical record will be kept private. However, we cannot guarantee total privacy. Your personal information may be given out if required by law. If information from this study is published or presented at scientific meetings, your name and other personal information will not be used. 6/27/06 Page 12 of 16 Participant Initials _____ IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form A record of your progress will be kept in a confidential form at your hospital or doctor’s office where you receive treatment. Organizations that may inspect and/or copy your research and medical records (blood samples, x-rays, scans, pathology slides, etc.) for quality assurance, research, and data analysis include groups such as: Southeast Cancer Control Consortium (SCCC) Operations Office The National Surgical Adjuvant Breast and Bowel Project (NSABP) Foundation Research Program (FRP) Amgen, Inc., which is the company supplying the study drug panitumumab for the study International Drug Development Institute (IDDI), which is the company that will analyze the data for this study Food and Drug Administration (FDA) Office for Human Research Protections (OHRP) Institutional Review Board (IRB) at your hospital Possible other federal or state government agencies If your record is used or given out for governmental purposes, it will be done under conditions that will protect your privacy to the fullest extent possible consistent with laws relating to public disclosure of information and law-enforcement responsibilities of the agency. These agencies may review the research to see that it is being done safely and correctly. You authorize the use of clinical information contained in your records, but any publication which includes such information or data shall not reveal your name, show your picture or contain any other personally identifying information, except as otherwise required by law. What are the costs of taking part in this study? You and/or your health plan/insurance provider (Medicare should be considered a health insurance provider) will need to pay for some or all of the costs of treating your cancer in this study. Some health plans will not pay these costs for people taking part in studies. Check with your health plan or insurance company to find out what they will pay for. Taking part in this study may or may not cost your insurance company more than the cost of getting regular cancer treatment. You or your insurance carrier will be responsible for the costs of clinic visits, any hospital admissions, laboratory tests, xrays, scans, chemotherapy treatments, radiation treatments, and any other tests. Please ask your doctor about any added costs or insurance problems. Tests, procedures, or drugs for which there is no charge in this study: 6/27/06 Page 13 of 16 Participant Initials _____ IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form Blood tests to measure the amount of calcium, potassium, and magnesium in the blood. These blood tests will be done before you join the study and at the scheduled time points described earlier in this consent form. PET scan performed after your study therapy is done. Panitumumab will be provided for this study at no cost to you by Amgen, Inc. However, you or your insurance company will need to pay for costs of the supplies and personnel who give you the drug. If, during the study, panitumumab is approved for use in rectal cancer, you and/or your health plan may have to pay for drug needed to complete this study. Oxaliplatin and capecitabine are available commercially, and you or your insurance company will be responsible for their costs. You or your insurance company will also need to pay for costs of the supplies and personnel who give you the drugs. The radiation therapy you receive in this study is considered the standard treatment for patients with your stage of rectal cancer. Therefore, you and/or your insurance company will be responsible for the costs of the radiation therapy. You will not be paid for taking part in this study. For more information on clinical trials and insurance coverage, you can visit the National Cancer Institute’s Web site at http://cancer.gov/clinicaltrials/understanding/insurancecoverage. You can print a copy of the “Clinical Trials and Insurance Coverage” information from this Web site. Another way to get the information is to call 1-800-4-CANCER (1-800-422-6237) and ask them to send you a free copy. What happens if I am injured because I took part in this study? It is important that you tell your study doctor, _________________________ if you feel that you have been injured because of taking part in this study. You can tell the doctor in person or call him/her at #____________________________. You will get medical treatment if you are injured as a result of taking part in this study. You and/or your health plan will be charged for this treatment. The study will not pay for medical treatment. Although no funds or monies have been set aside to compensate you in the event of injury or illness related to the study treatment or procedures, you do not waive any of your legal rights for compensation by signing this form. You or your insurance company will be charged for continuing medical care and/or hospitalization. 6/27/06 Page 14 of 16 Participant Initials _____ IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form What are my rights if I take part in this study? Taking part in this study is voluntary. You may choose to take part, not to take part, or may leave the study at any time. No matter what decision you make, there will be no penalty to you and you will not lose any of your regular benefits. Leaving the study will not affect your medical care or result in any penalty or loss of benefits to which you are entitled. Even after you agree to take part in this study, you may withdraw at any time. Before you withdraw, you should talk to one of the researchers or nurses involved. This will allow them to inform you of any medical problems that could result from stopping your treatment. You can choose to withdraw one of two ways. In the first, you can stop your study treatment, but still allow the study doctor to follow your care. In the second, you can stop your study treatment and not have any further contact with the study staff. Either way, there will be no penalty to you. Your decision will not affect your medical treatment or your relationship with those treating you or with this institution. If you withdraw from the study, you will still be offered all available care that suits your needs and medical condition. You are free to seek care from a doctor of your choice at any time. We will tell you about new information that may affect your health, welfare or willingness to stay in this study. You may be asked to sign another consent form in response to new information. 10/30/06 Who can answer my questions about the study? For questions about the study or a research-related injury, contact your doctor, _________________, at # _____________________. You may ask your doctor for further information on the risks, benefits or alternative treatments. For questions about your rights as a research participant, contact the ___________________ Institutional Review Board (which is a group of people at the hospital in the community where you receive treatment who review the research to protect your rights) at # ____________________ (the office of __________________________). Participant Contract I have been offered the opportunity to ask questions about this study and all questions have been answered to my satisfaction. The contents of this form have been explained to me and I understand them. I agree to allow the research personnel specified above the access to my medical records. 6/27/06 Page 15 of 16 Participant Initials _____ IRB Approval Date: ______________ Version Date: 7/28/06; Amendment #1 Updated 10/30/06 Appendix I NSABP FR-1 Southeast Cancer Control Consortium Consent Form It may be necessary for my doctor to contact me at a future date regarding new information about the treatment I received; therefore I agree to notify my doctor of any change of address and/or telephone number. My signature below means that I have voluntarily agreed to participate in this research study. I will be given a copy of all 16 pages of this consent. I may also request a copy of the study (complete study plan). ______________ (Date) _________________________________ (Participant Signature) I certify that I have explained to the above individual the nature and purpose, the potential benefits, and possible risks associated with participation in the research study and have answered any questions that have been raised. ______________ (Date) 6/27/06 _________________________________ (Signature of Person Obtaining Consent) Page 16 of 16 NSABP FR-1 Southeast Cancer Control Consortium Withdrawal of Consent I, _____________________________, withdraw my consent to participate in this study and refuse to be followed and have clinical data collected from my medical records. Participant Name ___________________________________ Study/ID #___________ (Please Print Name) Participant Signature ____________________________________ Date ___________ Witness Signature ______________________________________ Date ___________ 6/27/06 NSABP FR-1 Southeast Cancer Control Consortium Withdrawal of Treatment Consent I, _____________________________, withdraw my consent for treatment on this study. Even though I withdraw my consent for treatment, I will continue to be followed and clinical data will be collected from my medical records. Participant Name ___________________________________Study/ID #____________ (Please Print Name) Participant Signature ____________________________________ Date __________ Witness Signature ______________________________________ Date __________ 6/27/06