Vaccine/Screening
advertisement

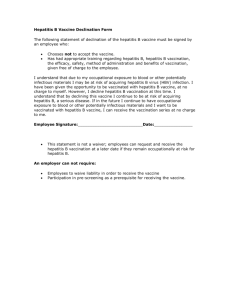
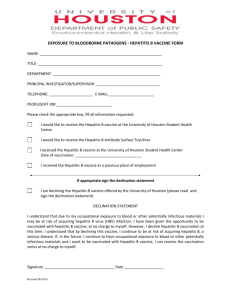
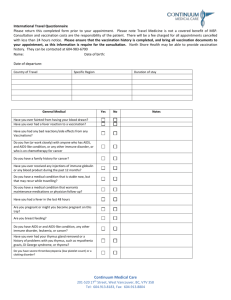
The University of Sydney CONCORD CLINICAL SCHOOL MEDICAL STUDENT DECLARATION PLEASE READ WEBSITE AND COMPLETE THIS FORM and return it with the other required documentation. It is NSW Government Law that medical students and health care workers are required to comply with the NSW Health Department Circular Occupational Screening and Vaccination Against Infectious Diseases (Circular 2003-91). This document can be viewed on the NSW Health Web site: http://www.health.nsw.gov.au/archive/cib/circulars/2003/cir2003-91.pdf or read the information on the following pages and if you are fully immunised please sign this form and return it with the other mandatory documentation. DECLARATION I (PRINT name): Address: Post Code: Date of Birth: I am aware that I am required to comply with the NSW Health Department Circular “Occupational Screening and Vaccination Against Infectious Diseases (Cir. 2003/91).” (Medical students in this document are regarded as “Other personnel”, in “Risk Category A”). Signed: Date: While you are not required to send any other vaccination/screening documentation before your elective, you must bring proof of vaccinations/screenings with you for the period of your elective. Vaccine/Screening Medical Students are Category A – direct patient contact or contact with blood and body substances. All employees and “other personnel” who have physical contact with, or potential exposure, to blood or body substances. Table 1. Summary of Screening and Vaccination Policy (Key: Y = yes, N = no, S = selected employees and "other personnel") Vaccine/Screening Adult Diphtheria and Tetanus OR Adult Diphtheria, Tetanus & Pertussis (cellular) Hepatitis A Hepatitis B Influenza Measles/Mumps/Rubella Varicella (chickenpox) 5 Tuberculosis A Y Y Y Y Y Y Y Y ADDITIONAL NOTES (Please also refer to the current edition of the National Health and Medical Research Council Australian Immunisation Handbook) 1 . Pertussis (Whooping Cough) Employees and "other personnel", who work in close contact with young infants, should receive one dose of an adult pertussis containing vaccine (instead of adult diphtheria and tetanus vaccine), unless they have received a diphtheria/tetanus vaccine within the previous five years. 2. Hepatitis A • Vaccination should be considered for category A employees and "other personnel" who work in rural and remote Aboriginal communities or who work in paediatric wards, intensive care units or emergency departments, which provide for substantial populations of Aboriginal children. Vaccination should also be considered for childcare workers, carers of the intellectually disabled and for employees and "other personnel" in category D, such as plumbers, who may be exposed to sewage at work. To avoid unnecessary vaccination, those born before 1950, those who spent their early childhood n Aboriginal communities, and those with previous unexplained hepatitis or jaundice, should be serologically screened. 3. Hepatitis B • Employees and "other personnel" should be considered immune if they have documented post-accination serology demonstrating adequate anti-HBs antibodies (>1 0 m1UlmL) or serological evidence of past infection. Pre-vaccination serology is not routinely required for unimmunised employees or "other personnel". Post-vaccination serology is required to confirm immunity following vaccination. If post-vacci nation serology does not demonstrate adequate anti-HBs antibodies, the employee and "other personnel" should be offered serological screening for hepatitis B surface antigen carriage. Those who are hepatitis B surface antigen negative should be offered a double dose of vaccine or a further course of 3 doses at monthly intervals with testing four weeks after each additional dose. Persistent non-responders must be advised of post-exposure precautions, as specified in NSW Health Circular 2003139 (Management of Health Care Workers Potentially Exposed to HIV, Hepatitis B and Hepatitis C). Booster doses are not required following achievement of serologically confirmed immunity and antibody levels do not require repeated monitoring. Employees and "other personnel" who perform exposure prone procedures (EPPs) as part of their employment must provide documented evidence of their hepatitis B immune status. Employees and "other personnel" who fail to provide documented evidence of their hepatitis B immune status, must not perform EPPs. Non-immune employees and "other personnel" must be counselled regarding risk and acknowledge this advice in writing. Non-immune employees and "other personnel", who perform EPPs, must undertake annual hepatitis B screening at their own cost. Employees and "other personnel" who are HBeAg and/or HBV DNA positive must not perform EPPs, as prescribed by NSW Health Circular 99188 (Health Care Workers Infected with HIV, Hepatitis B or Hepatitis C). 4. Measles/Mumps/Rubelia (MMR) Employees and "other personnel" (both male and female) should be considered immune to measles, mumps and rubella, if they can provide documented evidence of having received two doses of MMR vaccine or can provide serological evidence of immunity to measles, mumps and rubella. 5. Varicelia (Chicken Pox) • • • Employees and "other personnel" with a negative or uncertain history of varicella should be serologically screened and, if negative, vaccinated with two doses of vaccine, one to two months apart. Serological testing following vaccination is not required. Non-immune employees and "other personnel " must not care for patients with chicken pox or shingles Rarely a rash may develop following vaccination. Employees and "other personnel", who develop a rash during the six weeks following vaccination, should report it immediately and be reassigned to duties that require no patient contact, or placed on sick leave or a form of special leave for the duration of the rash. Employees must be advised of their right to submit a workers' compensation claim. 6. Tuberculosis • • • Tuberculosis screening, education and vaccination should be provided to employees and “other personnel" in accordance with NSW Health Circular 2001171 (Health Care Worker Tuberculosis Screening and Protection Policy). In low tuberculosis incidence countries such as Australia, employees and "other personnel" at risk of infection should be monitored for evidence of infection with periodic tuberculin skin tests (TSTs). Employees and "other personnel", who refuse to be monitored by TSTs should be offered BCG vaccination together with written information about the vaccine's efficacy, advantages and disadvantages. Non-participation must be documented in writing. Recommended frequency of TSTs varies according to risk of exposure to tuberculosis in the work setting and reference should be made to NSW Health Circular 2001171 (Health Care Worker Tuberculosis Screening and Protection Policy). 7. Hepatitis C (HCV) and Human Immunodeficiency Virus (HIV) All employees and "other personnel" who perform EPPs are required to be aware of their HCV and HIV status and must not perform EPPs if they are HCV polymerase chain reaction positive or H IV antibody positive, in accordance with NSW Health Circular 99188 (Health Care Workers Infected with HIV, Hepatitis B or Hepatitis C).