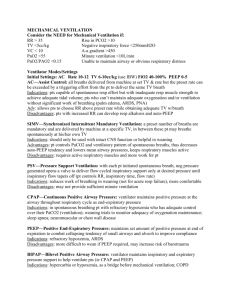
Educational Assignment Week 1: Mechanical Ventilation
advertisement
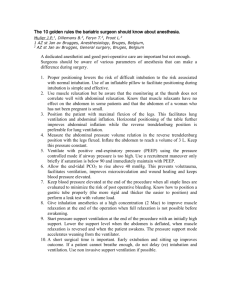
Educational Assignment Week 2: Airway Management and Mechanical Ventilation Weaning Didactics: SCCM’s AICU Online Course Series: Airway Management ACCP’s Critical Care Board Review Series: Weaning From Mechanical Ventilation Reading Assignment: Adult Multiprofessional Critical Care Review Principles of Weaning and Withdrawing Mechanical Ventilatory Support pg. 205 ACCP Review: Weaning From Mechanical Ventilation by Stoller Evidence-Based Guidelines for Weaning and Discontinuing Ventilatory Support. Chest: 2001. Clinical review: Liberation from mechanical ventilation. Crit Care: 2008. Clinical review: Management of difficult airways. Crit Care: 2006. Pre-Review Questions: SEP-2A-10 1. A 74-year-old man who has had congestive heart failure and chronic obstructive pulmonary disease is admitted to the intensive care unit because of increasing confusion. On physical examination, respirations are 35 per minute, and blood pressure is 70/40 mm Hg. Examination of the chest reveals crackles extending about one third of the way up both lung fields. Arterial blood studies (with the patient breathing 40% oxygen by face mask) show PO2 is 50 mm Hg, PCO2 is 58 mm Hg, and pH is 7.01. Electrocardiogram reveals atrial fibrillation with a ventricular rate of 135 beats/min. Which of the following should you do next? (A) Start noninvasive positive pressure ventilation by face mask (B) Insert a pulmonary artery catheter with the patient in a semirecumbent position (C) Administer one ampule of sodium bicarbonate (D) Begin furosemide, intravenously (E) Intubate the patient SEP-2A-19 2. When you look at chest radiographs to compare the position of your patient's endotracheal tube today with its position yesterday, you note that the tip of the tube is now slightly closer to his carina. Which of the following is most likely to have caused this change? (A) Large inspirations (B) Prone position (C) Neck extension (D) Neck flexion SEP-2A-20 3. A 28-year-old man who was extremely short of breath was transferred from the emergency department to the intensive care unit. The patient smoked one pack of cigarettes daily for the past 15 years. For the past five years he has had asthma, which has been treated with inhaled beta-agonists and inhaled corticosteroids. Recently the patient stopped using his inhalers. On examination, his blood pressure was 128/78 mm Hg with a 32 mm Hg pulsus paradoxus. He used his accessory muscles for breathing, and auscultation revealed little air movement. After treatment with a nebulized beta-agonist, the patient was breathing 2 L/min of oxygen by nasal cannula; arterial blood studies showed PO2 was 68 mm Hg, PCO2 was 63 mm Hg, and pH was 7.27. You applied a topical anesthetic to the upper airway and nasal mucosa and cautiously performed a nasal endotracheal intubation without sedating the patient. The patient was frightened but cooperative, and intubation was successful. He was then sedated with midazolam and morphine. The respiratory therapist manually ventilated the patient, and a chest radiograph was performed. Now, several minutes later, the therapist comments that ventilation is becoming extremely difficult to perform and the patient, who appears pale, is unresponsive and has a blood pressure of 76/40 mm Hg by manual cuff measurement. The chest radiograph reveals that the endotracheal tube is well positioned in the mid trachea. Which of the following should you now do? (A) Decrease the rate of positive pressure breaths and recheck the blood pressure (B) Connect the patient to a volume-cycled ventilator (C) Begin norepinephrine (D) Begin continuous nebulization of a beta-agonist (E) Perform a blind needle thoracostomy SEP-2B-12 4. A 28-year-old man is admitted to the intensive care unit after sustaining burns from a propane tank explosion. Over 60% of his body surface area is burned. Twenty-four hours after admission to the unit, the patient has respiratory failure and requires intubation and mechanical ventilation. Life-threatening complications are most likely to develop with the use of which of the following? (A) Cisatracurium (B) Pancuronium (C) Rocuronium (D) Succinylcholine (E) Vecuronium