RSPT 2353 – Neonatal/Pediatric Respiratory Care
advertisement
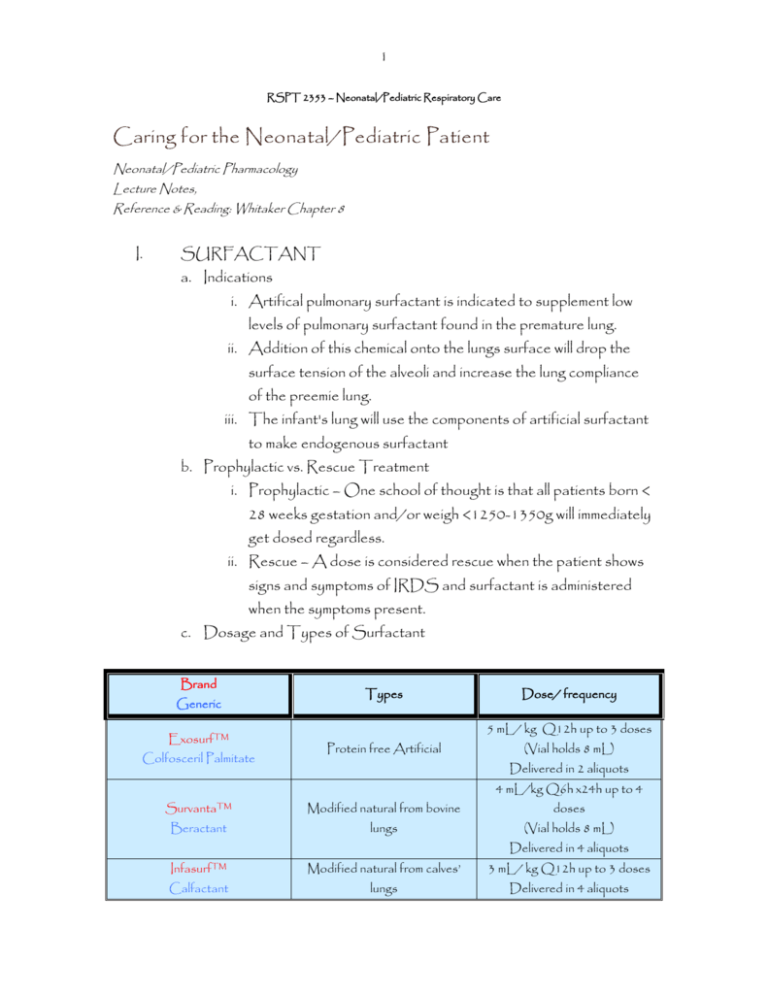
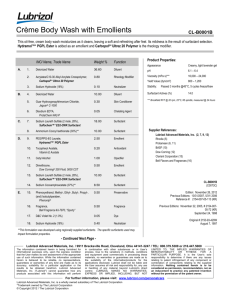
1 RSPT 2353 – Neonatal/Pediatric Respiratory Care Caring for the Neonatal/Pediatric Patient Neonatal/Pediatric Pharmacology Lecture Notes, Reference & Reading: Whitaker Chapter 8 I. SURFACTANT a. Indications i. Artifical pulmonary surfactant is indicated to supplement low levels of pulmonary surfactant found in the premature lung. ii. Addition of this chemical onto the lungs surface will drop the surface tension of the alveoli and increase the lung compliance of the preemie lung. iii. The infant's lung will use the components of artificial surfactant to make endogenous surfactant b. Prophylactic vs. Rescue Treatment i. Prophylactic – One school of thought is that all patients born < 28 weeks gestation and/or weigh <1250-1350g will immediately get dosed regardless. ii. Rescue – A dose is considered rescue when the patient shows signs and symptoms of IRDS and surfactant is administered when the symptoms present. c. Dosage and Types of Surfactant Brand Generic Exosurf™ Colfosceril Palmitate Types Dose/ frequency 5 mL/ kg Q12h up to 3 doses Protein free Artificial (Vial holds 8 mL) Delivered in 2 aliquots 4 mL/kg Q6h x24h up to 4 Survanta™ Modified natural from bovine doses Beractant lungs (Vial holds 8 mL) Delivered in 4 aliquots Infasurf™ Modified natural from calves’ 3 mL/ kg Q12h up to 3 doses Calfactant lungs Delivered in 4 aliquots 2 d. Generic Protocol – most institutions have a procedure to administering surfactant. i. Warm surfactant at room temperature for 20 minutes or warm in hand for 8 minutes. ii. Verify ETT placement by x-ray. iii. Note baseline parameters of ventilator settings, HR, SpO2, chest excursion, MAP (if applicable). iv. Change ventilator settings: rate to 40 bpm, Ti to 0.4 sec (ensures equal distribution) PIP, PEEP, and FiO2 remain the same. v. Patient should be supine. After each aliquot pt is placed in four positions as follows for 30 seconds: 1. head down, body turn to left (R side up) 2. head down , body turn to right (L side up) 3. head up, body turn to left (R side up) 4. head up, body turn to right (L side up) vi. Assess pt after each aliquot is administered and adjust as needed: 1. Decreased SpO2 Increase FiO2 2. Decreased chest excursion 3. Bradycardia Increase PIP Increase PIP 4. In only refractory situations should a practitioner hand bag a patient. vii. After administration monitor, for 10 minutes, return to original ventilator settings. *Note: If the patient can not tolerate his original settings, notify MD. II. PENTAMADINE (NebuPent®, Pentam-300®) a. Indications: Treatment and prevention of Pneumosystic Carinii Pneumonia (PCP ) who can not tolerate co-trimoxazole or fail to respond to this drug. Usually AIDS patients, or immunocompromised patients (cancers, esp. leukemia 3 b. Dosage: i. Inhalation - Prophylaxis 1. < 5years: 8 mg/kg not to exceed 300 mg 2. > 5 years 300 mg/dose q 3 weeks or monthly 3. Adults 300 mg q month or 140 mg q 2 weeks. ii. Inhalation – treatment 1. 600 mg/6 mL NS qday for 14-21 days. iii. Administer via Respigard II, with minimal people in room. Nose plugs if necessary. iv. All persons in room must wear N95 HEPA mask. c. Side Effects i. Most common is bronchospasm – prophylactically a bronchodilator is administered before and after tx. If occurs during tx, stop and administer bronchodilator. ii. Throat irritation – give a drink during or after tx as necessary iii. Nausea – Stop therapy, assess, resume if tolerated. III. PULMOZYME (Dornase Alfa) a. Indications: Management of CF to reduce frequency of respiratory infections and improve pulmonary function, a maintenance mucolytic b. An DNA enzyme produced by recombinant gene technology, derived from Chinese hamster ovary cell products (epoetin alfa) c. Dosage: 2.5 mL in 3mL NS. Qday or BID. d. This drug is not to be mixed with other drugs, and is to be administered via Pari LC neb. e. Side effects: i. Excessive coughing – stop and reassess ii. Induced bronchospasm – stop, administer bronchodilator if indicated. iii. Throat irritation – give drink after therapy. 4 IV. TOBRAMYCIN (TOBI ®) a. Indication: Inhalations therapy for the management of CF patients with P. aeruginosa infections b. Dosage: i. Low dose 40 – 160 mg BID ii. Prophylaxis in CF: 300 mg BID for 28 days on, 28 days off c. To be administered via Pari LC nebulizer. If on pulmozyme the patient must have and nebulizer for EACH drug. d. TOBI ® can sometimes be coordinated with Tobramycin IV, the RT must coordinate with the RN to ensure an accurate trough. e. Side effects i. Induced bronchospasm: stop tx, administer bronchodilator, if necessary. ii. Excessive coughing/hemoptysis – stop tx, notify RN and MD iii. Dyspnea – stop tx, administer O2 as needed. iv. Hyperventilation – Stop tx, allow pt to recover, resume if tolerated. v. Toxicity: Ototoxicity (ringing in ears) – notify RN and MD, Nephrotoxicity – notify MD if symptoms of renal failure occur. f. Other antibiotics that can be inhaled include: Gentamycin, Colistin, amikacin, and Amphotericin B.








![[Product Name] - proteabio.com](http://s3.studylib.net/store/data/007857579_2-ad13906ad6791e5042b2e55b2c293741-300x300.png)