Atelectasis of the lung, acute lung injury, vascular diseases
advertisement
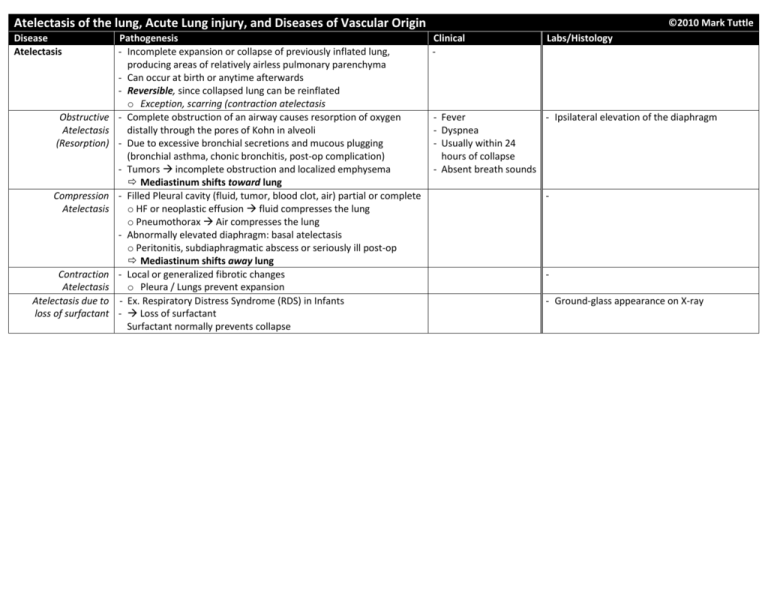
Atelectasis of the lung, Acute Lung injury, and Diseases of Vascular Origin Disease Atelectasis Obstructive Atelectasis (Resorption) Compression Atelectasis Contraction Atelectasis Atelectasis due to loss of surfactant Pathogenesis - Incomplete expansion or collapse of previously inflated lung, producing areas of relatively airless pulmonary parenchyma - Can occur at birth or anytime afterwards - Reversible, since collapsed lung can be reinflated o Exception, scarring (contraction atelectasis - Complete obstruction of an airway causes resorption of oxygen distally through the pores of Kohn in alveoli - Due to excessive bronchial secretions and mucous plugging (bronchial asthma, chonic bronchitis, post-op complication) - Tumors incomplete obstruction and localized emphysema Mediastinum shifts toward lung - Filled Pleural cavity (fluid, tumor, blood clot, air) partial or complete o HF or neoplastic effusion fluid compresses the lung o Pneumothorax Air compresses the lung - Abnormally elevated diaphragm: basal atelectasis o Peritonitis, subdiaphragmatic abscess or seriously ill post-op Mediastinum shifts away lung - Local or generalized fibrotic changes o Pleura / Lungs prevent expansion - Ex. Respiratory Distress Syndrome (RDS) in Infants - Loss of surfactant Surfactant normally prevents collapse ©2010 Mark Tuttle Clinical - Labs/Histology - Fever - Ipsilateral elevation of the diaphragm - Dyspnea - Usually within 24 hours of collapse - Absent breath sounds - - Ground-glass appearance on X-ray Acute Lung Injury: Pulmonary Edema • Pulmonary congestion + edema • Adult Respiratory Distress Syndrome (Diffuse alveolar damage b/c can be children too) 1. Hemodynamic edema(transudate) 2. Edema from Microvascular Injury (exudate) - Hydrostatic pressure ↑ - Infections: pneumonia, septicemia - Heavy, wet lungs, o Left sided HF (common) - Inhaled gases: oxygen, smoke frothy blood tinged o Volume Overload - Aspiration: gastric contents, near-drowning fluid o Pulmonary vein obstruction - Drugs/chemicals: chemotherapeutic agents - Fluid accumulates - Oncotic pressure ↓ (less common) o Bleomycin: edema & fibrosis Short term Long-term in the lower lobes o Hypoalbuminemia o Amphotericin B Microscopic changes where hydrostatic o Nephrotic syndrome o Heroi - Intraalveolar granular eosinophilic precipitate pressure is greater o Liver disease o Kerosine - Alveolar microhemorrhages and hemosiderin- Changes lead to o Protein-losing enteropathies o Paraquat (herbicide) laden macrophages (“heart-failure cells”) present impaired function - Lymphatic Obstruction - Shock in chronic cases (interstitial edema) - Trauma - With long-standing chronic passive congestion and predisposes - Transfusion-related (TRALI) (e.g. mitral stenosis – fish mouth from RF), lungs one to infections 3. Edema of undetermined origin become visibly brown. firm (hemosiderin-laden (intraalveolar - High Altitude (HAPE) – High altitude pulmonary edema macrophages and interstitial fibrosis) edema) - Neurogenic (CNS trauma) termed “brown induration” Adult Respiratory Infection Chemical Injury - Rapid onset of: Acute Stage Distress Syndrome Sepsis (40% cases) Heroin or methadone o Severe life-threatening respiratory insuffic. - Increased capillary permeability produces (ARDS, Diffuse Diffuse pulmonary Acetyaslicyclic acid o Cyanosis interstitial and then intra-alveolar edema Alveolar Damage infections Barbituate overdose o Severe arterial hypoxemia refractory to - Interstitial inflammation DAD) Gastric aspiration Paraquat (herbicide) oxygen therapy - Hyaline membranes composed of fibrin rich (30% cases) o “White out” on X-ray - bilateral fluid, cytoplasmic and lipid remnants of Noncardiogenic Inhaled Irritants - Severe pulmonary edema necrotic epithelial cells pulmonary edema Physical Injury Oxygen toxicity - Frequently progresses to multisystem failure Organizing stage resulting from acute Mechanical Smoke Pathogenesis - Resolution is unusual. Instead, the fibrin alveolar-capillary trauma(head ) Irritant gases and - Diffuse damage to alveolar capillary walls exudate organizes damage (20% cases) chemicals - Most common: alveolar capillary endothelium - Hyperplasia of type II pneumocyte continues Pulmonary - Less common: injury to alveolar epithelium – attempt at repair and resolution Clinical Course contusions Hematologic - Increased vascular permeability ↑ - Interstitial inflammation and fibrosis - 150,000 cases/year Near-drowning Multiple transfusions Alveolar flooding, rich in fibrin, deposit in wall - Intra-alveolar fibrosis in USA Fractures with fat DIC - Analogous to crescenteric glomerulonephritis - Honeycomb lung - 60% mortality embolism - Loss of diffusion capacity Superimposed bacterial infx: in fatal cases - Severe dyspnea + Burns Pancreatitis - Widespread surfactant abnormalities due to Diffuse Alveolar Damage (DAD) tachypnea Ionizing radiation damage of Type II Pneumocytes Atelectasis Hyaline membrane - O2 transport dmgd - Hypoxemia Uremia - Resolve in 1st week unresponsive to O2 Hypersensitivity - If survive > 1week, therapy Organic solvents Cardiopulm bypass Honeycomb inflammation + fibros - PaO2 < 50mmHg Drugs Lung compliance ↓ - Respiratory therapy V/Q mismatch - Need high O2 to treat but O2 toxicity Diseases of Vascular Origin: Pulmonary embolisum, hemorrhage, infarction. Pulmonary HTN, vascular sclerosis, Diffuse pulmonary hemorrhage (Goodpasture, idopath) Disease Pathogenesis Clinical Labs/Histology Pulmonary Embolism - Blood clot that occlude the large None (~60-80% are clinically silent) Embolus: pulmonary arteries - Too small of emboli - Red cells, platelets and fibrin fill arterial Large - Source: DVT in legs (most common) Hemorrhage (~10-15%) lumen adhering to endothelial surface - Chest pain - Predisposing factors: - Tissue viability sustained by collateral blood flow - May dissolve or organize and recanalize - Dyspnea o Immobilization (ex. hospital, flight) - Transient chest pain & cough Hemorrhage: - Shock o Hypercoagulable States Infarction (10%) – less likely b/c collateral circul. - Blood in alveoli and interstitium - Fever (Factor V bleeder, Contraception – - Due to inadequate collateral blood flow; often - Preserved architecture - Elevated enzyme, estrogen, Malignancy [Trousseau’s]) coexisting heart and lung disease is present Infarct: Acute R-HF (cor pulm.), CV collapse sudden death - Usually wedge-shaped and peripheral, with LDH3 ↑ Treatment - Due to obstruction of pulmonary vasculature embolus at apex mimic MI - Difficult problem: prophylaxis - Patients have electromechanical dissociation - Apex points to hilum - Early post-surgical ambulation Pulmonary hypertension - ¾ infarcts in lower lobe Small - Elastic stockings, leg exercises - Multiple emboli over time; can cause chronic Acute (recent) infarct - Transient chest Anticoagulation for high-risk ppl right heart strain (right ventricular hypertrophy) - Coagulative necrosis with hemorrhage pain or cough- Filter in inferior vena cava Second embolus (30%) (ie. red infarct) normal CVS - Overlying pleura with fibrinous pleuritis - Dyspnea - Post-morten clot: free, unattached Seen in most cases Remote (old) infarct - Tachypnea - Pre-morten clot: lines of Zahn, on vessel - Wheezing from THXA2 from platelets - Inflammatory response followed by - Chest pain - Fever regeneration and fibrosis (scar) - Cough, hemoptysis - Pleural friction rub - Often hemosiderin in macrophagesHF cells – infarcts with Special types of Emboli compromised Pulmonary Infarct Fat embolism: Air embolism: bronchial - Multiple in > 50% - Most common form of clinically - Trauma, surgery, intravenous injections, circulation - Lower lobes: 2/3 significant embolism second to obstetrical procedures, criminal abortion - Wedge shaped thromboembolism May cause sudden death frothy blood is Diagnosis - Base peripheral - Occurs generally as a result of fracture present in the right ventricle and pulmonary - Spiral CT - Apex toward hilum of a long bone, most typically the femur artery at autopsy angiography - Histological examination shows fat - On histological examination, empty spaces - Most definitive globules in the capillaries and small resembling fat emboli are seen technique, but Saddle Embolus vessels of the lung Embolic carcinomatosis: dangerous for the Septic embolism: - Carcinomas (breast, stomach and lung) invade patient - Infected fragments of venous thrombi or blood vessels, disseminate and occlude - D-dimer level tricuspid valve vegetations (endocarditis) pulmonary arteries - “Septic infarct” (neutrophils and Amniotic fluid embolism: organisms) can convert to abscess - Usually at time of delivery; can cause shock and Bone marrow embolism: diffuse alveolar damage in severe cases - CPR with chest compressions leading to rib fractures Starch or talc particles: - Contained in drug injected by addicts Disease Pulmonary Hypertension When mean pulmonary pressure reaches ¼ systemic Pathogenesis - Primary (Idiopathic) – rare o Females: 24-40yrs; sometimes young o Dyspnea, fatigue (hypoxia), common o Some patients have angina o Right ventricular hypertrophy o 80% die 2-5 years of Cor Pulmonale o Often w/emboli, pneumonia - Secondary: Structural conditions which increase pulmonary blood flow, vascular resistance, or L heart resistance o Chronic obstructive, insterstitial lung diseases o Antecedent congenital or acquired heart disease (ex. TOF) o Recurrent thromboemboli o Autoimmune disorders Diffuse Pulmonary Hemorrhage Syndromes Goodpasture - Anti-Basement Membrane Antibodies Syndrome - Simultaneous renal, pulmonary disease - Proliferative rapidly progressive glomerulonephritis - Necrotizing hemorrhagic interstitial pneumonitis Idiopathic Pulmonary - Degeneration and hyperplasia of Hemosiderosis alveolar epithelial cells - Cause unknown Vasculitis-associated hemorrhage - Hypersensitivity angiitis - Wegener’s Granulomatosis - Lupus erythematosus (SLE) Clinical - Role of BMPR2 (Bone morphogenic prot) Surface protein family TGF-β Binds to cytokines o Embryogenesis o Cell proliferation & differentiation o Apoptosis - BMPR2 inhibition of proliferation - If mutated proliferation of sm. mm. o 50% of familial 1° pulmonary HTN o 26% of sporadic cases o 2q33 locus association Morphology Atheromatous plaques - Main elastic arteries Medial hypertrophy, intimal proliferation, fibrosis - Small arteries and arterioles Plexogenic pulmonary arteriopathy - Capillary tuft formation (“plexiform lesion”) - Indicates severe and irreversible hypertension - Males > Females; most cases in teens, 20s - Patients generally present with hemoptysis, focal lung consolidations and renal failure. - Uremia common cause of death - Trigger, initiating antibody is unknown. - Viruses, smoking and exposure to hydrocarbons (dry cleaning industry) may be cofactors - Treatment – immunosuppressants and plasmapheresis - Cough, hemoptysis, anemia, weight loss - Children and young adults - Labs/Histology Mainly arterioles, small arteries Medial thickness, intimal fibrosis, narrow lumen - Immunofluorescence shows linear deposits of immunoglobulins and complement on the glomerular BM and in the alveolar septa - Hemosiderin filled macrophages in alveoli and hemosiderin in alveolar septa o DDx from HF cells HF cells not in septa - Capillary dilatation and pulmonary fibrosis -








