Newsletter - Hartley Corner Surgery
advertisement
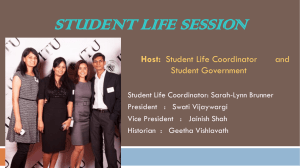
HARTLEY CORNER SURGERY PATIENT PARTICIPATION GROUP NEWSLETTER No.5 ~ July 2012 Committee Members: Chairperson: Anne Strong (email: amstrong@sky.com) Secretary: Karen Toms (Practice Manager - contact through Hartley Corner Surgery), Hugh Lambert & Gill Lambert (Treasurer) (email: mimi.lambert@ntlworld.com), Brian Henley (brian.henley@ntlworld.com), Louise Parratt, Emma Dent, Julia Wedlock. Introduction by Anne Strong: The Patient Participation Group thought it may be helpful to look at some of the roles that the staff at Hartley Corner Surgery undertakes – apart from the Doctors, what does everyone else do? We intend focusing on different roles over the next few newsletters, and hope you will find this of interest. Day in the Life of ….THE TRIAGE NURSE One of the members of staff you may come into contact with at the surgery is the Triage Nurse, Chris Macklin. Chris is a very experienced, qualified Registered Nurse, who has done a variety of additional clinical courses which enable her to act within this role. She is well known within the practice, as prior to becoming the Triage nurse was one of the Health Visitors for several years, and also does baby immunisations, some Asthma reviews and the Family Planning clinic. She also works some shifts at the Out Of Hours Service. Patients who have a medical problem and need advice without necessarily needing to see a Doctor, or those who wish to see a Doctor on the day but find there are no appointments available, are all referred to Chris. She is appropriately trained, and always has doctors on hand to refer to should it be necessary. The receptionist taking the call makes a list for Chris, taking the caller’s name, contact number and brief details of what the problem is – as soon as she arrives on duty, she looks through her referrals, identifying anything which in her experience needs to be dealt with as a priority. She then calls the patients back, listens to their concerns and decides on the appropriate route for each individual person. This could mean her: giving advice over the phone asking the patient to come to the surgery and see her for further assessment (she can initiate some treatments and arrange any appropriate prescriptions, and make appointments for further review if necessary) referring the patient to be seen by a Doctor as a routine appointment referring the patient to be seen by a Doctor that day as an urgent appointment if necessary, refer the patient to A&E or to call an ambulance As a qualified Nurse she has access to patient records and during the phone call she makes to each person, she can see their relevant medical history. Therefore any advice she offers or treatment she suggests is appropriate for the person concerned. At the end of each call she summarises the conversation, noting the problem, the advice or treatment she gave and any other essential information, so that when the patient next sees their Doctor everything is up to date. Some of the things she deals with on a regular basis include insect bites, nausea and vomiting, chest infections, rashes, tonsillitis, fevers and conjunctivitis. To make sure that patients don’t forget anything they may wish to talk over with her, she suggests they make a note of what they want to say, covering all their symptoms or concerns, plus the medication they are on, including any recent changes that there has been. Should the patient or their relative have to go out before Chris calls back (such as taking children to school), she makes a note of the time she rang, and then calls back within a reasonable time – she does not leave messages on answering machines to ensure patient confidentiality. This has just been a brief description of the role of the Triage Nurse, so that there is a better understanding of what she does. Anne SUMMER 2012 “HOT TOPIC” BBQ-ING IN SAFETY - article by Julia Wedlock PREVENTION OF FOOD POISONING The prevalence of ‘upset or dodgy tummy’ is doubled in the summer, possibly due to our delight at having a BBQ as soon as we see the sun – what hope this summer you may say!! However, there are many ways that we can lessen the chances of this happening by taking sensible and easy precautions with regard to food handling and preparation, to reduce the risk of food poisoning. BEFORE THE BBQ When shopping, try to buy your meat last or store in a cool bag so that it is kept cool for longer. Keep cooked meats and raw meat separate. Frozen meat must be thoroughly defrosted before cooking. Freeze any meat you are not planning to use within the next 2 days. Always keep marinated meat in the fridge – reserve a portion of the marinade to use when cooking. Take the meat out of the fridge immediately before putting it on the BBQ. COOKING ON THE BBQ Ensure plenty of clean utensils, plates and hand washing facilities or wipes to hand. Separate plates and utensils for raw and cooked meat. Pre-cooking food partially in the micro-wave, oven or hob is a good way of reducing BBQ time. Make sure the food goes immediately on the pre-heated BBQ to complete cooking Once your coals are lit, create a nice even heat which will take about 30 minutes – this will avoid food burning on the outside which will be raw inside! If you have a lid for your BBQ, keeping it down will keep the temperature constant. Remember each time you lift the BBQ lid the temperature will drop. Ensure food is sufficiently cooked by using a meat thermometer, using the chart or checking that there is no rawness when cutting into the meat. Cook food to a safe minimum internal temperature to destroy harmful bacteria. Check that there are no traces of raw meat inside your cooked meat or use a food thermometer to be sure the food has reached the minimum temperature (see chart below) Meat type Temperature Whole poultry 165F Poultry breasts 165F Ground poultry 165F Ground meats 165F Beef, pork, lamb, and veal (steaks, roast s & 145F chops) – allow to rest for 3 minutes Never partially BBQ meat and finish cooking later Keep cooked meats hot by setting them to the side of the grill, not directly over the coals. Always serve meat onto clean plates and not ones that have been used for the raw meat. Refrigerate any (cooled) leftovers promptly in shallow containers. Discard any food left more than 2hrs. Keep your BBQ clean by cleaning with a wire brush whilst it is still hot. Source: www.knoxspice.com/barbecue www.fsis.usda.gov/factsheets/Barbecue_Food_Safety www.nhs.uk FOOD POISONING ADVICE - article by Dr Hinton & Chris Macklin (Triage Nurse) With the onset of summer my colleagues and I are already seeing an increase in the number of cases of food poisoning. Food poisoning occurs when food or water contaminated with harmful germs, toxins or chemicals is eaten or drunk. It usually causes diarrhoea and cramping tummy pains with or without vomiting. Blood or mucus can appear in the stools with some infections. A high temperature headache and aching limbs can also occur. In most cases symptoms clear away over several days as the body’s system usually clears the infection, although sometimes it may take longer. If you are unlucky enough to be affected here is some advice on treatment. FLUIDS – HAVE LOTS TO DRINK. The aim is to prevent dehydration or treat dehydration if it has developed. Drink at least an extra 200mls fluid after each bout of diarrhoea. If you vomit wait 5-10 minutes and then try and sip 5mls water every 10 minutes – if tolerated with no further vomiting, slowly increase the amount of water. The best fluids to drink are water, diluted fruit juice and clear soups. Avoid milk/dairy products, and drinks with lots of sugar (fizzy drinks) as they can sometimes make diarrhoea worse. EAT AS NORMALLY AS POSSIBLE. It used to be advised to ‘starve’ for a while if you have had food poisoning. However the advice now is to eat small light meals if you can – be guided by ‘what you fancy’ and your appetite. Eat as soon as able – initially avoid fatty, spicy or heavy foods and those rich in dairy. Remember to continue to drink plenty to maintain hydration. MEDICATION Paracetamol is useful to ease a high temperature, headache and tummy cramps. Rehydration drinks – available in sachets to buy from Pharmacies are recommended for people who are frail, over the age of 60 or who have underlying health problems. Anti-diarrhoea drugs are not usually necessary. However if you have to, the safest and most effective is Loperamide. NOTE do not give to children under 12. Anti-diarrhoea drugs are not recommended for people with certain conditions and pregnant women, therefore, read the leaflet which comes with the medication to be safe. Do not take if you have a temperature, or you are passing blood or mucus with the diarrhoea. If symptoms are severe, or persist more than several days, your doctor may ask for a sample of the diarrhoea. This is sent to the ‘lab’ to look for infecting microbes (bacteria, parasites, etc.). Sometimes antibiotic or other treatments are needed if certain bacteria or other infections are found to be the cause. WHEN YOU SHOULD CONTACT THE PRACTICE FOR ADVICE If you suspect that you are becoming dehydrated. If you have blood in your diarrhoea or vomit. If you have severe abdominal pain. If you are vomiting a lot and unable to keep fluids down. If you have persisting high fever. If you have severe symptoms or you feel that your condition is getting worse. If your symptoms are not settling; i.e. vomiting for more than 2 days or diarrhoea that does not start to settle after 3-4 days. Infections caught abroad. If you are elderly or have an underlying health problem such as diabetes, epilepsy, inflammatory bowel disease, kidney disease. If you have a weakened immune system because of chemotherapy treatment, long term steroid treatment, HIV infection. If you are pregnant If you suspect that you may have contracted food poisoning from eating restaurant or takeaway food. Symptoms of dehydration in adults include: tiredness, dizziness or light-headedness, headache, muscular cramps, sunken eyes, passing little urine, a dry mouth and tongue, weakness and becoming irritable. Symptoms of severe dehydration in adults include: weakness, confusion, rapid heart rate, coma and producing little urine. This is a medical emergency! HAVING A BBQ IS ABOUT HANGING OUT WITH FAMILY AND FRIENDS, ENJOYING GREAT FOOD AND WEATHER. THESE HEALTHY TIPS WILL HELP ENSURE A SAFE AND HEALTHY SUMMER COOKING SEASON FOR YOU, YOUR FAMILY & FRIENDS……HAPPY GRILLING! HEALTHY RECIPE: - SPEEDY BEEF AND VEGETABLE STIR FRY Serves 4 Ready in under 25minutes 450g lean beef stir-fry strips 4 tbsp soy sauce 1 red chilli, deseeded and finely chopped 1 tsp grated root ginger 2 garlic cloves, peeled and crushed Low calorie cooking spray 400g pack stir- fry vegetables 100g shitake mushrooms, sliced 150ml beef stock Salt and freshly ground black pepper 4tbsp finely chopped coriander leaves Egg noodles to serve (optional) 1. In a large bowl mix the beef strips, soy sauce, red chilli, ginger and garlic together. 2. Spray a large non-stick wok or frying pan with low calorie cooking spray and place over a high heat. Add the beef and stir fry for 5minutes 3. Add the stir-fry vegetables, mushrooms and stock and stir fry for 8-10 minutes. 4. Remove from the heat, season and stir in the coriander. Serve immediately over cooked egg noodles if desired. Vary the vegetables depending on what is available – courgettes, mushrooms and red peppers make a great mix, just cut them up finely so they cook quickly.