Blood
advertisement

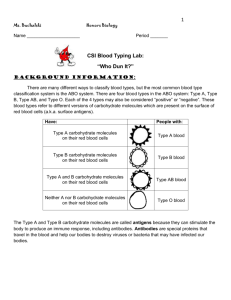
Blood I. Composition of Blood A. Formed elements are the cells and platelets (thrombocytes) and the fluid elements are the plasma and everything else suspended in it. B. Red Blood Cells (Erythrocytes) 1. Small, biconcave, anucleate (no nucleus) 2. Contain hemoglobin (about 200 million molecules per cell) a. Four polypeptide chains and four heme groups b. Heme groups bind oxygen c. Affinity of hemoglobin for oxygen changes with conditions – some conditions make it easier for oxygen to come off hemoglobin and diffuse into tissues 1) Increased temperature – working cells raise temp, need more oxygen 2) Lower pH – working cells produce lactic acid, need more oxygen to convert lactic acid to Krebs cycle intermediates 3. Counts – about 4 – 6 million per cubic millimeter of blood 4. Life span is about 120 days a. Worn out RBCs are recycled in the spleen b. Heme is broken down to bilirubin, which is converted to bile pigment in the liver C. White Blood Cells (Leukocytes) 1. Fight infection, leave blood and patrol lymph and tissues 2. Types of White Blood Cells a. Granular Leukocytes 1) Neutrophils a) Most abundant b) Multilobed nucleus joined by thin bridges of nucleoplasm – polymorphonuclear (PMNs) c) Granules don’t take up acidic or basic dyes (neutral) d) First to respond to injury i. Phagocytize bacteria and cell debris ii. Secrete oxygen free radicals iii. Secrete enzymes 2) Eosinophils a) Bilobed nucleus b) Granules take up eosin (an acidic pink dye) c) Control allergic reactions d) Fight parasitic worm infestations 3) Basophils a) U-shaped or lobed nucleus b) Granules take up basic dyes (purple) c) Release histamine, a chemical mediator of inflammation and allergic responses i. Causes vasodilation, bronchoconstriction, and secretion b. Agranular Leukocytes 1) Monocytes a) Spherical or kidney-shaped nucleus b) Leave blood and take up residence in tissues c) Differentiate into macrophages d) Phagocytize bacteria and cell debris e) Secrete enzymes and oxygen free radicals f) Secrete cytokines g) Present antigen to helper T-cells 2) Lymphocytes a) B-cells i. Have specific antigen receptors, only respond to that antigen ii. When stimulated differentiate into memory cells and plasma cells Plasma cells secrete antibodies b) T-cells i. Helper (T-4) Secrete interleukins to stimulate cytotoxic T-cells and B-cells ii. Cytotoxic (T-8) Directly attack cells that have specific antigens recognized by the T-cell receptor c) NK cells i. Third party cells, involved in tumor surveillance and anti-viral activity D. Platelets (Thrombocytes) 1. Fragments of megakaryocytes 2. No nuclei 3. Initiate blood clotting and plug hole E. Hematopoiesis 1. Formation of blood cells 2. Continuous production in bone marrow of flat bones 3. Hemocytoblast – stem cell that gives rise to all blood cells, depending upon stimulus a. Erythropoietin – produces erythrocytes (RBCs) b. Colony Stimulating Factors (CSFs) – produce leukocytes (WBCs) F. Plasma 1. Ninety two percent water (more or less) 2. Plasma proteins a. Gamma globulins 1) Antibodies b. Fibrinogen and other clotting factors 1) Fibrinogen forms basis for clot when converted to fibrin c. Complement 1) Lyse bacteria, opsonize, stimulate inflammation d. Transport proteins e. Albumin 1) Most common, big contributor to osmotic pressure in circulatory system 3. Electrolytes 4. Nutrients 5. Wastes II. Functions of Blood A. Helps maintain homeostasis B. Regulates body temperature C. Buffers pH D. Fluid and electrolyte balance E. Fight infection F. Transport 1. Exchanges between Blood and Tissue Fluid a. Oxygen and nutrients b. Carbon dioxide and wastes c. Hormones d. Mechanism 1) At arterial end of capillary a) Outward forces are greater than inward forces b) Hydrostatic pressure of blood + osmotic pressure of tissue fluid > hydrostatic pressure of tissue fluid + osmotic pressure of blood c) Fluid and nutrients move out of circulation 2) At venous end of capillary a) Inward forces are greater than outward forces b) Osmotic pressure of blood + hydrostatic pressure of tissue fluid > hydrostatic pressure of blood + osmotic pressure of tissue fluid c) Fluid and wastes move back into circulation 3) More fluid moves out than back in, excess is taken up by lymphatics G. Blood Clotting 1. The result of a series of enzymatic reactions (clotting cascade) that ultimately activate prothrombin to thrombin, the enzyme that converts soluble fibrinogen to fibrin a. Fibrin forms a mesh that helps trap platelets and RBCs to form a plug over holes in vessels b. Platelets stick to underlying connective tissue at the site of a wound and release chemicals that activate the clotting cascade c. At least 12 different clotting factors are present in blood in inactive soluble form d. Vitamin K is required for formation of good prothrombin and some other clotting factors 2. Hemophilia a. Lack of a clotting factor, leads to prolonged bleeding times and danger of hemorrhage b. May be sex linked 3. Thrombus formation a. Inappropriate clot formation (inside an unbroken vessel) b. Usually due to an imbalance of control mechanisms, may be due to stasis of blood or increased blood viscosity 4. Thromboembolism a. Emboli are floating masses in the blood; if a thrombus breaks away it is a thromboembolism b. May occlude vessels in other tissues, shutting off blood flow and leading to infarction III. Blood Groups and Typing A. ABO System 1. Antigens (proteins present on the surface of RBCs) 2. Blood type is determined by which antigens are present a. A, B, both (AB), or neither (O) b. Antibodies (preformed and directed against any ABO antigen an individual doesn’t have) 1) Anti-A, attacks any cell with the A antigen on its surface 2) Anti-B, attacks any cell with the B antigen on its surface 3) Type A people have anti-B antibodies 4) Type B people have anti-A antibodies 5) Type AB people have no anti-A or anti-B antibodies 6) Type O people have both anti-A and anti-B antibodies c. Transfusions 1) If type A people receive type B blood their anti-B antibodies will lyse the type B RBCs 2) If type A people receive type AB blood their anti-B antibodies will lyse the type AB RBCs 3) If type A people receive type A or type O blood their anti-B antibodies won’t have anything to lyse 4) If type B people receive type A blood their anti-B antibodies will lyse the type A RBCs 5) If type B people receive type A blood their anti-B antibodies will lyse the type A RBCs 6) If type B people receive type AB blood their anti-A antibodies will lyse the type AB RBCs 7) If type B people receive type B or type O blood their anti-A antibodies won’t have anything to lyse 8) Universal donor – type O 9) Universal recipient – type AB B. Rh System 1. C, D, and E antigens most common, D antigen is really the deal 2. No preformed antibodies, have to be exposed to the Rh factor to make antibodies against it 3. Won’t make anti-D antibodies if Rh+ (your immune system would kill you) 4. Rh– mother with Rh+ babies C. Blood Typing 1. Antigens present are type: A, B, AB, or O; also if Rh is present type is positive, if not type is negative IV. Effects of Aging A. Anemias, leukemias, clotting disorders increase in frequency with age B. Atherosclerosis may contribute to thrombus formation