The new antibiotics: a look at the past, a view of the present, and a
advertisement
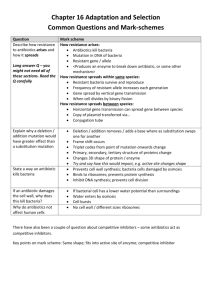
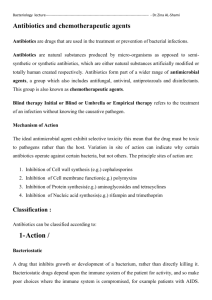
By the numbers 2 million patients in the United States get an infection as a result of a hospital stay. $122 million is the annual cost of antimicrobial resistance amongst a single pathogen (Staphylococcus aureus). 70% of the bacteria are resistant to at least one drug. What are the most common patient mistakes with antibiotics? Asking for antibiotics they don't need (viral infections) Not taking antibiotics as prescribed Stopping before the prescription runs out (encourage resistance) Saving antibiotics and later self-prescribing them. Why they don’t take them (Sanson-Fisher et al) No patients take pills more than 3 times daily. No patients take a medication for more than 5 days in a row. No patients take medication that makes them feel worse. No patients pay more than $15 of their own money for a prescription. Private lives of bacteria Bacteria have an “unembarrassed penchant for reproduction.” Francis Mah, MD Some bugs create a whole new generation every twenty minutes The antibiotic era: Began 1928 when Alexander Fleming discovered penicillin Used for World War II; general use late 1940s Is this the beginning of the end of the antibiotic era? “The bugs are getting stronger-and they’re getting stronger faster” Barry Kreiswirth Ten years ago: Nearly all strains of Streptococcus pneumoniae were susceptible to penicillin. Today: 45% of all strains are resistant. Infrastructure: Animals and agriculture Five times as many domestic food animals as people in the United States Daily animal fecal excretion can be 5-400 times greater than humans Amount of feces excreted by a cow per day is 100 times more than a human Flies carry genetically exact antibiotic-resistant organisms from nearby animals. Ground water and streams contaminated with antibiotic-resistant bacteria Used to treat fruit trees, honeybees hives, and catfish and salmon farms. The arms race “The war between humans and bacteria seems like a hopeless one because of the sheer numbers of bacteria, their incredible ability to adapt, and their unembarrassed penchant for reproduction.” Francis Mah, MD Pharmaceutical researcher’s chess game: Bacteria try to checkmate the best antibiotic move, the new antibiotic molecule attempts at checkmating the new bacterial strain Defenses Some succeeded in making cell walls impermeable Others created tiny pumps that vomited antibiotics out of the cell (efflux pump) Some have developed enzymes to attack the antibiotic and slice chemical rings Some antibiotics target an enzyme for attachment; bacteria have changed or replaced those enzymes Strict guidelines needed Correct dosing in specific and selected and properly diagnosed infections Correct period or duration of time Carefully selected patients The drugs: fluoroquinolones 3G fluorquinolones: Ciprofloxacin (Ciloxan) 5ml $40.99; Ofloxacin (Ocuflox) 5ml $40.99 3G 4G fluorquinolones: Levofloxacin (Quixin); New formulation 1.5% levofloxacin 4G fluorquinolones: Moxifloxacin (Vigamox)(oral: Avelox 1999), Gatifloxacin (Zymar)(oral: Tequin 1999) Reduced dosing: 140 patients with confirmed bacterial conjunctivitis Treated topically BID for 3 days Results: 81% were classified as microbiological successes. Bacterial keratitis 300 cases over 20 month period Risk factors found: Contact-lens wear 50.3% History of keratopathy 21% Trauma 15% Case report: Contact lens related infection History: 34 year-old female wanting SCL. In the past she reports a “red eye” with extended wear contact lens wear. Slit lamp evaluation: Inferior superficial punctate keratitis in both eyes, more dense in the right eye. Closer examination of the blink showed an incomplete blink. Diagnosis: Infiltrative keratitis and dryness Treatment: Use a steroid in combination (Tobradex)? Use an Antibiogram 4G fluorquinolone resistance Ask patient about hospital based infections and treatments. “There will be a continual need for new antibiotics because bacteria are very adaptable. We’ve already seen some resistance to fourth-generation fluoroquinolones in some ocular isolates, mainly because they have been in the systemic world for years” “Typically antibiotics have a 7 to 10 year lifespan. We hope with the proper use this will be the case with the fourth-generation fluoroquinolones as well.” Deepinder K. Dhaliwal, MD The future: 5G fluorquinolones: Trofloxacin (oral: Trovan), Azithromycin, Linezolid