A 65-year old Caucasian male presented with enlarged left
advertisement
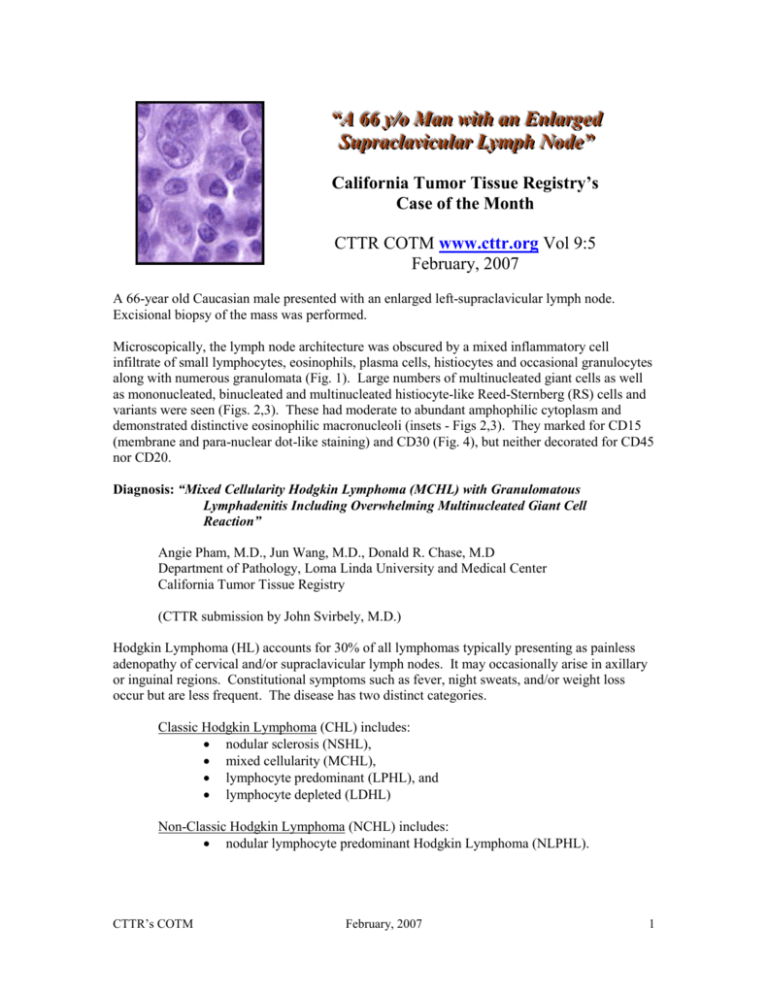
““A A 6666 yy//oo M Maann w wiitthh aann E Ennllaarrggeedd SSuupprraaccllaavviiccuullaarr LLyym mpphh N Nooddee”” California Tumor Tissue Registry’s Case of the Month CTTR COTM www.cttr.org Vol 9:5 February, 2007 A 66-year old Caucasian male presented with an enlarged left-supraclavicular lymph node. Excisional biopsy of the mass was performed. Microscopically, the lymph node architecture was obscured by a mixed inflammatory cell infiltrate of small lymphocytes, eosinophils, plasma cells, histiocytes and occasional granulocytes along with numerous granulomata (Fig. 1). Large numbers of multinucleated giant cells as well as mononucleated, binucleated and multinucleated histiocyte-like Reed-Sternberg (RS) cells and variants were seen (Figs. 2,3). These had moderate to abundant amphophilic cytoplasm and demonstrated distinctive eosinophilic macronucleoli (insets - Figs 2,3). They marked for CD15 (membrane and para-nuclear dot-like staining) and CD30 (Fig. 4), but neither decorated for CD45 nor CD20. Diagnosis: “Mixed Cellularity Hodgkin Lymphoma (MCHL) with Granulomatous Lymphadenitis Including Overwhelming Multinucleated Giant Cell Reaction” Angie Pham, M.D., Jun Wang, M.D., Donald R. Chase, M.D Department of Pathology, Loma Linda University and Medical Center California Tumor Tissue Registry (CTTR submission by John Svirbely, M.D.) Hodgkin Lymphoma (HL) accounts for 30% of all lymphomas typically presenting as painless adenopathy of cervical and/or supraclavicular lymph nodes. It may occasionally arise in axillary or inguinal regions. Constitutional symptoms such as fever, night sweats, and/or weight loss occur but are less frequent. The disease has two distinct categories. Classic Hodgkin Lymphoma (CHL) includes: nodular sclerosis (NSHL), mixed cellularity (MCHL), lymphocyte predominant (LPHL), and lymphocyte depleted (LDHL) Non-Classic Hodgkin Lymphoma (NCHL) includes: nodular lymphocyte predominant Hodgkin Lymphoma (NLPHL). CTTR’s COTM February, 2007 1 MCHL, illustrated in our case, comprises approximately 20-25% of HL and has a median presentation age of 37 years. It usually occurs in males (approximately 70%) and unlike NSHL, lacks a bimodal age distribution. Microscopically, MCHL typically obliterates the nodes follicular architecture. The distinctive feature is the presence of Reed-Sternberg cells (RS), usually binucleated cells with prominent eosinophilic macronucleoli. They are seen in a background milieu of inflammatory cells consisting of eosinophils, neutrophils, plasma cells and histiocytes. Granulomata in HL Curiously, both Hodgkin Lymphoma and Non-Hodgkin Lymphoma may present with a granulomatous lymphadenopathic microscopic appearance in either lymph node(s) or other organs, and it has been suggested that this change may portend a better prognosis. The change is morphologically non-specific as to etiology and may be caused by a myriad of etiologies related to the tumor process or separate from it. It may also obscure underlying clues to a diagnosis of lymphoma. Our presentation case shows an overwhelming granulomatous reaction with many multinucleated giant cells nearly obscuring diagnostic RS cells and variants. The granulomata of HL are described as being epithelioid histiocytes with associated Langhans or foreign-body type giant cells. Although asteroid bodies, Schaumann bodies or birefringent crystals are typically not found within the cytoplasm of the giant cells (as might be seen in sarcoidosis) a morphologic diagnosis is problematic and an attempt to explain the granulomatous inflammation should be made whenever possible. Granulomatous Lymphadenitis can be: non-infectious, including: sarcoidosis, foreign body reaction, secondary draining carcinoma, lymphoma, or infectious, including: tuberculosis, histoplasmosis, toxoplasmosis, brucellosis, tularemia, leishmaniasis, syphilis. In developing countries, infectious causes especially tuberculosis are the most likely, but in the West, the more common causes are non-infectious, especially sarcoidosis. Non-infectious Causes of Granulomatous Lymphadenitis (other than lymphoma): Sarcoidosis affects adults between the ages of 20 to 40 years and has a male to female ratio of 2:1. Blacks are nearly 10 times more frequently affected than whites. The disease is felt to be autoimmune and it tends to involve multiple organs most frequently the lungs, eyes, skin and lymph nodes. Although mediastinal and hilar lymph nodes are usually affected, generalized lymphadenopathy is possible. The characteristic granuloma is non-necrotic, composed of uniform epithelioid histiocytes, Langhans giant cells and small lymphocytes. The granulomata are sharply marginated (“punched out”). Cytoplasmic abnormalities such as Schaumann bodies, asteroid bodies, and calcium oxalate crystals may be present. But since these histologic findings may also occur in other disorders, ancillary studies are usually done including a Kviem test, a skin test, and possibly an angiotensin-converting enzyme level. The results, however, must be CTTR’s COTM February, 2007 2 correlated with the biopsy findings and the clinical setting. The diagnosis of sarcoidosis is one of exclusion. Benign lymph nodes draining carcinoma may develop granulomatous reactions secondary to the infusion of necrobiotic byproducts. Similar reactions may also be due to foreign body reactions to contrast media. Infectious Causes of Granulomatous Lymphadenitis Infectious granulomatous lymphadenitis has been described as having two distinctive granuloma morphologies: non-suppurative, hypersensitivity-type granulomata: histiocytes, with small round B cells located at the periphery suppurative granulomata: neutrophils, histiocytes, and monocytoid B cells present both at the periphery and in the center of the granuloma Tuberculosis. This classic type of suppurative infectious granulomatous lymphadenitis is typified by epithelioid granulomata having central caseating necrosis. Since necrosis is present, there may also be development of a draining sinus to the skin or through a mucosal lining. Most commonly, the cervical region (scrofula) is affected. Acid fast stain, cultures, or polymerase chain reaction are necessary to confirm presence of organisms. Atypical mycobacteria cause granulomatous lymphadenitis typically of lateral cervical lymph nodes. Microscopically, the granulomas are nearly identical to those of tuberculosis but show more neutrophils with formation of an abscess. Other clues to suggest nontuberculous mycobacterial etiology include ill-defined, irregularly shaped or serpinginous granuloma. An acid-fast stain may demonstrate the bacilli, and confirmation by PCR or cultures should identify the organisms. Fungal infections of a lymph node may show suppurative, non-supportive or both kinds of granulomata. Histoplasmosis shows a the basic reactive changes seen in stimulated lymph nodes, but also shows regions of necrosis and diffuse hyperplasia of sinus histiocytes. Blastomycosis, coccidioidomycosis, sporotrichosis, paracoccidioidomycosis, as well as opportunistic fungi (cryptococcosis, aspergillosis, mucormycosis, and candidiasis) are capable of causing fungal lymphadenitis. The organisms can be confirmed by GMS stain, cultures and molecular testing. Toxoplasmosis lymphadenitis will usually present with irregular granulomata composed of epithelioid histiocytes, marked follicular hyperplasia with small granulomas within the hyperplastic follicles, and monocytoid B cells distending the cortical and marginal sinuses. Toxoplasmosis usually involves the posterior cervical nodes of young women. Since morphologic and molecular diagnosis of toxoplasmosis is difficult, the diagnosis should be confirmed with serologic tests. Bartonella henselae, the bacteria responsible for cat-scratch disease, is the most common cause of suppurative lymphadenitis. Regional lymph nodes, mostly axillary or cervical, are usually involved showing follicular hyperplasia with monocytoid B cell proliferation within the sinuses and paracortical regions. Small suppurative granulomata are located adjacent to or within the monocytoid B cell aggregates. Later stages show stellate microabscesses with palisading CTTR’s COTM February, 2007 3 epithelioid histiocytes surrounding central necrotic fibrinoid material intermixed with neutrophils. Langhans-type giant cells are generally not present, but peripherally located mature plasma cells and immunoblasts may be seen. Clusters or chains of bacilli, which are most commonly found in the capillary walls, macrophages lining the lymph node sinuses, and areas of necrosis, are highlighted with the Warthin-Starry silver stain. The disease usually affects children and young adults, with an equal male to female ratio. Antibodies to the organism and amplification of DNA are helpful in the diagnosis. Other possible causes of granulomatous lymphadenopathy include syphilis, leprosy, lymphogranuloma venereum and Brucellosis, all of which must be confirmed with special stains, molecular or serologic tests. Suggested Reading: O’Connell M, Schimpff S, Kirschner R, Abt A, Wiernik P. Epithelioid Granulomas in Hodgkin Disease: A favorable prognostic sign? JAMA. 233: 886-889, 1975. Abrams J, Pearl P, Moody M, Schimpff S. Epithelioid Granulomas Revisited: Long-Term Follow-Up in Hodgkin’s Disease. Am J Clin Oncol (CCT). 11(4): 456-460, 1988. Braylan R, Long J, Jaffe E, Greco FA, Orr S, Berard C. Malignant Lymphoma Obscured by Concomitant Extensive Epithelioid Granulomas. Cancer 39: 1146-1155, 1977. Pak H, Friedman N. Pseudosarcoid Granulomas in Hodgkin’s Disease Hum Pathol 12(9): 832837, 1981. Silverberg S, DeLellis R, Frable W, LiVolsi V, Wick M . Silverberg’s Principles and Practice of Surgical Pathology and Cytopathology. Elsevier, Inc. 2006. CTTR’s COTM February, 2007 4