Antinociceptive role of oxytocin in the nucleus raphe magnus of rats
advertisement
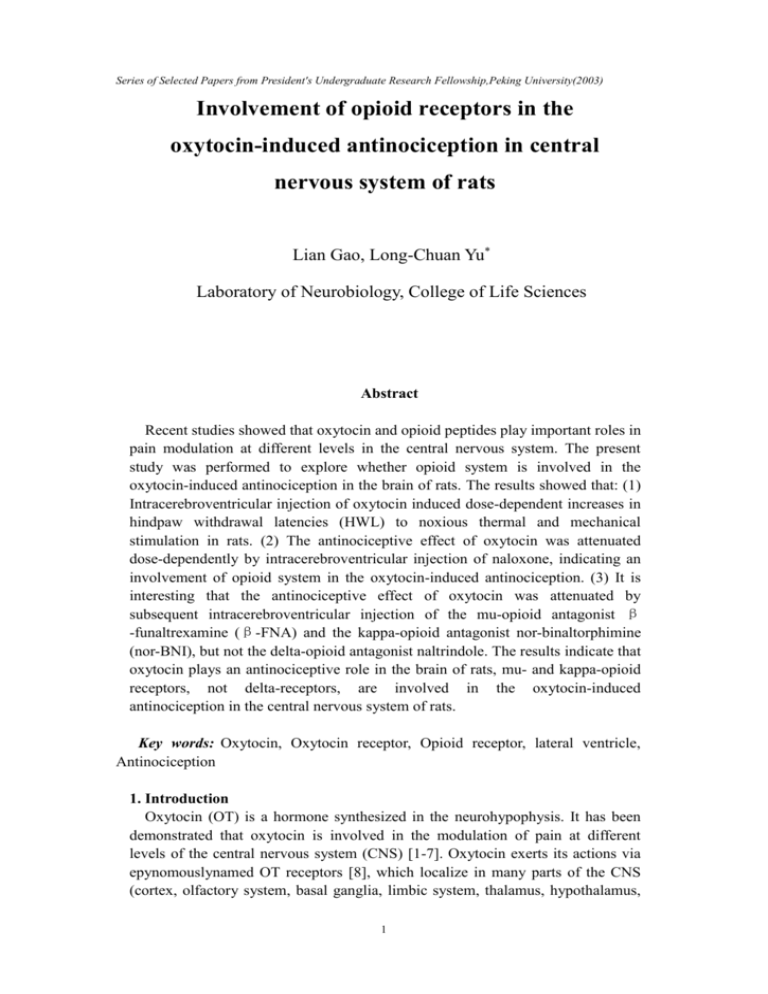
Series of Selected Papers from President's Undergraduate Research Fellowship,Peking University(2003) Involvement of opioid receptors in the oxytocin-induced antinociception in central nervous system of rats Lian Gao, Long-Chuan Yu* Laboratory of Neurobiology, College of Life Sciences Abstract Recent studies showed that oxytocin and opioid peptides play important roles in pain modulation at different levels in the central nervous system. The present study was performed to explore whether opioid system is involved in the oxytocin-induced antinociception in the brain of rats. The results showed that: (1) Intracerebroventricular injection of oxytocin induced dose-dependent increases in hindpaw withdrawal latencies (HWL) to noxious thermal and mechanical stimulation in rats. (2) The antinociceptive effect of oxytocin was attenuated dose-dependently by intracerebroventricular injection of naloxone, indicating an involvement of opioid system in the oxytocin-induced antinociception. (3) It is interesting that the antinociceptive effect of oxytocin was attenuated by subsequent intracerebroventricular injection of the mu-opioid antagonist β -funaltrexamine (β-FNA) and the kappa-opioid antagonist nor-binaltorphimine (nor-BNI), but not the delta-opioid antagonist naltrindole. The results indicate that oxytocin plays an antinociceptive role in the brain of rats, mu- and kappa-opioid receptors, not delta-receptors, are involved in the oxytocin-induced antinociception in the central nervous system of rats. Key words: Oxytocin, Oxytocin receptor, Opioid receptor, lateral ventricle, Antinociception 1. Introduction Oxytocin (OT) is a hormone synthesized in the neurohypophysis. It has been demonstrated that oxytocin is involved in the modulation of pain at different levels of the central nervous system (CNS) [1-7]. Oxytocin exerts its actions via epynomouslynamed OT receptors [8], which localize in many parts of the CNS (cortex, olfactory system, basal ganglia, limbic system, thalamus, hypothalamus, 1 Series of Selected Papers from President's Undergraduate Research Fellowship,Peking University(2003) brain stem and dorsal horn of the spinal cord) and in the peripheral nervous system. Antinociceptive effect of oxytocin has been reported in many studies. Intracerebroventricular injection of oxytocin induced antinociception [3]. Intraperitoneal or intracisternal injection of oxytocin produced antinociceptive effect in rats or in mice [9]. Madrazo et al. found that intracerebroventricular injection of oxytocin reduced suffering of a patient with intractable cancer pain [10]. There is, thus, increasing interest in the role of oxytocin in antinociception. A network of descending pathways projecting from cerebral structures to the dorsal horn of the spinal cord plays a complex and crucial role in the transmission of nociceptive information from the periphery to the CNS [8,11]. Oxytocin and opioid peptides are involved in the process. Our reports demonstrated that intra-periaqueductal gray (PAG) or nucleus raphe magnus (NRM) and intracerebroventricular injection of oxytocin induced dose-dependent antinociceptive effects in rats [5,7,12]. It is well known that opioid peptides play an important role in antinociception in the brain. The efficacy of intracerebroventricular administration of morphine has been well documented [13,14]. Also, intracerebroventricular injection of muand delta-opioid receptor agonists produced dose-dependent antinociception in the Randall Sellito test [15] and hot-plate test [16] in rats, and in mice, the intracerebroventricular administration of opioid receptor agonist have been shown to produce antinociception tested by hot-plate or tail-flick [17-19]. Furthermore, it has been demonstrated that oxytocin-induced antinociceptive effect was attenuated by intrathecal administration of the opioid antagonist naloxone, suggesting an involvement of the endogenous opioid system in the oxytocin-induced antinociception at the spinal level in rats with inflammation [20]. Recent studies in our laboratory have shown that opioid receptors were involved in the oxytocin-induced antinociception in the PAG [5] and NRM [12] of rats. The aim of the present study was to investigate the involvement of opioid receptors in the oxytocin-induced antinociception in the central nervous system of rats. 2. Materials and methods 2.1. Animals All experiments were performed on freely moving male SD rats (220–250 g; Experimental Animal Center of Henan Medical University, Henan, China). The rats were housed in cages with free access to food and water, and maintained in a room temperature of 25±2oC with a 12 h light–dark cycle. All experiments were conducted according to the guidelines of the International Association for the Study of Pain [21] and every effort was made to minimize both the animal suffering and the number of animals used. 2.2. Chemicals Solutions for intracerebroventricular injection were prepared with sterilized saline (0.9%), each with a volume of 5 μl of: (1) 0.05, 0.1 or 0.25 nmol of 2 Series of Selected Papers from President's Undergraduate Research Fellowship,Peking University(2003) oxytocin (Penisula Laboratories, USA); (2) 0.1, 0.5 or 1 μg of naloxone (naloxone hydrochloride; Sigma Chemical Company, St. Louis, MO); (3) 10 nmol of β -funaltrexamine (β-FNA hydrochloride; Tocris, Balwin, MO 63011, USA); (4) 10 nmol of nor-binaltorphimine (nor-BNI dihydrochloride; Tocris, Balwin, MO 63011, USA); (5) 10 nmol of naltrindole (naltrindole hydrochloride; Tocris, Balwin, MO 63011, USA). 2.3. Neuropharmacological experiment 2.3.1. Training before the operations All rats were accustomed to the test condition for 5 days before the experiment was carried out. After the training, the latency of hindpaw withdrawal to thermal stimulation was about 4.5-5.5 s and to mechanical stimulation was about 5-7 s. 2.3.2. The hot-plate and Randall Selitto test The response to noxious thermal stimulation was assessed by the hot-plate test [22,23]. The entire ventral surface of the rat’s hindpaw was placed manually on the hot-plate, which was maintained at a temperature of 52 oC (51.7-52.3oC). The latencies to hindpaw withdrawal during thermal and mechanical stimulation were measured and expressed in seconds to be referred to as the hindpaw withdrawal latency (HWL). The Randall Selitto Test (Ugo Basile, Type 7200, Italy) was used to assess the HWLs to noxious mechanical stimulation [22,23]. A wedge-shaped pusher at a loading rate of 30 g/s was applied to the dorsal surface of the manually handled hindpaw and the latency required to initiate the withdrawal response was assessed and expressed in seconds. In both of the tests, 15 s was the cut-off time to prevent possible tissue damage. The average values obtained before intracerebroventricular injection were regarded as the basal HWL. The HWLs recorded during subsequent experiments were expressed as percentage changes of the basal level for each rat (% changes of the HWL). Each rat was tested with both types of stimulation. 2.3.3. Intracerebroventricular injection The animals were anaesthetized by intraperitoneal pentobarbital (45 mg/kg) and were mounted on a stereotaxic instrument. A stainless steel guide cannular of 0.8 mm outer-diameter was directed into the lateral ventricle (AP, -0.92 mm; LR, 1.5 mm; V, 3.6 mm from the surface of the skull. AP, anterior (+) or posterior (-) to Bregma; L or R, left or right to midline; V, ventral to the surface of skull) according to Paxinos and Watson [24] and was fixed to the skull by dental acrylic. On the day of experiment, a stainless steel needle with 0.4 mm diameter was directly inserted into the guide cannula, with 1 mm beyond the tip of the latter. Five microliter of solution was thereafter infused into the lateral ventricle over 1 min. 2.3.4. Histologic verification of the injection site 3 Series of Selected Papers from President's Undergraduate Research Fellowship,Peking University(2003) At the end of the experiments the rat was killed by a high dose of pentobarbital (80 mg/kg) and the rat heads were fixed in 10% formalin for 24 hours with the injecting tube in situ before section. The location of the tip of the injecting tube was verified and all the tips of the injecting tube were in lateral ventricle area of rats in the present study. 2.3.5. Statistical analysis Data from nociceptive tests were presented as mean±S.E.M. The two-way analysis of variance (ANOVA) was used to evaluate the difference in HWLs between two groups (Fleft/left is the F value of the two groups: the left HWL of the first group compared with the left HWL of the second group). *P<0.05, **P<0.01 and ***P<0.001 were considered as significant differences. 3. Results 3.1. Effects of intracerebroventricular injection of oxytocin on HWLs to noxious thermal and mechanical stimulation in rats Rats received intracerebroventricular injection of 0.05 (n=6), 0.1 (n=6) or 0.25 nmol of oxytocin (n=6), or 5 μl of 0.9% saline as a control (n=8). As shown in Fig. 1, the HWLs to thermal and mechanical stimulation increased significantly after intracerebroventricular injection of 0.25 nmol of oxytocin (Thermal test: Fleft/left=26.17, P<0.001; Fright/right=59.26, P<0.001; Randall Selitto test: Fleft/left=38.72, P<0.001; Fright/right=14.58, P<0.01), but not 0.1 nmol of oxytocin (Thermal test: Fleft/left=4.16, P=0.06; Fright/right=0.68, P=0.43; Randall Selitto test: Fleft/left=8.03, P<0.05; Fright/right=2.09, P=0.17), or 0.05 nmol of oxytocin (Thermal test: Fleft/left=1.01, P = 0.33; Fright/right=0.26, P=0.62; Randall Selitto test: Fleft/left=0.36, P=0.56; Fright/right=0.13, P=0.72), compared with the control group. The HWLs increased and to reach the peak at 10 min after intracerebroventricular injection of oxytocin, and then recovered to the basal line at 30 min. 3.2. Blockade effects of intracerebroventricular injection of naloxone on the oxytocin-induced increase in HWLs Rats received intracerebroventricular injection of 0.25 nmol of oxytocin, followed 5 min later by intracerebroventricular administration of 0.1 (n=6), 0.5 (n=6) or 1 μg of naloxone (n=6), or 5 μl of 0.9% saline as a control (n=6). The results are shown in Fig. 2. Compared with the control group, the increased HWLs to thermal stimulation were attenuated significantly after administration of 1 μg (Fleft/left=21.26, P <0.001; Fright/right=38.23, P<0.001) and 0.5 μg of naloxone (Fleft/left=12.23, P<0.01; Fright/right=9.50, P<0.05), but not 0.1 μg of naloxone (Fleft/left=0.01, P=0.91; Fright/right=0.76, P=0.40) compared to the control group. And the increased HWLs to mechanical stimulation were also attenuated significantly after administration of 1 μg of naloxone (Fleft/left=15.97, P<0.01; Fright/right=15.46 P< 0.01), but not 0.5 μg (Fleft/left=1.86, P=0.20; Fright/right=1.78, P=0.21) and 0.1 μg of naloxone (Fleft/left=3.00, P=0.11; Fright/right=1.33, P=0.27) compared with the control group. Another group of rats (n=6) received 4 Series of Selected Papers from President's Undergraduate Research Fellowship,Peking University(2003) intracerebroventricular injection of 5 μl of 0.9% saline, followed 5 min later by 1 μg of naloxone. There were no marked changes in HWLs during 30 min after the injection. 3.3. Influence of different opioid antagonists on the oxytocin-induced increase in HWLs Rats received intracerebroventricular administration of 0.25 nmol of oxytocin, followed 5 min later by 10 nmol of β-FNA (n=6), 10 nmol of nor-BNI (n=6) or 10 nmol of naltrindole (n=6), or 5 μl of 0.9% saline as a control (n=6). The results are shown in Fig. 3. Compared with the control group, the increased HWLs to both thermal and mechanical stimulation were attenuated significantly after administration of 10 nmol of β-FNA (Thermal test: Fleft/left=16.05, P<0.01; Fright/right=43.98, P<0.001; Randall Selitto test: Fleft/left=24.72, P<0.001; Fright/right=14.43, P<0.01) and 10 nmol of nor-BNI (Thermal test: Fleft/left=52.17, P<0.001; Fright/right=146.81, P<0.001; Randall Selitto test: Fleft/left=13.34, P<0.01; Fright/right=21.82, P<0.001), but not 10 nmol of naltrindole (Thermal test: Fleft/left=0.87, P=0.37; Fright/right=0.03, P=0.87; Randall Selitto test: Fleft/left=0.30, P=0.60; Fright/right=0.04, P=0.84). Two groups of rats received intracerebroventricular injection of 5 μl of 0.9% saline, followed 5 min later by 10 nmol of β-FNA (n=6) or nor-BNI (n=6). There were no marked changes in HWLs during 30 min after the injection. 4. Discussion The present study showed that intracerebroventricular injection of oxytocin increased the rat’s pain threshold, and the increase in induced HWLs to both thermal and mechanical stimulation was about 40% by 0.25 nmol of oxytocin and about 20% by 0.1 nmol of oxytocin (Fig. 1). It demonstrated that oxytocin played a dose-dependent antinociceptive effect in the brain of rats. Arletti et al. found that intracerebroventricular injection of oxytocin increased the latencies of rat’s tail-flick, what could be reversed by the selective oxytocin antagonist [3]. The result demonstrated that the antinociceptive effect of oxytocin in the lateral ventricle has respect to oxytocin receptors, and indicated that oxytocin activate oxytocin receptors in the brain to modulate the nociceptive response. When high dose (10 nmol/rat) of oxytocin was used, 5-10 min after injection, rats would become paralyzed and kept barrel rotating [3]. In present study, rats were mild insane for hours after intracerebroventricular injection of 1 nmol of oxytocin, which could also increase the HWLs by about 50%. The result may be impact by both the antinociception of oxytocin and the nonspecific epilepsia, in view of that, present study use a relatively low dose, 0.25 nmol of oxytocin to minimize the influence of insanity to the thermal and mechanical test. Studies showed that in the central nervous system, the oxytocin gene is primarily expressed in magnocellular neurons in the hypothalamic paraventricular nucleus and supraoptic nucleus [25]. Action potentials in these neurosecretory cells trigger the release of oxytocin from their axon terminals in the neurohypophysis [26]. Also, studies showed that oxytocin fibers and endings have been described in nuclei around the 5 Series of Selected Papers from President's Undergraduate Research Fellowship,Peking University(2003) lateral ventricle of rats [25]. It is well known that opioid peptides play a key role in antinociception in the central nervous system [8,27,28]. Intracerebroventricular injection of opioid peptides produced dose-dependent antinociception [13-19]. Previous studies showed that oxytocin-induced antinociception could be blocked by the non-selective opioid receptor antagonist naloxone in the supraspinal level [3]. In the present study, same result was found that the oxytocin-induced increases in HWLs were attenuated significantly by administration of non-selective opioid antagonist naloxone (Fig. 2), indicating an involvement of opioid system in the process of nociceptive modulation of oxytocin in the brain. It is well known that there are three types of opioid receptors in the rat central nervous system, mu-, delta- and kappa-opioid receptors [29-31]. Interestingly, the oxytocin-induced antinociceptive effect to both thermal and mechanical stimulation were blocked significantly by intracerebroventricular administration of 10 nmol of β-FNA or nor-BNI, the antagonist of mu- and kappa-opioid receptors, but not the antagonist of delta-opioid receptors naltrindole (Fig. 3), indicating that mu- and kappa-opioid receptors, not delta0opioid receptor, are involved in the oxytocin-induced antinociception in the brain. The hot-plate and the Randall Sellito test were used to assess the effect of antinociception in the present study. According to our results, it seems that the oxytocin-induced increase of HWLs to thermal stimulation was more significant than that to mechanical stimulation. Whether oxytocin has more effect on thermal-sensor than pressure-sensor remains to be determined. Taken together, the present study demonstrated that oxytocin plays an antinociceptive role in the brain of rats, mu- and kappa-opioid receptors, not delta-receptors, are involved in the oxytocin-induced antinociception in the central nervous system of rats. Acknowledgements This study was supported by the President's Undergraduate Research Fellowship (PURF), Peking University and funds from the National Natural Science Foundation of China (NSFC). Thanks to my advisor, Professor Yu, and all my workmates in my laboratory. References [1] Raggenbass M. Vasopressin- and oxytocin-induced activity in the central nervous system: electrophysiological studies using in-vitro systems. Prog Neurobiol 2001;64:307-26. [2] Agren G, Uvnas-Moberg K, Lundeberg T. Olfactory cues from an oxytocin-injected male rat can induce antinociception in its cage-mates. 6 Series of Selected Papers from President's Undergraduate Research Fellowship,Peking University(2003) Neuroreport 1997;8:3073–6. [3] Arletti R, Benelli A, Bertolini A. Influence of oxytocin on nociception and morphine antinociception. Neuropeptides 1993;24:125-9. [4] Caron RW, Leng G, Ludwig M, Russell JA. Naloxone-induced supersensitivity of oxytocin neurones to opioid antagonists. Neuropharmacology 1998;37:887–97. [5] Ge Y, Lundeberg T, Yu LC. Blockade effect of mu and kappa opioid antagonists on the antinociception induced by intra-periaqueductal grey injection of oxytocin in rats. Brain Res 2002;927:204–7. [6] Robinson DA, Wei F, Wang GD, Li P, Kim SJ, Vogt SK, Muglia LJ, Zhuo M. Oxytocin mediates stress-induced analgesia in adult mice. J Physiol 2002;540:593-606. [7] Lund I, Yu LC, Uvnas-Moberg K, Wang J, Yu C, Kurosawa M, Agren G, Rosen A, Lekman M, Lundeberg T. Repeated massage-like stimulation induces long-term effects on nociception: contribution of oxytocinergic mechanisms. Eur J Neurosci 2002;16:330-8. [8] Millan MJ, Descending control of pain. Prog Neurobiol 2002;66:355-474. [9] Lundeberg T, Uvnasmoberg K, Agren G, Bruzelius G. Antinociceptive effects of oxytocin in rats and mice. Neurosci Lett 1994;170:153-7. [10] Madrazo I, Franco-Bourland RE, Leon-Meza VM, Mena I. Intraventricular somatostatin-14, arginine casopressin, and oxytocin: analgesic effect in a patient with intractable cancer pain. Appl Neurophysiol 1987;50:427-31. [11] Liu ZJ, Zhuang DB, Lundeberg T, Yu LC. Involvement of 5-hydroxytryptamine1A receptors in the descending anti-nociceptive pathway from periaqueductal grey to the spinal dorsal horn in intact rats, rats with mononeuropathy and rats with inflammation. Neuroscience 2002;112:399-407. [12] Wang JW, Lundeberg T, Yu LC. Antinociceptive role of oxytocin in the nucleus raphe magnus of rats, an involvement of mu opioid receptor in the effect. Regulatory Peptides 2003;115(3):153-9. [13] Yaksh TL, Rudy TA. Narcotic analgesics: CNS sites and mechanisms of action as revealed by intracerebral injection techniques. Pain 1978;4:299-359. [14] Adams JU, Tallarida RJ, Geller EB, Adler MW. Isobolographic superaddictivity between delta- and mu-opioid agonists in rat depends on the ratio of compounds, the mu-agonist and the analgesic assay used. J Pharmacol Exp Ther 1993;266:1261-7. [15] Miaskowski C, Taiwo YO, Levine JD. Contribution of supraspinal mu- and delta-opioid receptors to antinociception in the rat. Eur J Pharmacol 1991;205:247-52. [16] Dauge V, Petil F, Rossignol P, Roques BP. Use of mu- and delta-opioid peptides of various selectivity gives further evidence of specific involvement of mu-opioid receptors in supraspinal analgesia (tail-flick test). Pain 1987;14:171-8. [17] Porreca F, Mosberg HI, Hurst R, Hruby VJ, Burks TF. Role of mu- delta- and 7 Series of Selected Papers from President's Undergraduate Research Fellowship,Peking University(2003) kappa-opioid receptors in the spinal and supraspinal mediation of gastrointestinal transit effects and hot-plate analgesia in the mouse. J Pharmacol Exp Ther 1984;230:341-8. [18] Heyman JS, Mulvaney SA, Mosberg HI, Porreca F. Opioid delta-receptor involvement in supraspinal and spinal antinociception in mice. Brain Res 1987;100-8. [19] Jiang Q, Mosberg HI, Porreca F. Antinociceptive effects of [D-Ala2]deltophin II, a high selective delta-agonist in vivo. Life Sci 1990;47:PL43-7. [20] Yu SQ, Lundeberg T, Yu LC. Involvement of oxytocin in spinal antinociception in rats with inflammation. Neuroscience 2003;983:13-22. [21] Zimmermann M. Ethical guidelines for investigations of experimental pain in conscious animal. Pain 1983;16:109-10. [22] Yu LC, Hansson P, Lundeberg T. The calcitonin gene-related peptide antagonist CGRP8-37 increases the latency to withdrawal responses bilaterally in rats with experimental mononeuropathy, an effect partly reversed by naloxone. Neuroscience 1996;71:523–31. [23] Yu LC, Lundeberg S, An H, Wang FX, Lundeberg T. Effects of intrathecal galanin on nociceptive responses in rats with mononeuropathy. Life Sci 1999;64:1145-53. [24] Paxinos G, Watson C. The Rat Brain in Stereotaxic Coordinates, 3rd Edition, Academic Press, Sydney, 1998. [25] Gimpl G, Fahrenholz F. The Oxytocin Receptor System: Structure, Function, and Regulation. Physiological Reviews 2001;2:629-83. [26] Poulain DA, Wakerley JB. Electrophysiology of hypothalamic magnocellular neurons secreting oxytocin and vasopressin. Neuroscience 1982;7:773-808. [27] Fields HL, Basbaum AI. Central nervous system mechanisms of pain modulation. In: Wall, P.D., Melzack, R. (Eds.), Textbook of Pain, 4th Edition. Churchill Livingston, Edinburgh, 1999, pp. 309–29. [28] Tseng LF. The pharmacology of opioid peptides, Singapore: Harwood Academic Publishers 1995. [29] Martin WR, Eades CG, Thompson JA, Huppler RE, Gilbert PE. The effects of morphine- and nalorphine-like drugs in the nondependent and morphine-dependent chronic spinal dog. J Pharmacol Exp Ther 1976;197:517-32. [30] Gillan MGC, Kosterlitz HW. Spectrum of the mu-, delta-, and kappa-binding sites in homogenates of rat brain. Br J Pharmacol 1982;77:461-9. [31] Goldstein A, Naidu A. Multiple opioid receptors: ligand selectivity profiles and binding site signatures. Mol Pharmacol 1989;36:265-72. 8 Series of Selected Papers from President's Undergraduate Research Fellowship,Peking University(2003) %Changes of HWL to thermal stimulation 60 OT 0.25 nmol OT 0.1 nmol OT 0.05 nmol Saline 50 40 30 20 10 0 *** *** *** * ** -10 %Changes of HWL to mechanical stimulation -20 40 30 20 10 0 -10 0 5 10 15 20 25 min 30 0 5 10 15 20 25 30 Fig. 1. Effects of intracerebroventricular administration of oxytocin on HWLs to thermal (A and B) and mechanical stimulation (C and D) in rats. Left HWL: A and C; right HWL: B and D. Time=0 min: intracerebroventricular injection of 0.05, 0.1 or 0.25 nmol of oxytocin, or 5 μl of 0.9% saline as the control group. Data are presented as mean S.E.M, % change of HWL (vertical axis). Horizontal axis indicates minutes (min) after the injection. The statistical difference between groups was evaluated by two-way ANOVA. OT, oxytocin; HWL, hindpaw withdrawal latency. *P<0.05, **P<0.01 and ***P<0.001 compared with the control group. 9 min Series of Selected Papers from President's Undergraduate Research Fellowship,Peking University(2003) %Changes of HWL to thermal stimulation 70 OT 0.25 nmol + Saline 5 l OT 0.25 nmol + NX 1 g OT 0.25 nmol + NX g OT 0.25 nmol + NX 1 g Saline 5 l + NX 1 g 60 50 40 30 20 10 0 *** ** *** * ** ** %Changes of HWL to mechanical stimulation -10 50 40 30 20 10 0 -10 0 5 10 15 20 25 min 30 0 5 10 15 20 25 30 Fig. 2. Inhibitory effects of intracerebroventricular administration of naloxone on the oxytocin-induced increases in HWLs to thermal (A and B) and mechanical stimulation (C and D) in rats. Left HWL: A and C; right HWL: B and D. Time=0 min: intracerebroventricular administration of 0.25 nmol of oxytocin; Time=5 min: intracerebroventricular administration of 0.1, 0.5 or 1 μg of naloxone, or 5 μl of 0.9% saline as the control group. Data are presented as mean S.E.M, % change of HWL (vertical axis). Horizontal axis indicates minutes (min) after the injection. The statistical difference between groups was evaluated by two-way ANOVA. OT, oxytocin; NX, naloxone; HWL, hindpaw withdrawal latency. *P<0.05, **P<0.01 and ***P<0.001 compared with the control group. 10 min Series of Selected Papers from President's Undergraduate Research Fellowship,Peking University(2003) %Changes of HWL to thermal stimulation 60 OT 0.25 nmol + Saline 5 l OT 0.25 nmol + -FNA 10 nmol OT 0.25 nmol + nor-BNI 10 nmol OT 0.25 nmol + naltrindole 10 nmol 50 40 30 20 10 0 ** *** *** *** *** ** ** *** %Changes of HWL to mechanical stimulation -10 40 30 20 10 0 -10 0 5 10 15 20 25 min 30 0 5 10 15 20 25 30 Fig. 3. Influence of intracerebroventricular administration of β-FNA, nor-BNI and naltrindole on the oxytocin-induced increases in HWLs to thermal (A and B) and mechanical stimulation (C and D) in rats. Left HWL: A and C; right HWL: B and D. Time=0 min: intracerebroventricular administration of 0.25 nmol of oxytocin; Time=5 min: intracerebroventricular administration of 10 nmol of β-FNA, nor-BNI or naltrindole, or 5 μl of 0.9% saline as the control group. Data are presented as mean S.E.M, % change of HWL (vertical axis). Horizontal axis indicates minutes (min) after the injection. The statistical difference between groups was evaluated by two-way ANOVA. OT, oxytocin; β-FNA, β-funaltrexamine; nor-BNI, nor-binaltorphimine; HWL, hindpaw withdrawal latency. *P<0.05, **P<0.01 and ***P<0.001 compared with the control group. 11 min Series of Selected Papers from President's Undergraduate Research Fellowship,Peking University(2003) 作者简介: 高炼,女,1982 年 2 月出生于湖南长沙,2000 年从湖南师范大学附属中学 考入北京大学生命科学学院。在校期间学习刻苦努力,成绩优异,热心班级事务, 积极参与班上组织的各项活动,思想品德优秀,尊敬师长,人际关系良好。 2002 年进入于龙川教授的神经生物学实验室,从事神经递质,神经肽在大 鼠中枢神经系统中的痛觉调制作用的研究,取得了很多实验成果,部分工作结果 已作为合作者整理成文,投国外高水平刊物。 感悟与寄语: 能获得校长基金的资助,我觉得非常荣幸,作为一个本科生,能有这样的机 会,做科研,写论文,我觉得这是一笔难得的财富,这也得益于老师们对我的培 养,以及实验室的同学们对我的帮助,我的收获不仅仅是几篇论文,而且是一种 科学思考,不断进取的精神,这些都是我努力奋进,取得成果的动力。 在实验的过程中,我学到了很多书本上学不到的知识和技能,锻炼了自己独 立学习和科研的能力,为我以后的学习和工作打下了坚实的基础。 在此,我再次对关心和帮助我的老师和同学表示衷心的感谢。 指导教师简介: 于龙川,男,北京大学生命科学学院教授,博士生导师,北京大学生命科学 学院神经生物学实验室负责人。获博士学位(北医大,1987)和医学科学博士学 位(瑞典 Karolinska 研究院,1998)。1995 年 11 月回国并组建神经生物学研究 室,研究神经肽及其受体在中枢神经系统内对痛觉信息传递的调节作用,阿片耐 受和依赖的神经机制,以及神经肽及其受体在早老年性痴呆(Alzheimer’s Disease) 发病机理及预防和治疗中的作用。自 95 年以来在国外较高水平的学术杂志发表 科研论文约 40 篇。 12