A PRACTICAL OPTOMETRIC HEADACHE APPROACH
advertisement
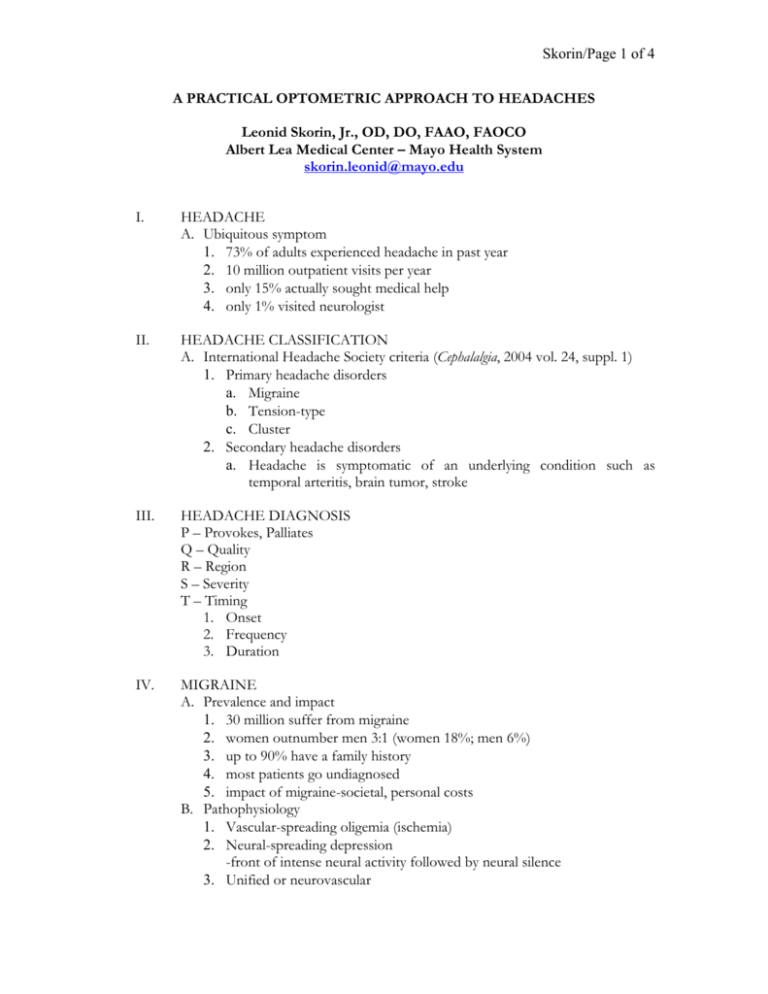
Skorin/Page 1 of 4 A PRACTICAL OPTOMETRIC APPROACH TO HEADACHES Leonid Skorin, Jr., OD, DO, FAAO, FAOCO Albert Lea Medical Center – Mayo Health System skorin.leonid@mayo.edu I. HEADACHE A. Ubiquitous symptom 1. 73% of adults experienced headache in past year 2. 10 million outpatient visits per year 3. only 15% actually sought medical help 4. only 1% visited neurologist II. HEADACHE CLASSIFICATION A. International Headache Society criteria (Cephalalgia, 2004 vol. 24, suppl. 1) 1. Primary headache disorders a. Migraine b. Tension-type c. Cluster 2. Secondary headache disorders a. Headache is symptomatic of an underlying condition such as temporal arteritis, brain tumor, stroke III. HEADACHE DIAGNOSIS P – Provokes, Palliates Q – Quality R – Region S – Severity T – Timing 1. Onset 2. Frequency 3. Duration IV. MIGRAINE A. Prevalence and impact 1. 30 million suffer from migraine 2. women outnumber men 3:1 (women 18%; men 6%) 3. up to 90% have a family history 4. most patients go undiagnosed 5. impact of migraine-societal, personal costs B. Pathophysiology 1. Vascular-spreading oligemia (ischemia) 2. Neural-spreading depression -front of intense neural activity followed by neural silence 3. Unified or neurovascular Skorin/Page 2 of 4 4. Neurogenic inflammation of trigeminal sensory fibers 5. Serotonin (5-HT)-key transmitter in migraine C. Migraine Classification 1. Migraine without aura (common migraine) 2. Migraine with aura (classic migraine) 3. Migraine aura without headache-acephalgic migraine 4. Complicated migraine a. Ophthalmoplegic migraine b. Basilar migraine c. Migraine equivalents D. Migraine Definition 1. Recurrent stereotypical head pain 2. Neurologic symptoms preceding pain 3. Pain is throbbing, unilateral 4. Autonomic nervous system dysfunction 5. Buildup and migration of scotoma 6. Frequency - variable 7. Onset 18- 30 years 8. Female predominance 9. Positive family history 10. Various potential triggers E. Migraine Treatment 1. Nonpharmacologic – Holistic a. Eliminate trigger factors b. Stress management – Relaxation techniques c. Biofeedback – Works best in children - Controls autonomic nervous system d. Physical techniques (1) Massage, acupressure (2) Acupuncture + OTC painkillers: 44% less headaches (3) Trigger point injections (4) Muscle stretching exercises (5) Osteopathic manipulation (6) Chiropractic spinal manipulation e. Homeopathic (1) Feverfew – herb, 50 to 100 mg daily – parthenolide can cause oral ulcers, tongue irritation, lip swelling (2) Riboflavin – vitamin B2-400 mg daily increases energy efficiency of mitochondria (3) Butterbur – herb, 75 mg BID x 4 months: 50% less headaches. Use the brand Petadolex. (4) Magnesium – 600 mg daily: 50% less headaches Skorin/Page 3 of 4 f. Botulinum toxin injection peripheral effect – muscle relaxant central effect – inhibits release neurotransmitters of trigeminal cell-mediated 2. Symptomatic (Abortive) a. Over-the-counter medication (1) Aspirin (2) Acetaminophen (3) Non-steroidal anti-inflammatory drugs (a) Advil Migraine – Ibuprofen 200mg (b) Motrin Migraine Pain – 200mg to 400mg per day (4) Combination drugs: (a) Excedrin Migraine – Aspirin, acetaminophen, caffeine b. Prescription medication (1) Combination drugs with narcotic (a) Fiorinal – aspirin, butalbital, caffeine (b) Fioricet – acetaminophen, butalbital, caffeine (2) Ergotamine tartrate (a) Cafergot – ergotamine, caffeine (oral or rectal) (b) Ergostat – ergotamine (sublingual) (3) Dihydroergotamine (a) D.H.E. 45 (b) Migranal (4) Narcotics: (a) Stadol NS – butorphanol (b) Demerol – meperidine (5) Midrin (a) Isometheptene,acetaminophen, dichloralphenazone (6) Selective serotonin receptor agonists (a) Imitrex (sumatriptan) Imitrex Injection SQ 6mg Nasal Spray 5mg, 20mg Tablets 25mg, 50mg, 100mg (b) Zomig (zolmitriptan) Tablets 2.5mg, 5mg Zomig-ZMT 2.5mg, 5mg orally disintegrating tablet Nasal Spray 5mg (c) Amerge (naratriptan) Tablets 1mg, 2.5mg (d) Maxalt (rizatriptan) Tablets 5mg, 10mg Maxalt-MLT orally disintegrating tablets 5mg, 10mg (e) Axert (almotriptan) Tablets 6.25mg, 12.5mg Skorin/Page 4 of 4 (f) Frova (frovatriptan) Tablet 2.5mg 26 hour half-life – all others no more than 6 hours (g) Relpax (eletriptan) Tablets 20mg, 40mg (h) Treximet (sumatriptan/naproxen) 85mg sumatriptan, 500mg naproxen sodium More effective than either single component (7) Selective Serotonin Receptor Agonists (a) Efficacy: if first triptan does not work, try another – may require trial and error (b) Onset: injection – 10-15 minutes nasal spray – 15 minutes troche – no faster than oral tablets (c) Route: nasal spray or injection for nausea/vomiting (d) Duration: longest acting – Frova and Amerge 3. Prophylactic (Preventative) a. Beta blockers (1) Inderal – propranolol (2) Tenormin – atenolol b. Tricyclic antidepressants (1) Elavil, Endep – amitriptyline c. Nonsteroidal anti-inflammatory drugs (1) Anaprox, Anaprox DS – naproxen sodium (2) Naprosyn – Naproxen d. Calcium channel blockers (1) Calan – verapamil (2) Procardia – nifedipine e. Monoamine oxidase inhibitors (1) Nardil – phenelzine f. Anticonvulsants (1) Depakote – divalproex (2) Depakote ER – extended release QD dosing (3) Depakene – valproic acid (4) Topamax – topiramate reduces migraine attacks by 50% in 6 weeks