Glycopeptides
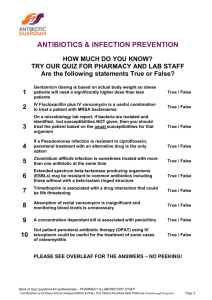
advertisement
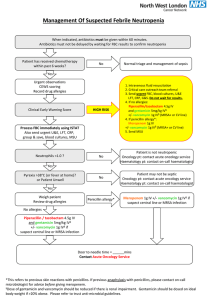
Glycopeptides Glycopeptides is a group of antibiotics composed of glycosylated cyclic or polycyclic nonribosomal peptides. The most common glycopeptide antibiotics include vancomycin, teicoplanin, telavancin, bleomycin, ramoplanin, and decaplanin. Vancomycin has been used in clinical practice since 1958, teicoplanin from the middle of 1980th years. For the last10 years the popularity of this group of antibacterial preparation is increased because of high frequency of infections caused by grampositive microorganisms. Currently glycopeptides are used in the first line treatment of infections caused by MRSA, MRSE and enterococcal infections resistant to ampicillin and aminoglycosides. Action mechanism Glycopeptides work by interfering with synthesis of bacterial cell wall. They exert bactericidal action, however, the effect against enterococci, streptococci and coagulase-negative staphylococcus is bacteriostatic. Spectrum of activity Glycopeptides are active against Gram-positive aerobic and anaerobic microorganisms: Staphylococcus (including MRSA, MRSE), streptococci, pneumococci (including PRA), enterococci, peptostreptococci, Listeria, corynebacteria, clostridia (including C.difficile). Gram-negative bacteria are resistant to glycopeptides. The spectrum of activity of all Glycopeptides is almost similar. The difference are in the level of activity and acquired resistance. For example, teicoplanin is more active against S.aureus (including MRSA), streptococci (including S.pneumoniae) and enterococci. Vancomycin is more active against coagulase-negative staphylococcus. For the recent 1 years, there was found S.aureus with reduced susceptibility to vancomycin and teicoplanin. The resistance to vancomycin develops quickly. Indications Infections caused by MRSA and MRSE. Staphylococcal infections in case of allergy to β-lactamase. Severe infections caused by Enterococcus spp., C.jeikeium, B.cereus, F.meningosepticum. Infectious endocarditis caused by streptococci and S.bovis, with allergies to β-lactamase. Infective endocarditis caused by E.faecalis (in combination with gentamicin). Meningitis caused by S.pneumoniae, resistant to penicillin. Empirical therapy of life-threatening infections: Infectious endocarditis of the tricuspid valve or prosthetic valve (in combination with gentamicin) Catheter-associated sepsis Posttraumatic or postoperative meningitis (in combination with cephalosporins III generation or fluoroquinolones); Peritonitis in peritoneal dialysis Neutropenic fever Antibiotic-associated diarrhea caused by C.difficile Prevention of wound infection in orthopedic and cardiac surgery in institutions with high prevalence of MRSA or allergy to β-lactams; Prevention of endocarditis in high risk patients 2 Contraindications Hypersensitivity to any of the medication ingredients Pregnancy Breastfeeding Warnings Pregnancy. Glycopeptides are not recommended for use during pregnancy because of high risk of oto-, neuro and nephrotoxicity. Breastfeeding. Small amounts of Glycopeptides penetrate through breast milk. Glycopeptides can change intestinal microflora in children. Pediatric use. Glycopeptides should be used with caution in children because of high risk of oto-, neuro- and nephrotoxicity. Glycopeptides are indicated when benefits of application overweights possible risks. Geriatric use. Glycopeptides should be used with caution in elderly age because of high risk of nephrotoxicity. The dose of the medications should be adjusted in patients with kidney diseases. Urinary system. Kidney damage is more common for vancomycin, The risk of renal failure is increased in patients with a history of kidney diseases, hypovolemia, prolonged therapy, concomitant application with nephrotoxic drugs (aminoglycosides, amphotericin B, polymyxin B, cyclosporine, furosemide, ethacrynic acid). During the treatment it is necessary to monitor urine outflow, creatinine blood levels. Residual concentrations of vancomycin in the blood should not exceed 10 mg/liter. 3 Ototoxicity and vestibular disorders. Usually ototoxicity is reversable, in rare cases irreversible deafness may develop. Intravenous application. In rapid intravenous administration of vancomycin, hypotension, chest pain, tachycardia, facial flushing may occur. Glycopeptides side effects Urinary system: reversible renal failure (increase of creatinine and urea blood levels, anuria) The frequency of nephrotoxic reactions depends on dose, duration of treatment and patient's age. The risk is increased when glycopeptides are used in combination with aminoglycosides, furosemide, or ethacrynic acid. Nephrotoxicity and renal failure are more common for vancomycin than for teicoplanin CNS: dizziness, headache Ototoxicity: loss of hearing, vestibular disorders in patients with impaired renal function which receive high doses of vancomycin Local reactions: pain, burning sensation at the injection site, phlebitis Allergic reactions: rash, hives, fever, anaphylactic shock Hematologic reactions: reversible leukopenia, thrombocytopenia Gastrointestinal tract: nausea, vomiting, diarrhea Liver: transient increase in activity of transaminases, alkaline phosphatase Vancomycin Generic Name (active ingredient): Vancomycin Vancomycin is an antibacterial drug, which was derived from Amycolatopsis orientalis, the drug exerts bactericidal effects to a broad spectrum of microorganisms. 4 Mechanism of action The preparation works by blocking the synthesis of the bacterial cell wall, however the drug does not work on the same fragment of the cell wall like penicillins and cephalosporins, thus the resistance to these antibiotics will not affect Vancomycin. The drug binds to the predecessor of the cellular wall thus causing the cell to lyze. The drug also is able to penetrate the cellular membrane of the bacteria and selectively inhibit RNA synthesis. The drug is active against a broad spectrum of grampositive microorganisms. The preparation actively affects only bacterial cells that are in the process of replication. Most of the gram-negative bacteria are resistant to the drugs effect. The preparation does not express cross resistance to other antibiotics. 5