Autologous Bone Marrow Transplantation for Critical, Limb

Home Search Listings Resources Help What's New About
Autologous Bone Marrow Transplantation for Critical, Limb-
Threatening Ischemia
This study is currently recruiting patients.
Verified by Franziskus-Krankenhaus May 2007
Sponsored by: Franziskus-Krankenhaus
Information provided by: Franziskus-Krankenhaus
ClinicalTrials.gov Identifier: NCT00434616
Purpose
Critical limb ischemia is a condition where the blood circulation in the limbs, in most cases the legs, is decreased so that pain and non healing wounds ensue. Mostly, this is a sequel of arteriosclerosis and/or diabetes. If surgical and other methods for the improvement of blood supply for the leg have failed or are not possible, most of these patients will proceed to amputation of the leg.
Bone marrow contains cells which can induce and augment the growth of new, small arteries called collateral arteries. It has been shown in animals and in some case series that the transplantation of a concentrate of the patient’s own bone marrow into the ischemic limb can improve the blood circulation via the induction of collateral growth.
However, it is not known if this bone-marrow induced collateral growth is sufficient to avoid otherwise necessary amputations.
Therefore, we conduct a study to compare the efficiency of concentrated bone marrow cells injected into the critically ischemic limb compared to a placebo procedure where only saline is injected. We think that the transplantation of autologous bone marrow will reduce the number of necessary leg amputations, reduce pain and induce wound healing.
In this investigation, patients with limb threatening ischemia are randomly allocated either to the bone marrow group or to the placebo group. Patients in the bone marrow group will have their bone marrow harvested under sedation , and the bone marrow cells are concentrated. The cell concentrate will then be injected directly into the muscle of the diseased leg. Patients in the placebo group will undergo sedation as well but no bone marrow harvest is done, and saline is injected into the ischemic leg. The procedure will require about 1.5-2 hours, and the subjects will be admitted to the Franziskus Hospital-
Berlin Vascular Centre. Monthly examinations up to three months after the bonemarrow or placebo procedure are done. After the follow-up of three months, the rate of death and amputations and the wound healing process are compared between groups.
Adverse and serious adverse events will be recorded during this time period. Diagnostic studies will be obtained to measure blood flow in the treated leg during the follow up period and include skin oxygen measurements, pressure recordings in the leg and arteriography. Also, quality of life, pain and wound healing will be assessed.
After completion of the three months study participation, subjects who have been treated with placebo will be able to receive open-label bone marrow transplantation therapy.
Condition
Peripheral Vascular
Disease
Diabetic Foot
Peripheral Arterial
Occlusive Disease
Leg Ulcer
Gangrene
Ischemia
Intervention
Procedure: Autologous bone marrow cell concentrate transplantation
Phase
Phase
II
Phase
III
MedlinePlus related topics: Diabetic Foot ; Leg Injuries and Disorders ;
Peripheral Vascular Diseases ; Vascular Diseases
Genetics Home Reference related topics: Vascular Diseases
Study Type: Interventional
Study Design: Treatment, Randomized, Double-Blind, Placebo Control,
Parallel Assignment, Safety/Efficacy Study
Number of arms in study: 2
Official Title: Security and Effectiveness of Autologous Bone Marrow
Transplantation to Avoid Amputations in Patients With Limb-Threatening
Ischemia: a Single-Center Randomized Placebo-Controlled Double-Blind Study
Further study details as provided by Franziskus-Krankenhaus:
Primary Outcome Measures:
Major amputation of the index limb [Time Frame: 3 months]
Persisting critical limb-threatening ischemia [Time Frame: 3 months]
Secondary Outcome Measures:
Wound healing (wound size, wound stage)
Pain and analgesics use
Rutherford grade and stage
Walking distance (treadmill) if possible
Quality of life (EQ-5D Questionnaire)
Transcutaneous oxygen pressure (TcpO2), ABI, absolute ankle perfusion pressure
Collateral artery number as judged by contrast angiography after 3 months
Rate and extent of minor (below the ankle) amputations
survival without amputation [Time Frame: 3 months]
Total Enrollment: 90
Study start: April 2007; Expected completion: December 2008
Peripheral arterial disease (PAD) represents very advanced arteriosclerosis. It is not unusual for this condition to result in limb-threatening ischemia that usually results in amputation of the limb.About 150.000 thigh or calf amputations due to PAD are done annually in the United states.
Treatment of critical limb threatening ischemia (corresponding to Rutherford grade II or
III) consists of revascularization of the leg with critically reduced blood supply.
Depending on the localization and morphology of the occlusion, surgical revascularization by means of bypass surgery or catheter-based percutaneous transluminal angioplasty (PTA) may be used (even as a complementary procedure).
However, successful revascularization is possible in only max. 60% to 70% of the patients affected. Patients with limb threatening ischemia which cannot be revascularized have a one–year amputation rate exceeding 80% and a 20-30% mortality.
Several studies have shown that in less advanced PAD the implantation of a concentration of mononuclear cells harvested from the patient’s own bone marrow has been effective in developing collateral vessel formation translating into an improvement in PAD symptoms. Additional clinical evidence that this simple, safe and inexpensive therapy can induce therapeutic angiogenesis in the ischemic limb sufficient to prevent amputation would be valuable to both patients and clinicians.
This single-centre study will evaluate the clinical potential for the implantation of a concentration of bone marrow mononuclear cells for therapeutic angiogenesis through the augmented formation of collateral vessels in the ischemic limb. It is a placebocontrolled, 1:1 randomised study with a total of 90 patients included. The placebo procedure consists of a sham bone marrow puncture where no bone marrow aspiration is done; instead, only a stab puncture of the skin is made.
The bone marrow cell concentrate will be prepared “point of care”, patient-side from an aspirate of 240 mL of bone marrow. A concentrate volume of 40-50 mL will be injected into 40-50 sites in the muscles of the ischemic limb. A blinded physician injects either the bone marrow cell concentrate or the visually identical placebo solution into the ischemic leg.
Improvement in perfusion of the limb will be measured using clinical assessment and ankle-brachial-index (ABI), transcutaneous oxygen (TcPO2) and contrast angiography.
Quality of life and pain will be assessed.
Study participation ends for the subjects after a follow-up of three months with monthly visits. After this, clinical and perfusion status are recorded at least three-monthly up to two years after study inclusion.
HYPOTHESIS:
Implantation of Bone Marrow Aspirate Concentrate (BMAC) can be clinically effective in treating critical limb threatening ischemia so that the number of amputations can be reduced.
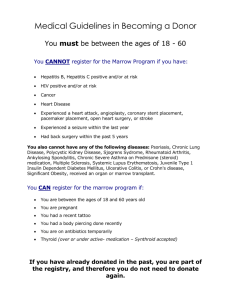
Inclusion criteria:
Presence of Critical Limb ischemia according to the guidelines of the
Transatlantic Consensus Group (TASC) Rutherford grade II or III. Perfusion is measured with absolute perfusion pressure and ankle-brachial index (ABI) and transcutaneous oxygen tension (TcpO2); for inclusion, ABI has to be less than or equal to 0.6 or absolute ankle pressure must be less than 60 mmHg. If ABI is technically not feasible, e.g. in patients with media calcification, inclusion criteria are a tcpO2 value (supine, forefoot, 44°C) of less than 20 mmHg if there is no tissue loss, or a tcpO2 of less than 40 mmHg if there is tissue loss.
No sufficient response to best standard care delivered for six weeks.
No surgical or radiological interventional option for revascularisation as confirmed by a vascular surgeon and an interventional radiologist
Age older than 18 years
Signed informed consent
Absence of life-threatening complications from the ischemic limb
Exclusion criteria:
Expected life span less than six months
Bone marrow diseases which preclude transplantation (eg lymphoma, leukaemia, myelodysplastic syndrome and others)
Renal failure on hemodialysis
Life threatening complications of limb ischemia with the need for immediate limb amputation to avoid death or clinical deterioration
End points:
Primary end point:
Major amputation (above the ankle) of the index limb after 3 months or persisting critical limb ischemia of the index limb after three months
Secondary end points:
Wound healing (wound size, wound stage)
Pain and analgesics use
Rutherford grade and stage
Walking distance (treadmill) if possible
Quality of life (EQ-5D Questionnaire)
Transcutaneous oxygen pressure (TcpO2), ABI, absolute ankle perfusion
pressure
Collateral artery number as judged by contrast angiography after 3 months
Rate and extent of minor (below the ankle) amputations in the index limb
Eligibility
Ages Eligible for Study: 18 Years - 95 Years, Genders Eligible for Study: Both
Criteria
Inclusion Criteria:
Presence of Critical Limb ischemia according to the guidelines of the
Transatlantic Consensus Group (TASC) Rutherford grade II or III. Perfusion is measured with absolute perfusion pressure and ankle-brachial index (ABI) and transcutaneous oxygen tension (TcpO2); for inclusion, ABI has to be less than or equal to 0.6 or absolute ankle pressure must be less than 60 mmHg. If ABI is technically not feasible, e.g. in patients with media calcification, inclusion criteria are a tcpO2 value (supine, forefoot, 44°C) of less than 20 mmHg if there is no tissue loss, or a tcpO2 of less than 40 mmHg if there is tissue loss.
No sufficient response to best standard care delivered for six weeks.
No surgical or radiological interventional option for revascularisation as confirmed by a vascular surgeon and an interventional radiologist
Age older than 18 years
Signed informed consent
Absence of life-threatening complications from the ischemic limb
Exclusion Criteria:
Expected life span less than six months
Bone marrow diseases which preclude transplantation (eg lymphoma, leukaemia, myelodysplastic syndrome and others)
Renal failure on hemodialysis
Life threatening complications of limb ischemia with the need for immediate limb amputation to avoid death or clinical deterioration
Location and Contact Information
Please refer to this study by ClinicalTrials.gov identifier NCT00434616
Berthold Amann, MD ++49-30-26380 amann@franziskus-berlin.de
Andre Schmidt-Lucke, MD ++49-30-2638-0 Ext. 3600 sl-innere@franziskusberlin.de
Germany
Franziskus Hospital Berlin Vascular Center, Berlin, D 10787, Germany; Recruiting
Berthold Amann, MD, Principal Investigator
Study chairs or principal investigators
Berthold Amann, MD, Principal Investigator, Franziskus Hospital, Berlin Vascular
Center
More Information
Home page of Berlin Vascular Center
Publications
Tateishi-Yuyama E, Matsubara H, Murohara T, Ikeda U, Shintani S,
Masaki H, Amano K, Kishimoto Y, Yoshimoto K, Akashi H, Shimada K,
Iwasaka T, Imaizumi T; Therapeutic Angiogenesis using Cell
Transplantation (TACT) Study Investigators. Therapeutic angiogenesis for patients with limb ischaemia by autologous transplantation of bone-marrow cells: a pilot study and a randomised controlled trial. Lancet. 2002 Aug
10;360(9331):427-35.
Durdu S, Akar AR, Arat M, Sancak T, Eren NT, Ozyurda U. Autologous bone-marrow mononuclear cell implantation for patients with Rutherford grade II-III thromboangiitis obliterans. J Vasc Surg. 2006 Oct;44(4):732-9.
Epub 2006 Aug 22.
Iba O, Matsubara H, Nozawa Y, Fujiyama S, Amano K, Mori Y, Kojima H,
Iwasaka T. Angiogenesis by implantation of peripheral blood mononuclear cells and platelets into ischemic limbs. Circulation. 2002 Oct
8;106(15):2019-25.
Nizankowski R, Petriczek T, Skotnicki A, Szczeklik A. The treatment of advanced chronic lower limb ischaemia with marrow stem cell autotransplantation. Kardiol Pol. 2005 Oct;63(4):351-60; discussion 361.
English, Polish.
Hernandez P, Cortina L, Artaza H, Pol N, Lam RM, Dorticos E, Macias C,
Hernandez C, Del Valle L, Blanco A, Martinez A, Diaz F. Autologous bone-marrow mononuclear cell implantation in patients with severe lower limb ischaemia: A comparison of using blood cell separator and Ficoll density gradient centrifugation. Atherosclerosis. 2006 Sep 15; [Epub ahead of print]
Study ID Numbers: 2006-001825-24; FKH 200
Last Updated: May 9, 2007
Record first received: February 9, 2007
ClinicalTrials.gov Identifier: NCT00434616
Health Authority: Germany: Paul-Ehrlich-Institut
ClinicalTrials.gov processed this record on May 23, 2007
U.S. National Library of Medicine , Contact NLM Customer Service
National Institutes of Health , Department of Health & Human Services , USA.gov
Copyright , Privacy , Accessibility , Freedom of Information Act