NEONATES RETRIEVED FOR CONGENITAL HEART DISEASES
advertisement

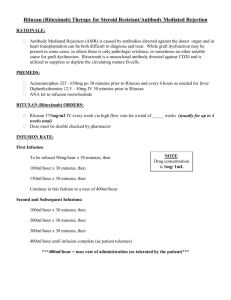
P51 NEONATES RETRIEVED FOR CONGENITAL HEART DISEASES - THE EXPERIENCE OF A RETRIEVAL SERVICE Dutta S, Bhuta T, Berry A NSW newborn and paediatric Emergency Transport Service, NETS) Background: There is a paucity of information in the literature regarding the spectrum of patients presenting with congenital heart diseases requiring emergency retrieval and also the management of patients requiring prostaglandin (PGE1) infusion for ductus dependent lesions during retrieval. Aims: (1) To study the demographics of patients with congenital heart disease transported by NETS. (2) To study the group of patients who required PGE1 infusion during retrieval, the need for intubation and ventilation, the side effects and predictors of response to PGE 1 infusion. Methods: Retrospective case review of patients retrieved by NETS from 1-9-95 to 30-4-97 from the NETS database and case notes. Only patients transported to a higher level of care and who had a final echo-proven diagnosis of structural congenital heart disease were included in the study, The distribution of various cardiac lesions; the demographic data and the use of various treatment modalities during transport were studied for each diagnostic category. Response rates to PGE1 were determined for different diagnostic groups. Results: 217 patient records were reviewed and 101 patients were excluded [no heart disease on echo (n=47), primary pulmonary hypertension (a=8), non-structural heart diseases (n=7), reverse transported (n=17), preterm infants with PDA (n=22)]. The remainder (n=116) had structural lesions; 67% were classified as cyanotic heart disease and 33% as acyanotic heart disease. 46% of cyanotic patients had d-transposition of great arteries (TGA). 44% of patients had decreased pulmonary flow, of which pulmonary atresia (PA) was the commonest. In the acyanotic group 45% of patients had left to right shunts, the commonest being ventricular septal defects (VSD). 37% of acyanotic patients had coarctation of aorta (CoA), The mean age at presentation was < l day for all cyanotic heart lesions except for total anomalous pulmonary venous return (5 days). Patients with acyanotic lesions generally presented later, the mean age being 20 days for VSD and 9 days for CoA. 51.3% of cyanotics and 44.7% of acyanotics were mechanically ventilated. 47.4% of all cyanotics received PGE 1 infusion whereas only 21% of acyanotics received PGE1. The response rate to PGE1 infusion for patients with TGA decreased pulmonary flow and CoA were 84%, 84º/o and 66% respectively. Of the 46 patients who received PGE 1 17.4% were not ventilated (n=8) and of them only one developed apnoea (dose of 33 ng/kg/min). The odds of responding to PGE1 were 10 fold higher if the PaO2 was < 40 mm Hg [95% confidence intervals (CI) 1.17, 128]. There was no significant difference in rate of response between high dose PGE 1 infusion (> 50 ng/kg/min) and low dose PGE1 infusion (< 50 ng/kg/min), odds ratio (OR) 1.23 (95% CI 0.3, 4.7). Age 1 week, term gestation, fractional inspired O2 (0.21) and baseline pH <7.25 did not predict response to PGE 1 infusion; ORs were 1.3, 1.0, 0.87 and 1.14 respectively. Conclusions: Mechanical ventilation and prostaglandin infusions were administered to a large proportion of patients with no major complications. Low dose PGE1 was as effective as high dose PGE1 infusion. The only predictor of response to PGE1 infusion was low PaO2. None of the non-ventilated patients receiving a PGE1 infusion of <33 ng/kg/min developed apnoea. We speculate that “well" newborns with ductus dependent congenital heart disease on low dose PGE 1 infusion can be retrieved without mechanical ventilation,