Obesity
advertisement
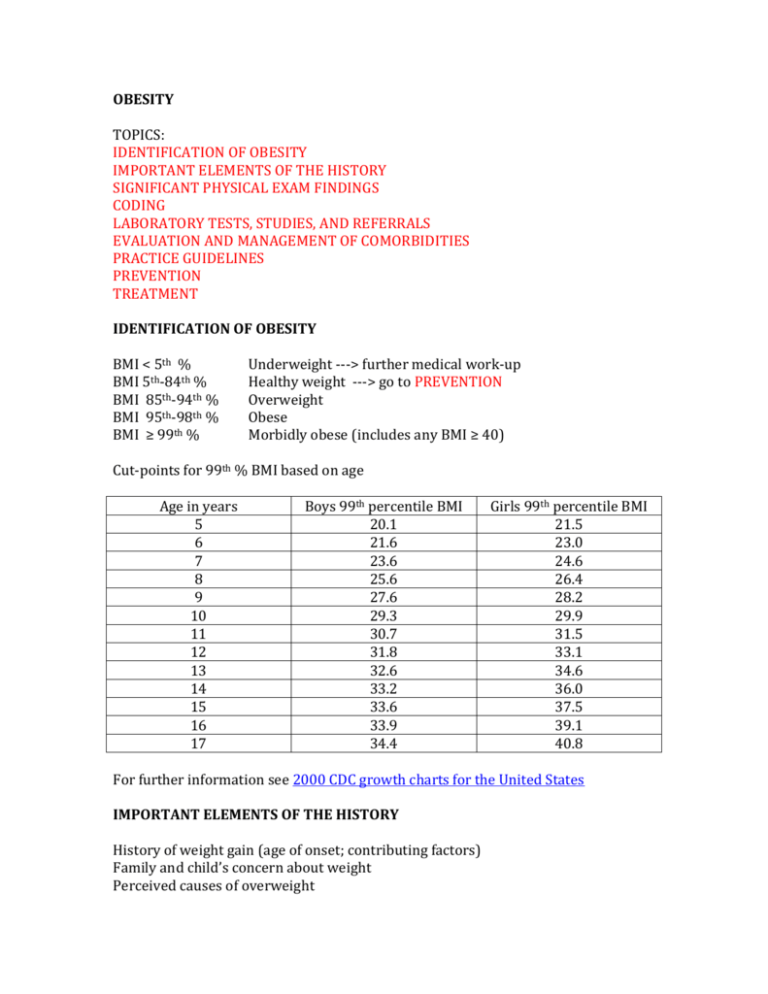
OBESITY TOPICS: IDENTIFICATION OF OBESITY IMPORTANT ELEMENTS OF THE HISTORY SIGNIFICANT PHYSICAL EXAM FINDINGS CODING LABORATORY TESTS, STUDIES, AND REFERRALS EVALUATION AND MANAGEMENT OF COMORBIDITIES PRACTICE GUIDELINES PREVENTION TREATMENT IDENTIFICATION OF OBESITY BMI < 5th % BMI 5th-84th % BMI 85th-94th % BMI 95th-98th % BMI ≥ 99th % Underweight ---> further medical work-up Healthy weight ---> go to PREVENTION Overweight Obese Morbidly obese (includes any BMI ≥ 40) Cut-points for 99th % BMI based on age Age in years 5 6 7 8 9 10 11 12 13 14 15 16 17 Boys 99th percentile BMI 20.1 21.6 23.6 25.6 27.6 29.3 30.7 31.8 32.6 33.2 33.6 33.9 34.4 Girls 99th percentile BMI 21.5 23.0 24.6 26.4 28.2 29.9 31.5 33.1 34.6 36.0 37.5 39.1 40.8 For further information see 2000 CDC growth charts for the United States IMPORTANT ELEMENTS OF THE HISTORY History of weight gain (age of onset; contributing factors) Family and child’s concern about weight Perceived causes of overweight Consequences of overweight in child’s life Previous attempts at weight loss DIET AND PHYSICAL ACTIVITY: Food preferences Behavioral feeding problems Meal patterns Snacks Sugary beverages Eating out Screen time Activity patterns Nutrition Patient Care Forms on the LPCH intranet: Weekly food diary (7-day record of diet and activity) Monthly exercise log OBESITY-INDUCING MEDICATIONS: Steroids Anticonvulsants (valproic acid, gabapentin) Psychiatric drugs (antipsychotics, tricyclic antidepressants, lithium) Hormonal contraceptives SYMPTOMS: Headaches ---> consider pseudotumor cerebri Snoring ---> consider sleep apnea Daytime sleepiness ---> consider sleep apnea Shortness of breath ---> consider congestive heart failure Abdominal pain ---> consider GE reflux (burning pain) or NASH (RUQ pain) Constipation Irregular menses or amenorrhea ---> consider pregnancy, PCOS and/or hypothyroidism Hip or knee pain ---> consider slipped capital femoral epiphysis Back pain Darkening of the skin on neck and/or axillae ---> consider diabetes Nocturia or polyuria ---> consider diabetes Poyldipsia ---> consider diabetes Binging ---> consider an eating disorder Purging ---> consider an eating disorder READINESS FOR CHANGE: Prochaska and DiClemente’s Stages of Change Precontemplation Contemplation Preparation Action Maintenance SIGNIFICANT PHYSICAL EXAM FINDINGS High blood pressure ---> further evaluation for hypertension Short stature (ht < 25th %) ---> consider endocrine abnormality Eyes: blurred disc margins ---> consider pseudotumor cerebri Face: abnormal facies ---> consider genetic syndrome Throat: enlarged tonsils ---> consider sleep apnea Neck: mass ---> consider enlarged thyroid and hypothyroidism Abdomen: RUQ tenderness ---> consider NASH Back: buffalo hump ---> consider Cushing’s syndrome Extremities: bowed legs ---> consider Blount’s disease Genitalia: precocious puberty ---> consider endocrine abnormality; undescended testicle ---> consider Prader-Willi syndrome OMIM #176270 delayed puberty ---> consider hypothyroidism Precocious puberty: < 8 years in girls and < 9 years 6 months in boys Delayed puberty: no pubertal development by age 13 in girls and 14 in boys Skin: acanthosis nigricans ---> insulin resistance; consider diabetes striae ---> consider Cushing’s syndrome CODING: WEIGHT: Overweight (ICD-9 278.02): BMI 85th-94th % Obese (ICD-9 278.00): BMI 95th-98th % Morbidly obese (ICD-9 278.01) BMI ≥ 99th % Abnormal weight gain (ICD-9 783.1) COMORBIDITIES: Acne (ICD-9 706.1) Back pain (ICD-9 724.5) Blount’s disease (ICD-9 732.4) Constipation (ICD-9 564.00) ---> fiber-rich diet Depression (ICD-9 296.2) Diabetes mellitus, type 2 (ICD-9 250.02 – uncontrolled) Disordered eating (ICD-9 307.5) Dyslipidemia (ICD-9 272.4) Fatty liver (ICD-9 571.8) Gastroesophageal reflux (ICD-9 530.81) Gynecomastia (ICD-9 611.1) Hypercholesterolemia (ICD-9 272.0) Hyperlipidemia (ICD-9 272.4) Hypertriglyceridemia (ICD-9 272.1) Hypertension (ICD-9 401.9) Impaired fasting glucose (ICD-9 790.21) Impaired glucose tolerance (ICD-9 790.22) Insulin resistance (ICD-9 251.1) Iron-deficiency anemia (ICD-9 280.9) Irregular menses (ICD-9 626.4) Left ventricular hypertrophy (ICD-9 746.89) Obstructive sleep apnea (ICD-9 327.23) Polycystic ovary syndrome (ICD-9 256.4) Pseudotumor cerebri (ICD-9 348.2) Slipped capital femoral epiphysis (ICD-9 732.2) Vitamin D deficiency (ICD-9 268.9) LABORATORY TESTS, STUDIES, AND REFERRALS AAP GUIDELINES FOR LABS: BMI 85th-94th % (≥ 2 years old): Fasting lipid panel •Repeat every 2 years BMI ≥ 95th % (≥ 10 years old): Fasting lipid panel Fasting glucose AST, ALT • Repeat every 2 years Also consider: CBC BUN, creatinine Electrolytes Comprehensive metabolic panel Fasting insulin level Free T4, TSH High-sensitivity CRP (for assessment of inflammation and cardiovascular risk) LH, FSH, prolactin, free and total testosterone, DHEAS, androstenedione, SHBG (for PCOS) Leptin MC4R (for early onset obesity)---> send-out to Athena Diagnostics Prader-Willi FISH probe (fluorescent in-situ hybridization) Vitamin D, 25-OH ---> if < 20 ng/ml give ergocalciferol 50,000 I.U. Qweek x 6 weeks STUDIES: Sleep study: Stanford Sleep Clinic (if parasomnia present) Pulmonary Clinic for overnight sleep study at El Camino Hospital Exercise study at LPCH Pediatric Exercise Lab (for assessment of fitness) Indirect calorimetry at LPCH Pulmonary Function Lab (for assessment of resting energy expenditure and daily caloric intake) REFERRALS: (as indicated) Nutrition at 730 Welch Road (Ning Wan, RD) Physical therapy Public health nursing Social work Pediatric Weight Clinic at Castro Commons: BMI ≥ 99th % (morbid obesity) and family is motivated Medically or socially complex patient No improvement after one year of follow-up in Primary Care Clinic Subspecialists: Cardiology – for left ventricular hypertrophy or heart failure Eating disorders clinic – for severely disordered eating ENT – for tonsillar hypertrophy Endocrinology – for diabetes or short stature Genetics – for hypothyroidism or Prader-Willi syndrome Nephrology – for hypertension Ophthalmology – for pseudotumor cerebri Orthopedics – for Blount’s disease or slipped capital femoral epihphysis Pulmonary – for sleep apnea Psychiatry – for depression Child Protective Services: Santa Clara County: 408-299-2071 San Mateo County: 650-595-7922 Criteria: (from Child Obesity and Medical Neglect, Pediatrics January 2009) 1. High likelihood of serious harm from comorbid conditions 2. Reasonable likelihood that coercive state will result in treatment 3. Absence of alternative options EVALUATION AND MANAGEMENT OF COMORBIDITIES DIABETES DYSLIPIDEMIA HYPERTENSION METABOLIC SYNDROME NAFLD PCOS PSEUDOTUMOR CEREBRI DIABETES: Fasting glucose 2 hour GTT Random glucose NORMAL <100 <140 IMPAIRED 100-125 140-199 DIABETES ≥126 ≥200 ≥200 + symptoms Prediabetes = impaired fasting glucose or impaired glucose tolerance Reference: American Diabetes Association Clinical Practice Recommendations 2009 DYSLIPIDEMIA Acceptable Borderline Abnormal Total cholesterol <170 170-199 ≥200 LDL <110 110-129 ≥130 Pharmacologic treatment: children ≥ 8 years old with: Persistent elevation of LDL > 190 after diet therapy, with no other risk factors Persistent elevation of LDL > 160 after diet therapy, with risk factors LDL > 130 in children with diabetes Reference: Pediatrics 2008 Lipid screening and cardiovascular health in children American Heart Association Guidelines: Triglycerides > 150 abnormal HDL < 35 abnormal HYPERTENSION: Blood pressure norms by height and age Blood Pressure Tables for Children The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents (2004) Prehypertension: Hypertension: SBP or DBP 90th to <95th % (or ≥120/80) SBP and/or DBP ≥95th % on 3 or more occasions Prehypertension Stage 1 hypertension Stage 2 hypertension BP 90th to <95th % 95th to 99th % + 5 mm Hg >99th % + 5 mm Hg FOLLOW-UP Recheck in 6 months Recheck in 1-2 weeks Recheck within 1 week DRUG Tx Treat as per Table 6 criteria Treat with meds Evaluation of confirmed hypertension: Labs: BUN, creatinine, electrolytes, UA, UC, CBC Studies: renal ultrasound, echocardiogram (for LVH) For all patients: Therapeutic Lifestyle Change Consider the DASH eating plan: Dietary Approaches to Stop Hypertension “Table 6: Indications for Antihypertensive Drug Therapy in Children” Symptomatic hypertension Secondary hypertension Hypertensive target-organ damage Diabetes (types 1 and 2) Persistent hypertension despite nonpharmacologic measures METABOLIC SYNDROME Key components from 2002 ATP III of the National Cholesterol Education Program: Abdominal obesity Atherogenic dyslipidemia Raised blood pressure Insulin resistance ± glucose intolerance Proinflammatory state Prothrombotic state Promote weight loss and manage individual components NAFLD (Non-alcoholic fatty liver disease) Stages of fatty liver: Steatosis Steatohepatitis (NASH) Fibrosis Cirrhosis Liver failure Screening tests: AST, ALT – [refer to pedi GI if markedly abnormal; repeat in 3 months if mildly abnormal; if still abnormal refer to pedi GI] Liver ultrasound Diagnostic tests: (after referral to Pediatric GI) Liver biopsy Liver MRI Evaluation to exclude other causes of liver disease: Alpha-1-antitrypsin Ceruloplasmin (for Wilson’s disease) Antinuclear antibodies Anti liver, smooth muscle, and kidney antibodies (for autoimmune hepatitis) Hepatitis A, B, and C studies (for viral hepatitis) POLYCYSTIC OVARY SYNDROME Diagnosis by any 2 of the following: Oligomenorrhea or amenorrhea Elevated circulating androgens or clinical signs of androgen excess Polycystic ovaries by ultrasound [ultrasound not necessary in most cases] Laboratory evaluation: LH, FSH, prolactin, DHEAS, androstenedione, SHBG, free and total testosterone Treatment: (apart from weight loss) Oral contraceptives – Adolescent Medicine referral Metformin PSEUDOTUMOR CEREBRI (also known as Idiopathic Intracranial Hypertension) Diagnosis: Symptoms of elevated ICP Normal CT/MRI of the brain Opening pressure of >250 mm in lateral decubitus position Normal CSF composition No other cause of intracranial hypertension Referrals: Ophthalmology Neurology Interventional Radiology (if needed for LP) Treatment: Carbonic anhydrase inhibitors Serial lumbar punctures Ventriculoperitoneal and/or lumboperitoneal shunting Weight loss (including bariatric surgery) PRACTICE GUIDELINES AAP guidelines, December 2007: Expert Committee Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity Academy of Eating Disorders guidelines, February 2009: AED Guidelines for Childhood Obesity Prevention Programs California Medical Association Foundation, 2008: Child and Adolescent Obesity Provider Toolkit Endocrine Society guidelines, December 2008: Prevention and Treatment of Pediatric Obesity National Institute for Children’s Healthcare Quality An Implementation Guide from the Childhood Obesity Action Network PREVENTION AAP OBESITY PREVENTION GUIDELINES: Limit sugar-sweetened beverages Encourage 9 servings per day of fruits and vegetables Eat breakfast daily Limit eating out Encourage family meals Limit portion size Eat a diet rich in calcium and high in fiber with balanced macronutrients Encourage exclusive breastfeeding for 6 months Limit consumption of energy-dense foods Promote moderate to vigorous physical activity ≥ 60 minutes per day Limit screen time to a maximum of 2 hours per day Parent handouts: Ounce of Prevention (from the state of Ohio and Nationwide Children’s Hospital) TREATMENT AAP STAGES OF OBESITY TREATMENT OTHER TREATMENT RESOURCES: Motivational interviewing Eating and activity plans Community resources GROUP TREATMENT PROGRAMS WEIGHT LOSS MEDICATION BARIATRIC SURGERY AAP STAGES OF OBESITY TREATMENT: Stage 1: Stage 2: Stage 3: Stage 4: Prevention Plus (PP) Structured Weight Management (SWM) Comprehensive Multidisciplinary Intervention (CMI) Tertiary Care Intervention (TCI) BMI 85th-94th % + risk 95th-99th % >99th % Age 2-5 years PP up to SWM PP up to CMI PP up to CMI Age 6-11 years PP up to SWM PP up to CMI PP, SWM, or CMI up to TCI Age 12-18 years PP up to SWM PP up to TCI PP, SWM, or CMI up to TCI STAGE 1: PREVENTION PLUS •Goal = weight maintenance to improve BMI •Tailor follow-up to individual families •If no improvement in BMI after 3 to 6 months advance to stage 2 Key points: ≥ 5 servings of fruits and vegetables per day Minimize sugar-sweetened beverages (no more than 1 serving per day) Decrease television to ≤ 2 hours per day Be physically active ≥ 1 hour per day Prepare more meals at home Eat at the table as a family 5 to 6 times per week Eat a healthy breakfast every day Involve the whole family in lifestyle changes Allow the child to self regulate meals and avoid over-restriction Tailor recommendations to cultural values STAGE 2: STRUCTURED WEIGHT MANAGEMENT •Target diet and physical activity behaviors more intensively •Goal = weight maintenance, but weight loss should not exceed 1 lb/month in children 2 to 11 years old or 2 lb/week in older children Follow up monthly •If no improvement in BMI after 3 to 6 months advance to stage 3 Key points: Planned diet with balanced macronutrients emphasizing low energy-density foods Structured daily meals and snacks Reduce television and other screen time to ≤ 1 hour per day Planned activity 60 minutes per day Use of logs to monitor behavior Provide reinforcement for achieving targeted behaviors STAGE 3: COMPREHENSIVE MULTIDISCIPLINARY INTERVENTION •Refer to a multidisciplinary obesity care team (including a behavioral counselor, dietitian, and exercise specialist) for a structured behavioral modification program •Goal = weight maintenance or gradual weight loss until BMI < 85%; weight loss should not exceed 1 lb/month in children 2 to 5 years old or 2 lbs/week in older children Key points: Goal setting and contingency management Negative energy balance Parental participation for children < 12 years old Systematic evaluation of body measurements, diet, and activity Frequent visits up to weekly for 8 to 12 weeks and then monthly STAGE 4: TERTIARY CARE •Refer to a pediatric tertiary care weight management center with treatment to include diet, medication, and /or surgery WEIGHT GOALS (adapted from the AAP 2007 guidelines) BMI 85th-94th% 95th-98th% 2-5 years old WM or WG WM ≥99th% WL of ≤ 1 pound per month (with BMI ≥ 21) 6-11 years old WM Gradual WL of 1 pound per month WL of ≤ 2 pounds per week WM = weight maintenance WG = weight gain WL = weight loss OTHER TREATMENT RESOURCES MOTIVATIONAL INTERVIEWING (Miller and Rolnick) Express empathy Develop discrepancy Roll with resistance 12-18 years old WM or gradual WL WL of ≤ 2 pounds per week WL of ≤ 2 pounds per week Support self-efficacy Avoid argumentation EATING AND ACTIVITY PLANS: •MyPyramid.gov dietary plan based on age and activity level •Plate Method: American Diabetes Association - Create Your Plate •Glycemic index •5210 (from Maine Medical Center): 5 or more servings of fruits and vegetables per day 2 hours or less of recreational screen time per day 1 hour or more of physical activity per day 0 sugary drinks 2008 HHS Physical Activity Guidelines for Americans Key targets: Aerobic activity (running, swimming, dancing, cycling, etc.) Muscle-strengthening activity (climbing, playing tug-of-war, lifting weights, etc.) Bone-strengthening activity (running, jumproping, basketball, etc.) Recommendation: 60 minutes or more of physical activity daily Mostly moderate or vigorous intensity aerobic activity with vigorous activity ≥ 3 days per week Muscle-strengthening activity at least 3 days per week Bone-strengthening activity at least 3 days per week Parent handouts: Checklists for 2-7 years old, 8-12 years old, and teens in English and Spanish (source: Dan Delgado, MD on the AAP California Chapter 1 website) Beverages - Sugary drinks and childhood obesity Food labels - Read It Before You Eat It High fiber diet - Fiber and Your Child Organic Essentials pocket guide from the Organic Center Serving size - What size is your serving? Vegetarian diet - Vegetarianism http://www.fitness.gov/kidstips.pdf -> general handout targeted for kids http://www.nutritionexplorations.org/pdf/educators/Healthier_eating.pdf -> handout for parents discussing how to eat from the food groups http://www.fns.usda.gov/tn/resources/nibbles/readit_poster.pdf -> easy handout on how to read basics of a nutrition label using the 5/20% rule http://www.nal.usda.gov/wicworks/Sharing_Center/MO/Lets_Eat_Out.pdf -> tips on making healthier choices at fast food restaurants, also available in spanishhttp://www.nal.usda.gov/wicworks/Sharing_Center/MO/Lets_Eat_Outsp.pdf http://www.nche.org/2003TheKidsActivityPyramid.pdf -> colorful activity pyramid for kids with ideas on how to get moving http://www.dshs.state.tx.us/wichd/nut/pdf/NR00015.pdf -> handout on portion sizes for both young children & adults in English and Spanish, pages 7 and 8 COMMUNITY RESOURCES: Boys and Girls Club East Palo Alto activity guide: www.epaguide.org Farmers markets Gardening ---> Collective Roots Running ---> Girls on the Run YMCA East Palo Alto Sequoia-Redwood City (Fit Families Program) GROUP TREAMENT PROGRAMS: Packard Pediatric Weight Control Program 650-725-4244 Kids 8 to 12 and 13 to 15 years old Weekly meetings over 6 months for parents and kids SHAPEDOWN TOPS = Taking Off Pounds Sensibly Weight Watchers Parent handout: Weight Management Resources for Kids and Teens PDF WEIGHT LOSS MEDICATION: (FDA-approved) •Orlistat(Xenical, Alli) ≥ 12 years old •Sibutramine (Meridia) ≥ 16 years old BARIATRIC SURGERY: LPCH Adolescent Bariatric Surgery Program Refer to Weight Clinic at Castro Commons Criteria: Completion of growth (generally ≥ 13 years in girls and ≥ 15 years in boys) BMI ≥ 35 with major comorbidities of obesity BMI ≥ 40 with lesser comorbidities of obesity For further reference see: 2004 report in Pediatrics by Inge, et al: Bariatric Surgery for Severely Overweight Adolescents: Concerns and Recommendations 2009 report in Obesity by Pratt, et al: Best Practice Updates for Pediatric/Adolescent Weight Loss Surgery WES 11/09