C7 UHW Student Information Pack
advertisement

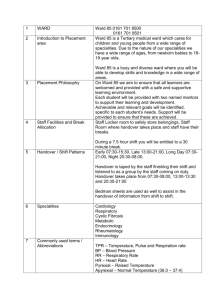
University Hospital of Wales Ward C7 Medicine FRaME/Endocrine (Focused Rehabilitaion and Medical Evaluation) Student Orientation pack Name………………………………………………… Mentor…………………………………………….. 02/09 An Introduction Welcome to C7. We hope your placement with us will not only be an enjoyable and exciting one, but one in which you gain an insight into the nursing care and management of patients with a range of medical conditions. On C7 we work 12 ½ hour shifts 7-7.30 days and nights. As we get a paid half hour break each day we are required to pay back the 1.5 hrs we owe each week, therefore staff work a 6hr shift every 4 weeks. During your placement you will be allocated a mentor who will work with you, supervising and providing guidance and support throughout your stay. On C7 we have a multi disciplinary approach in providing individualised care to the patient and their family. The ward C7 has two distinct purposes: C7 North is: FRaME. (Focussed Rehab and Medical Evaluation) ward. 19 beds male and female This booklet provides you with an overview of the ward area and the patients we care for on the ward. During your allocation on C7 you will be allocated a mentor and co mentor, who will work alongside you, supervising and offering you guidance and support during your stay with us. FRaME – originally based on B6N, was a new ward which opened in October of 2008 as part of the Cardiff and Vale NHS Trust bed capacity plan. The aim was to open more medical beds within the Trust thereby placing medical patients on appropriate wards and not as outliers in other specialities such as general surgery. The ward consists of 19 beds male and female C7 FRaME consultants are: DR Biju Mohamed Dr Karl Davis along with an SHO and Registrar working within the area. Both Dr Mohamed and Dr Davis cover the ward at the same time. Dr Mohameds patients are located in the 9 bedder, with Dr Davis’s in the sides. C7 South is General medicine with an endocrine speciality. The patients on this end of the ward can be very varied and can include endocrine inpatients. The south end of the ward is where the regional Endocrine investigation unit is based. The endocrine specialist nurses see out patients on a daily basis. C7 Endocrine consultants are: Dr Steve Davies Dr Aled Reed Professor Colin Dayan The three consultants cover the ward on a rolling one month programme. Along with a full medical team of an F1 (foundation year) doctor An F2 (SHO) and a specialist registrar. Nursing team: Ward Sister: Deputy Ward Sister: Sharon Irving Liz Vaughan Our Nursing Philosophy of Care is: We aim to treat every patient as an individual, providing evidence based care of the highest standard by skilled staff within a multi -disciplinary team (MDT), thus ensuring that each patient receives care appropriate to their individual needs until they are medically fit and suitable for discharge. All efforts are made to ensure the patient is sufficiently prepared for their return home, and relatives are involved with the MDT in the preparation for their discharge. Despite all the attempts of the multi disciplinary team this can sometimes be a lengthy process and relatives can be assured that we make every effort where possible to speed up this process. Our patients can be assured that confidentiality and their rights will be recognised and respected by all staff involved in their care regardless of their age, disability, race, religion or gender. Skills list for students Ward C7 offers the student the opportunity to learn and improve many clinical nursing skills. Here are some areas students may wish to focus on: • Admission and discharge of patients: policies and practice • Referral to other services – referral criteria and processes, e.g. Social workers, physiotherapy, occupational therapy etc • Care of the acutely unwell • Management of long term medical conditions • Multidisciplinary care of the medical patient • Management roles, resources, decision making processes, essence of care and other benchmarking processes Transferable Skills for students • Use of NEWS scoring , and when to inform Medical Rapid Response Team for intervention/ assessment - measurement and recording of observations including blood pressure, pulse, oxygen saturations, temperature and respirations and how to interpret findings. • You will learn about aseptic technique including catheterisation and wound care. • You will be involved with drug administration (orally, inhalation, subcutaneous, intramuscular and suppositories). • Nutritional and tissue viability assessment including pressure area management. • Blood glucose testing and recording. • The preparation and administration of insulin. • Admission and Discharge/Transfer procedure. • General hygiene, oral care, nutrition and hydration. • Administration of oxygen and use of nebuliser therapy. • Managing and preventing risk. • Documentation. • Patient assessment. Within 24 hours of admission, a patient should have had the Activities of Daily Living assessment and a property disclaimer completed in the admission booklet. The following risk assessments need to be completed: Waterlow risk assessment (within 6 hours of admission, Nutritional risk assessment (including weight recorded), Pat-e-bac assessment, Falls risk assessment. Once completed, these assessments should highlight the need, if any for further intervention, for example, Airwave/Repose mattress, referral to physiotherapy, commencing a food chart, cot sides, crash mats etc. These risk assessment scores should be recorded on the daily charts for quick reference. Opportunities There will also be opportunities for students to work with other members of the multidisciplinary team. For example: Some of the procedures and investigations you may be able to observe include: • • • • • • • • • • • • • • • Routine blood tests Arterial blood gases CT, MRI and Ultrasound scans Blood sugar monitoring ECGs Catheter insertion Lumbar punctures Urine testing Wound cultures VQ scans OGD Physiotherapy treatments OT washing and dressing assessments / Home Visits Speech and language assessments Dietetic screening Daily Routine Remember, no day is the same as we care for a variety of different patients with varying individual needs! Times are as a rough guide only! 7am Handover The start of a shift begins with ‘handover’ or ‘report’ of patient information, this promotes continuity of care and allows staff to review and plan care. Patients are discussed with the nurse and health care support worker looking after that group of patients. Two qualified nurses will share out the patients, (usually the 9 bedded bay or the side bays) with the third qualified nurse assisting with all areas as required. The health care support workers will work in all areas of the ward. The nurse in charge of the shift should also be made aware of any potential discharges and any patients that are particularly unwell to ensure that they are adequately supported. You will receive a printed document, detailing the patients on the ward. At the end of the shift, the report must be disposed of in confidential waste (envelope situated on the nurses station). 7.30 – 12 noon Patients to be sat up ready for breakfast Breakfast/tea round – served by ward caterers, patients to be assisted as required Medication round, including ordering new medications from pharmacy Washes, pressure area checks and bed making Restocking of the linen trolley Incontinence care and toileting, as required Observations Blood sugar monitoring prior to lunch Morning breaks to start at 10am – 30 minutes 1200 Midday Lunch and tea round – served by ward caterers, patients to be assisted as required Medication round and updating of daily recording charts Update food charts Afternoon Doctors' rounds/Physio/OT interventions, visits from specialist nurses Handover to afternoon staff, if applicable Dressings Relevant referrals made and discharge planning, Incontinence care and toileting, as required Pressure area checks General tidy (clean down tables, wash medicine pots, commode cleaning etc) Checking of oxygen and suction units – each bed side unit should have a yanker sucker, green oxygen tubing and a non-re-breather mask. Equipment re-stocking and ordering of equipment (e.g. bottles/bedpans, pads, blood sugar monitoring equipment, thermometer covers... the list is endless!) Documentation – including notes and monitoring/completing risk assessments Blood sugar monitoring prior to tea Afternoon breaks to start at 1500 – 20 minutes 1700 hours Evening meal and tea round- served by ward caterers, patients to be assisted as required Update food record charts Medication round Update handover sheet on the computer ready for night staff Incontinence care and toileting, as required Pressure area checks Tidy ward 1900 hours Handover to night staff General clean and tidy up, removing potential hazards e.g. relatives chairs, rubbish, linen bags etc 2000 hours Settle and make patients comfortable for the night Observations Pressure area checks Incontinence care and toileting, as required Update/Add up fluid balance charts Empty catheters Attend to patient needs as required Medication round Other Information Referral Criteria/ Admission methods Patients are admitted to C& from A&E, MAU, A1 & A4 Short stay wards and sometimes other ward areas. Visiting Times 2-4 6-8pm. This is to ensure that patients are not disturbed at meal times. Useful Telephone Numbers Ward number – Reception 42181 North 43759 South 43760 Cardiac Arrest - 2222 Switchboard - 100 To use the Hospital Bleep System dial 181 then the person's bleep number that you need to contact, then the extension number of the phone you’re using followed by #. What you can expect from us • • • • • • • • You will receive an induction into your work area to ensure you are familiar with the environment and are able to practice safely. You must find out the location of the arrest trolley, portable oxygen and fire extinguishers and exits on your first day. You will discuss your learning needs and outcomes at the beginning of the placement. We will provide an environment conducive to meeting identified individual student learning needs which are also safe and healthy. During your placement you will be allocated a mentor to work alongside. The mentor will be a qualified practitioner who will assist and support you during your clinical work (at least 50% of your rota will be allocated alongside your mentors). Your mentor will assess your performance against your course learning outcomes, and provide feedback to help you develop your skills. You will receive supervision during your clinical practice. You will be a valued member of the multidisciplinary team during your placement, and can expect support from all your colleagues. We will listen to your feedback about your placement and will respond to any issues raised sensitively. What we expect from you • • • • • • • We expect you to arrive on time for planned shifts and any other activity identified by the Mentor or delegated supervisor We expect you to ensure your Mentor is aware of your learning outcomes for the placement and specific learning needs We expect you to act in a professional manner. We expect you to dress in accordance with your University’s uniform policy, and also in accordance with the Cardiff and Vale NHS Trust uniform policy (no jewellery apart from stud earrings and wedding ring if applicable). You should inform your mentor or delegated person if you are unwell and not able to attend your placement. Please do this as soon as possible prior to your shift. You should also inform the University, as per guidelines. We expect you to maintain and respect confidentiality and patient dignity at all times. This applies to clients, their records and discussions between the student and the Mentor. We would like you to raise any issues regarding your placement with your mentor. If this is not possible please speak to the deputy or Ward Manager otherwise you should contact your link tutor / placement co-ordinator. Induction Checklist 1. INTRODUCTION TO THE WORKPLACE TO BE COVERED ON DAY ONE OF THE PLACEMENT Introduction to other members of staff □ Allocation of mentor and key supervisors’ □ Brief tour of ward, department or work area, toilets, rest room, □ Restaurant, car parking etc □ Fire exits, alarms, and equipment and fire evacuation procedures and emergency procedures□ How to report accidents to yourself, others or near miss □ Health and safety including infection control measures, □ Food hygiene, chemicals and physical hazards in the workplace □ Local arrangements for safe lifting and handling including equipment □ Telephone and bleeps – use and location □ Safe keeping of property – for staff and patients □ Confidentiality – personal and access to patient records etc □ 2. TRUST AND LOCAL POLICIES AND PROCEDURES Location of and access to reference books, policies and standards: □ Risk Control Policies and Procedures Manual □ Accident Reporting □ Health and Safety □ Infection Control □ Needle Stick Injuries □ Fire Regulations and Procedures □ Confidentiality/Data Protection Act/Security of Information □ Human Resources e.g. Equality and Diversity/Disability/Bullying and Harassment, Whistle blowing, disciplinary and grievance etc □ 3. PLACEMENT RESPONSIBILITIES Hours of work including shift work, flexi-time arrangements □ Reporting sickness absence and other absence □ Outline of duties and supervision □ Performance standards □ 4. TRAINING NEEDS IDENTIFIED AND ACTIONS Learning Outcomes for placement discussed □ Specific learning needs discussed □ Learning Resources available discussed □ I confirm that a local induction has been completed and all the topics have been discussed and understood. Student :_____________________Mentor:________________________