פירות שיח אברהם נגד תסמונת קדם ווסתית
advertisement
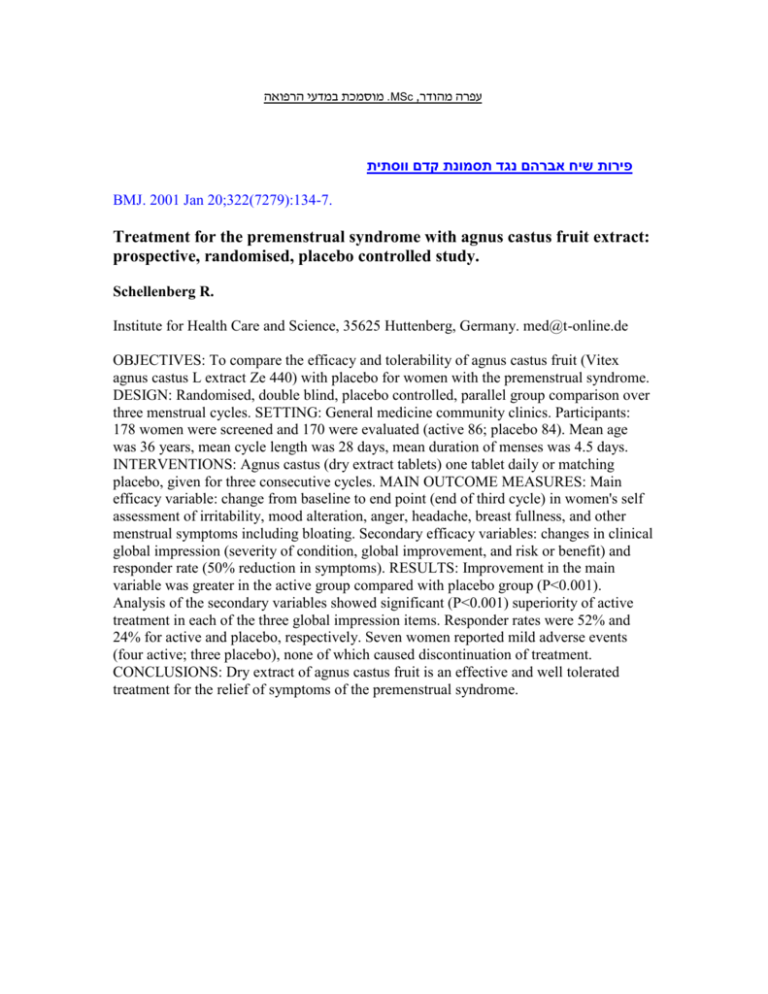
מוסמכת במדעי הרפואה.MSc ,עפרה מהודר פירות שיח אברהם נגד תסמונת קדם ווסתית BMJ. 2001 Jan 20;322(7279):134-7. Treatment for the premenstrual syndrome with agnus castus fruit extract: prospective, randomised, placebo controlled study. Schellenberg R. Institute for Health Care and Science, 35625 Huttenberg, Germany. med@t-online.de OBJECTIVES: To compare the efficacy and tolerability of agnus castus fruit (Vitex agnus castus L extract Ze 440) with placebo for women with the premenstrual syndrome. DESIGN: Randomised, double blind, placebo controlled, parallel group comparison over three menstrual cycles. SETTING: General medicine community clinics. Participants: 178 women were screened and 170 were evaluated (active 86; placebo 84). Mean age was 36 years, mean cycle length was 28 days, mean duration of menses was 4.5 days. INTERVENTIONS: Agnus castus (dry extract tablets) one tablet daily or matching placebo, given for three consecutive cycles. MAIN OUTCOME MEASURES: Main efficacy variable: change from baseline to end point (end of third cycle) in women's self assessment of irritability, mood alteration, anger, headache, breast fullness, and other menstrual symptoms including bloating. Secondary efficacy variables: changes in clinical global impression (severity of condition, global improvement, and risk or benefit) and responder rate (50% reduction in symptoms). RESULTS: Improvement in the main variable was greater in the active group compared with placebo group (P<0.001). Analysis of the secondary variables showed significant (P<0.001) superiority of active treatment in each of the three global impression items. Responder rates were 52% and 24% for active and placebo, respectively. Seven women reported mild adverse events (four active; three placebo), none of which caused discontinuation of treatment. CONCLUSIONS: Dry extract of agnus castus fruit is an effective and well tolerated treatment for the relief of symptoms of the premenstrual syndrome. מוסמכת במדעי הרפואה.MSc ,עפרה מהודר רפואה סינית נגד בחילות בהריון J Reprod Med. 2001 Sep;46(9):835-9. Effect of acupressure on nausea and vomiting during pregnancy. A randomized, placebo-controlled, pilot study. Werntoft E, Dykes AK. Department of Nursing, Unit of Caring Sciences, Lund University, Lund, Sweden. elisabet.werntoft@omv.lu.se OBJECTIVE: To compare the antiemetic effect of acupressure at the Neiguan point (P6) in a group of healthy women with normal pregnancy and nausea and vomiting during pregnancy (NVP) with a similar group receiving acupressure at a placebo point and another, similar group not receiving any treatment. STUDY DESIGN: A randomized, placebo-controlled, pilot study involving 60 women. RESULTS: It is possible to reduce NVP significantly with acupressure at P6 as compared to acupressure at a placebo point or no treatment at all in healthy women with normal pregnancies. Relief from nausea appeared one day after starting treatment in both the P6 and placebo groups but lasted for only six days in the placebo group. The P6 group, however, experienced significantly less nausea after 14 days as compared to the other two groups. CONCLUSION: This study involved 60 healthy women with normal pregnancy and suffering from NVP. According to the results, in healthy women with normal pregnancy it is possible to reduce NVP significantly at P6 as compared to acupressure at a placebo point and to no treatment. מוסמכת במדעי הרפואה.MSc ,עפרה מהודר דיקור למניעת מיגרנות Headache. 2002 Oct;42(9):855-61. Acupuncture in the prophylactic treatment of migraine without aura: a comparison with flunarizine. Allais G, De Lorenzo C, Quirico PE, Airola G, Tolardo G, Mana O, Benedetto C. Woman's Headache Center, Department of Gynecology and Obstetrics, University of Turin, Turin, Italy. OBJECTIVES: In a randomized controlled trial extending over 6 months, we evaluated the effectiveness of acupuncture versus flunarizine in the prophylactic treatment of migraine without aura. METHODS: One hundred sixty women with migraines were randomly assigned to acupuncture treatment (group A, n = 80) or to an oral therapy with flunarizine (group F, n = 80). In group A, acupuncture was carried out in weekly sessions for the first 2 months and then once a month for the next 4 months. The same acupoints were used at each treatment: LR3 Taichong, SP6 Sanyinjiao, ST36 Zusanli, CV12 Zhongwan, LI4 Hegu, PC6 Neiguan, GB20 Fengchi, GB14 Yangbai, EX-HN5 Taiyang, GV20 Baihui. In group F, 10 mg flunarizine were given daily for the first 2 months and then for 20 days per month for the next 4 months. RESULTS: The frequency of attacks and use of symptomatic drugs significantly decreased during treatment in both groups. The number of attacks after 2 and 4 months of therapy was significantly lower in group A than in group F, and analgesic consumption was significantly lower in group A at 2 months of treatment. At 6 months no such differences existed between the two treatment groups. Pain intensity was significantly reduced only by acupuncture treatment. Side effects were significantly less frequent in group A. CONCLUSIONS: Acupuncture proved to be adequate for migraine prophylaxis. Relative to flunarizine, acupuncture treatment exhibited greater effectiveness in the first months of therapy and superior tolerability.