Supplemental Methods
advertisement

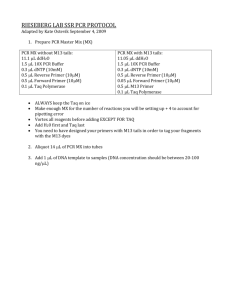
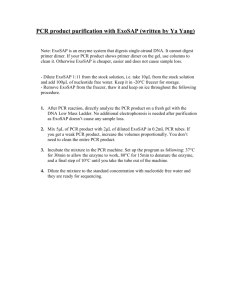
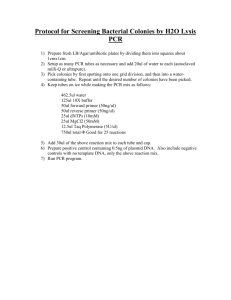
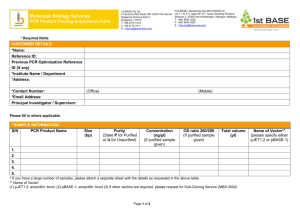
Supplemental Methods Tissue specimens and matched normal blood were obtained at the time of surgery, snap frozen and stored at -70 ºC. DNAs were prepared using standard procedures. For all tumors, H & E stained sections were evaluated to identify tissues will neoplastic cellularity of >66% that were then used for DNA preparation. Normal (non-neoplastic DNA) was prepared from peripheral blood leukocytes for the majority of cases, or when blood was not available, from normal uninvolved myometrium. Microsatellite analysis was performed as previously described (Kowalski et al. 1997) using five National Cancer Institute consensus microsatellite markers (BAT25, BAT26, D2S123, D5S346 and D17S250) (Boland et al. 1998). Tumors were designated as having high-level MSI (MSI+) if novel PCR bands were identified in at least two of the five consensus panel markers. Tumors were considered microsatellite stable if there was no evidence of MSI in any marker. PCR primer sequences were M13 tailed and sequences are available by request from the author. PCR reactions were purified after thermocycling using solid phase reversible immobilization (SPRI)-based technology (AMPure®; Agencourt Biosciences Corp., Beverly, MA), resulting in the removal of unincorporated dNTPs, primers, and salts. PCR products were eluted in 30l distilled H2O. Both strands of each PCR product were sequenced as follows: Sequencing reactions were performed using 3l (approximately 25ng) of purified PCR product in a 6l reaction containing 0.33l BigDye Terminator v3.1 premix, 3.2 pmol of either M13 forward (TGTAAAACGACGGCCAGT) or M13 reverse (CAGGAAACAGCTATGACC) primer, and 1.03l 5X BigDye sequencing buffer. Cycle-sequencing was performed for 35 cycles following the manufacturers recommendations on GeneAmp 9700 PCR machines (Applied Biosystems, Foster City, CA). Sequencing reactions were purified using CleanSEQ® (Agencourt Biosciences Corp., Beverly, MA) to remove unincorporated dye-terminators, and analyzed on 3730xl DNA analyzers (Applied Biosystems, Foster City, CA). Sequences were analyzed using Sequencher (Gene Codes). All mutations were absent in the corresponding normal DNA demonstrating they arose somatically and all mutations were confirmed in a second independent PCR. It should be noted that the A315T reported in ESS-1 derived from an endometrial stromal sarcoma occurred in the mesenchymally expressed isoform (FGFR2c) and all carcinosarcomas (tumors with both malignant epithelial and stromal elements) were also screened for mutations in exon 9 (NM_000141). 1. Kowalski LD, Mutch DG, Herzog TJ, et al: Mutational analysis of MLH1 and MSH2 in 25 prospectively-acquired RER+ endometrial cancers. Genes Chromosomes Cancer 18:219-227, 1997 2. Boland CR, Thibodeau SN, Hamilton SR, et al: A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res 58:5248-5257, 1998