How to help patients with restless legs
syndrome
Discerning the indescribable and relaxing the restless
Virgilio Gerald H. Evidente, MD Charles H. Adler, MD, PhD
VOL 105 / NO 3 / MARCH 1999 / POSTGRADUATE MEDICINE
CME learning objectives
To familiarize primary care physicians with diagnostic criteria for restless legs syndrome
To elucidate secondary, and often curable, causes of restless legs syndrome
To describe current treatment options for restless legs syndrome
This page is best viewed with a browser that supports tables
Preview: Few conditions are characterized by the difficulty encountered in trying to depict their symptoms,
but such is the case in restless legs syndrome. Patients report sensations that are not painful yet are distinctly
bothersome and can lead to significant physical and emotional disability. Once correctly diagnosed, restless
legs syndrome can usually be effectively treated symptomatically, and in some secondary cases, it can even
be cured. In this article, the authors focus on clinical features that enable timely identification of the
condition and on current management strategies.
In the mid-1940s, Swedish neurologist Karl A. Ekbom described a disorder characterized by sensory
symptoms and motor disturbance of the limbs, mainly during rest. He named the condition restless legs
syndrome (1). Although the syndrome affects about 10% to 15% of the US population (2), it is often
unrecognized and misdiagnosed. It may begin at any age (1-3), even as early as infancy, but most patients
who are severely affected are middle-aged or older. Symptoms progress over time in about two thirds of
patients and may be severe enough to be disabling.
Diagnostic criteria and common features
In 1995, the newly formed International Restless Legs Syndrome Study Group developed criteria for
diagnosing restless legs syndrome (3). Four basic elements must be present to make the diagnosis: (1) a
desire to move the limbs, often associated with paresthesia or dysesthesia, (2) symptoms exacerbated by rest
and relieved by activity, (3) motor restlessness, and (4) nocturnal worsening of symptoms. These and several
additional features commonly seen in restless legs syndrome are discussed in the following paragraphs.
Desire to move the limbs, paresthesia, dysesthesia. Patients often describe an unpleasant sensation
in the calves and occasionally in the thighs, feet, or upper limbs. Although the study group refers to
dysesthesia or paresthesia (which implies abnormal sensations) (3), most patients simply relate
vague, nonpainful, indescribable, bilateral (rarely unilateral) discomfort in the limbs, using such
terms as crawling, creeping, tingling, burning, itching, and aching.
Symptoms are similar to those described by patients with akathisia (which is usually caused by use
of neuroleptic drugs). However, in contrast to patients with restless legs syndrome, those with
akathisia have an inner feeling of restlessness, gain the most relief by resting in a recumbent
position, and do not experience paresthesia or nocturnal worsening of symptoms.
Symptoms exacerbated by rest, relieved by activity. The unpleasant limb sensations of restless legs
syndrome are precipitated by rest or inactivity (eg, lying in bed at night, riding in a car or airplane,
sitting in a theater). The discomfort is usually relieved by motor activity (eg, moving the legs,
walking).
Motor restlessness. Patients describe a buildup of discomfort and involuntary limb jerking if they
remain still. There is an urge to move the legs and relief after moving (much like the sensation of
tics). Compelling motor restlessness can manifest as tossing and turning in bed, needing to pace the
floor, stretching or shaking the legs, or needing to exercise (3). Limb movements in restless legs
syndrome are partly voluntary, in that patients choose to move to relieve the discomfort, and partly
involuntary, since patients are compelled to move. Such partly voluntary, partly involuntary
movements are sometimes referred to as "unvoluntary" or "semivoluntary."
Nocturnal worsening of symptoms. All patients notice worsening of symptoms at night (usually as
they lie in bed before sleep or when they are awakened in the middle of the night) and improvement early in the morning. Nocturnal worsening is caused by lack of motor activity at night and is
also thought to be due to an independent circadian rhythm (3). In severe cases, patients experience
symptoms both day and night.
Periodic limb movements of sleep. About 80% of patients with restless legs syndrome have
unilateral or bilateral periodic limb movements of sleep, also called nocturnal myoclonus (1,3).
These movements are stereotyped, repetitive, slow flexion of the limbs (legs alone or legs more
than arms) during stage 1 or 2 sleep. They occur semirhythmically at intervals of 5 to 60 seconds
and last about 1.5 to 2.5 seconds. In the lower limbs, repetitive dorsiflexion of the big toe with
fanning of the small toes is seen, along with flexion of the ankles, knees, and thighs.
Dyskinesias while awake. These motions, also called periodic limb movements while awake, are
seen in 30% to 50% of patients with restless legs syndrome (3). They are similar to periodic limb
movements of sleep but occur only during wakefulness. They can be fast or slow and periodic or
nonperiodic.
Sleep disturbance. Because of limb discomfort and jerking, most patients with restless legs
syndrome have disturbances of sleep onset or maintenance (1,3). The result is excessive daytime
sleepiness and fatigability, although not to the same degree as that caused by narcolepsy.
Primary disease
In most cases, restless legs syndrome is idiopathic. Such idiopathic disease can be familial (in 25% to 75%
of cases) and, if so, is transmitted in an autosomal-dominant fashion (1,3,4). Progressive decrease in age at
onset with subsequent generations (ie, genetic anticipation) has been described in some families. Patients
with familial restless legs syndrome tend to have an earlier age at onset and slower progression (5).
Secondary disease
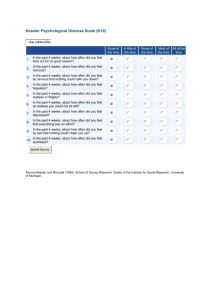
Restless legs syndrome can develop as a result of certain conditions or factors (table 1), particularly iron
deficiency and peripheral neuropathy (6-12). These two conditions should be ruled out on clinical grounds
before restless legs syndrome is labeled primary (13). Because of the prevalence of these conditions in the
general population, their association with restless legs syndrome needs to be interpreted with considerable
caution.
Table 1. Factors and conditions that may contribute to secondary restless legs syndrome (in order of
frequency)
Deficiency of iron, folate, or magnesium
Polyneuropathy caused by alcohol abuse, amyloidosis, diabetes mellitus, idiopathic polyneuropathy,
lumbosacral radiculopathy, Lyme disease, monoclonal gammopathy of undetermined significance,
rheumatoid arthritis, Sjögren's syndrome, uremia, or vitamin B12 deficiency
Pregnancy
Anemia
Parkinson's disease
Gastric surgery
Chronic obstructive pulmonary disease
Carcinoma
Chronic venous insufficiency or varicose veins
Intake of certain substances or drugs: alcohol, caffeine, anticonvulsants (eg, methsuximide [Celontin
Kapseals], phenytoin [Dilantin]), antidepressants (eg, amitriptyline HCl [Elavil], paroxetine HCl [Paxil]),
beta blockers, histamine2 antagonists, lithium, neuroleptics
Withdrawal from vasodilators, sedatives, or imipramine HCl (Tofranil)
Cigarette smoking
Myelopathy or myelitis
Hypothyroidism or hyperthyroidism
Acute intermittent porphyria
Fibromyalgia syndrome
Arborizing telangiectasia of the lower limbs
Peripheral microemboli made of cholesterol
Restless legs syndrome can be the initial manifestation of iron deficiency (1,14). A low serum ferritin level
may precede a drop in serum iron level. Depletion of iron stores, in the absence of overt iron deficiency, can
lead to restless legs syndrome. How this occurs in unknown. Treatment with ferrous sulfate may bring
improvement.
About 5% of patients with sensory neuropathy (especially caused by uremia, rheumatoid arthritis, and
diabetes) have restless legs syndrome (8). Treatment of the polyneuropathy may improve symptoms.
Diagnosis
Diagnosis of restless legs syndrome is founded mainly on clinical history. If a secondary cause is suspected
on the basis of history, abnormal findings on neurologic examination, or poor response to treatment, a
laboratory workup should be done. Testing should measure levels of blood urea nitrogen, creatinine, fasting
blood glucose, ferritin, magnesium, thyrotropin, and folate and should include a glucose tolerance test and a
complete blood cell count.
Needle electromyography and nerve-conduction studies should be considered if polyneuropathy is suspected
on clinical grounds, even if results of neurologic examination are apparently normal (13). Polysomnography
is rarely necessary but may be used to quantify periodic limb movements of sleep or to characterize sleep
architecture, especially in patients who continue to have significant sleep disturbance despite relief of
sensory symptoms with treatment.
Nonpharmacologic management
Patients with suspected restless legs syndrome who are sensitive to caffeine, alcohol, or nicotine should
avoid these substances (1,6). Offending medications (table 1) also should be discontinued. In general,
physical measures are only partially or temporarily helpful. Some patients benefit from hot or cold baths,
whirlpool baths, rubbing of the limbs, or vibratory or electrical stimulation of the feet and toes before
bedtime.
Supplementation to correct deficiencies in vitamins (eg, folate) (15), electrolytes (eg, magnesium) (7), or
iron may improve symptoms. Patients with prominent varicose veins in the legs may benefit from use of
sclerosing agents (9). Those with uremia may have relief after kidney transplantation or correction of anemia
with erythropoietin (Epogen, Procrit) (6).
Pharmacologic management
Drug therapy for primary restless legs syndrome is largely symptomatic, since cure is only possible in
secondary disease. Medications should be initiated at a low dose and be taken an hour or two before bedtime
to allow sufficient absorption and onset of action. Additional doses can be taken if symptoms cause
awakening in the middle of the night. If tolerance to one drug develops, another class of drugs may be
substituted. Monthly rotation of two or three agents found to be effective may help prevent tolerance. A
combination of drugs may be beneficial in severe cases.
Levodopa with carbidopa
Levodopa with carbidopa (Sinemet) can improve sensory symptoms and periodic limb movements of sleep
in primary restless legs syndrome and that associated with uremia (1-3,16). For symptoms that start before
sleep, one 25/100-mg carbidopa/levodopa tablet can be taken 1 to 2 hours before bedtime. If symptoms
occur during the night, one 25/100-mg controlled-release carbidopa/levodopa (Sinemet CR) tablet can be
used. In patients who have symptoms both before sleep and during the night, a combination of short-acting
and controlled-release tablets can be given. Most patients experience benefits when the levodopa portion of
carbidopa/levodopa totals 100 to 500 mg daily, although some may need 1,000 to 1,500 mg. Nausea and
constipation are the most common side effects of levodopa.
The major drawback in prescribing levodopa for restless legs syndrome is that in about 80% of patients,
augmentation of symptoms occurs as early as a few months after initiation of therapy (17). It can manifest as
earlier onset during the evening or after assuming a restful position, as increased intensity in the morning (ie,
rebound), or as extension of symptoms to the upper body. Augmentation is more likely in patients with
severe pretreatment symptoms and in those taking 200 mg or more of levodopa daily. If augmentation or
rebound develops, adjunctive therapy with reduction of the levodopa dose or discontinuation of levodopa
and substitution of another drug may help.
Dopamine agonists
Dopamine agonists are less likely to produce augmentation or rebound and can be useful alone or along with
levodopa in patients in whom one of these conditions develops (2,17,18). Side effects of dopamine agonists
include nausea, light-headedness, drowsiness, and postural hypotension.
Pergolide mesylate (Permax) is a potent, long-acting dopamine D1 and D2 receptor agonist that has been
shown to be effective in restless legs syndrome (1-3,16), even in patients who are unresponsive to levodopa
(18). The dose is 0.05 mg before bedtime initially, and it can be increased by 0.05 mg every 3 to 5 days until
relief is obtained or side effects develop. The usual effective daily total is 0.1 to 0.75 mg, given in divided
doses; some patients may need up to 1.5 mg.
Bromocriptine mesylate (Parlodel), a dopamine D2 receptor agonist, also has been found to be effective in
restless legs syndrome (1-3,18). Bromocriptine can be started at a dose of 1.25 mg at bedtime and increased
by 1.25 mg every few days until benefits or side effects are noted. The effective daily dose ranges from 5 to
15 mg.
Pramipexole (Mirapex), a dopamine D2 and D3 receptor agonist, and ropinirole hydrochloride (Requip), a
dopamine D2 receptor agonist, were recently approved by the Food and Drug Administration for treating
Parkinson's disease. Pramipexole is started at 0.125 mg at bedtime and gradually increased to a maximum of
1.5 mg three times daily. Ropinirole is started at 0.25 mg and increased to 3 to 8 mg three times daily
(19,20).
Benzodiazepines
Benzodiazepines may be used as monotherapy in patients with mild or intermittent symptoms or as add-on
therapy in severe cases. Clonazepam (Klonopin) has been shown to ease the sensory symptoms and periodic
limb movements of sleep in restless legs syndrome (1-3,16). The agent can be started at 0.25 mg at bedtime
and increased by 0.25 mg every week to a maximum of 3 to 4 mg daily in divided doses. Anecdotal reports
indicate that other benzodiazepines, such as temazepam (Restoril) and alprazolam (Xanax), are also
effective. The major side effects of benzodiazepines include daytime drowsiness and confusion, unsteadiness
and falls, and aggravation of sleep apnea.
Opioids
Low-potency opioids, such as codeine and propoxyphene (Darvon, Dolene), can benefit patients with mild
and intermittent symptoms, and higher-potency agents, such as oxycodone hydrochloride (Roxicodone),
methadone (Dolophine) hydrochloride, and levorphanol tartrate (Levo-Dromoran), may have a role in
refractory cases (1-3,16). In a double-blind, placebo-controlled study, oxycodone (mean daily dose, 15.9 mg)
was found to be more effective than placebo (21). However, most physicians are hesitant to use opioids in
restless legs syndrome because of the perceived risk of addiction and do so only in refractory cases.
Anticonvulsants
Double-blind studies have shown that carbamazepine (Tegretol), at a dose of 200 to 400 mg daily, is
effective in reducing sensory manifestations of restless legs syndrome (1-3,16), especially among young
patients with recent onset of disease and severe symptoms. Unfortunately, subsequent clinical experience has
not shown convincing efficacy of carbamazepine.
Open-label studies have found gabapentin (Neurontin) to be effective in relieving sensory symptoms (22)
and periodic limb movements of sleep, even in refractory cases. The drug can be initiated at a dose of 100 to
300 mg at bedtime and increased by 100 to 300 mg every 3 days to a maximum of 2,400 mg daily in divided
doses. Gabapentin is usually well tolerated but may cause transient or mild side effects, such as somnolence,
dizziness, ataxia, and fatigue.
Presynaptic alpha2-adrenergic agonist
Clonidine hydrochloride (Catapres) may be effective in primary restless legs syndrome and that associated
with uremia (1-3,16). The drug should be started at 0.1 mg at bedtime and can be increased every week by
0.1 mg to a maximum of 1 mg daily (average effective daily dose, 0.5 mg). Among the common side effects
are dry mouth, decreased cognition, light-headedness, sleepiness, and constipation.
Summary
Restless legs syndrome is a common, potentially disabling condition that affects about 10% to 15% of the
general population and yet is often unrecognized and misdiagnosed. It is mainly diagnosed clinically and
only rarely requires polysomnography. The condition is usually primary and treatable. First, however,
secondary causes should be sought, especially iron deficiency and peripheral neuropathy, because when the
source is an accompanying factor or condition, the syndrome may be curable. The most effective drugs are
dopaminergic agents, clonazepam, opioids, gabapentin, and clonidine. Additional agents are available that
may be beneficial as add-on or alternative therapy.
What are the mechanisms that cause restless legs syndrome?
Pathogenesis of the syndrome is unclear. Karl A. Ekbom originally proposed that it was mainly the result of
accumulation of metabolites in the legs from venous congestion (1-3). Peripheral nerve abnormalities have
also been proposed, but no structural changes in nerve endings have been seen (4). Many experts believe that
the syndrome is generated centrally (1,3,5). Periodic limb movements of sleep, in particular, are thought to
be caused by sleep-related disruption of descending inhibitory reticulospinal pathways that are normally
active at the brain stem or spinal cord level.
On the basis of treatment response, restless legs syndrome has been linked to dopaminergic or opiate
abnormalities (3). Dopamine blockers and opiate blockers reactivate symptoms when given to patients with
the syndrome. Results of single-photon emission computed tomography have suggested deficiency of
dopamine D2 receptors (6). Sympathetic hyperactivity has also been implicated (5) on the basis of
observations that sympathetic nerve blockade relieves periodic limb movements of sleep and that alphaadrenergic blockers improve symptoms of restless legs syndrome. Studies also have suggested possible
underactivity of the serotonin and gamma-aminobutyric acid neurotransmitter systems.
References
1.
2.
3.
4.
5.
6.
Trenkwalder C, Walters AS, Hening W. Periodic limb movements and restless legs syndrome.
Neurol Clin 1996;14(3):629-50
Silber MH. Restless legs syndrome. Mayo Clin Proc 1997;72(3):261-4
Walters AS, for the International Restless Legs Syndrome Study Group. Toward a better
definition of the restless legs syndrome. Mov Disord 1995;10(5):634-42
Rutkove SB, Matheson JK, Logigian EL. Restless legs syndrome in patients with
polyneuropathy. Muscle Nerve 1996;19(5):670-2
O'Keeffe ST. Restless legs syndrome: a review. Arch Intern Med 1996;156(3):243-8
Staedt J, Stoppe G, Kogler A, et al. Dopamine D2 receptor alteration in patients with periodic
movements in sleep (nocturnal myoclonus). J Neural Transm Gen Sect 1993;93(1):71-4
References
1.
Trenkwalder C, Walters AS, Hening W. Periodic limb movements and restless legs syndrome.
Neurol Clin 1996;14(3):629-50
2. Silber MH. Restless legs syndrome. Mayo Clin Proc 1997;72(3):261-4
3. Walters AS, for the International Restless Legs Syndrome Study Group. Toward a better
definition of the restless legs syndrome. Mov Disord 1995;10(5):634-42
4. Trenkwalder C, Seidel VC, Gasser T, et al. Clinical symptoms and possible anticipation in a
large kindred of familial restless legs syndrome. Mov Disord 1996;11(4):389-94
5. Ondo W, Jankovic J. Restless legs syndrome: clinicoetiologic correlates. Neurology
1996;47(6):1435-41
6. O'Keeffe ST. Restless legs syndrome: a review. Arch Intern Med 1996;156(3):243-8
7. Popoviciu L, Asgian B, Delast-Popoviciu D, et al. Clinical, EEG, electromyographic and
polysomnographic studies in restless legs syndrome caused by magnesium deficiency. Rom J
Neurol Psychiatry 1993;31(1):55-61
8. Rutkove SB, Matheson JK, Logigian EL. Restless legs syndrome in patients with
polyneuropathy. Muscle Nerve 1996;19(5):670-2
9. Kanter AH. The effect of sclerotherapy on restless legs syndrome. Dermatol Surg 1995;21(4):32832
10. Sanz-Fuentenebro FJ, Huidobro A, Tejadas-Rivas A, et al. Restless legs syndrome and
paroxetine. Acta Psychiatr Scand 1996;94(6):482-4
11. Drake ME. Restless legs with anti-epileptic drug therapy. Clin Neurol Neurosurg 1988;90(2):151-4
12. Metcalfe RA, MacDermott N, Chalmers RJ. Restless red legs: an association of the restless legs
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
syndrome with arborizing telangiectasia of the lower limbs. J Neurol Neurosurg Psychiatry
1986;49(7):820-3
Iannaccone S, Zucconi M, Marchettini P, et al. Evidence of peripheral axonal neuropathy in
primary restless legs syndrome. Mov Disord 1995;10(1):2-9
O'Keeffe ST, Gavin K, Lavan JN. Iron status and restless legs syndrome in the elderly. Age
Ageing 1994;23(3):200-3
Botez MI, Lambert B. Folate deficiency and restless-legs syndrome in pregnancy. N Engl J Med
1977;297(12):670
Krueger BR. Restless legs syndrome and periodic movements of sleep. Mayo Clin Proc
1990;65(7):999-1006
Allen RP, Earley CJ. Augmentation of the restless legs syndrome with carbidopa/levodopa. Sleep
1996;19(3):205-13
Earley CJ, Allen RP. Pergolide and carbidopa/levodopa treatment of the restless legs syndrome
and periodic leg movements in sleep in a consecutive series of patients. Sleep 1996;19(10):801-10
Ondo W. Ropinirole for restless legs syndrome. Mov Disord 1999;14(1):138-40
Lin SC, Kaplan J, Burger CD, et al. Effect of pramipexole in treatment of resistant restless legs
syndrome. Mayo Clin Proc 1998;73(6):497-500
Walters AS, Wagner ML, Hening WA, et al. Successful treatment of the idiopathic restless legs
syndrome in a randomized double-blind trial of oxycodone versus placebo. Sleep 1993;16(4):32732
Adler CH. Treatment of restless legs syndrome with gabapentin. Clin Neuropharmacol
1997;20(2):148-51
Dr Evidente was a fellow in movement disorders and Dr Adler is associate professor of neurology,
Parkinson's Disease and Movement Disorders Center, Mayo Clinic Scottsdale, Scottsdale, Arizona. Dr
Evidente is now at St Lukes Medical Center, Quezon City, Philippines. Correspondence: Charles H. Adler,
MD, PhD, Parkinson's Disease and Movement Disorders Center, Mayo Clinic, 13400 E Shea Blvd,
Scottsdale, AZ 85259.
RETURN TO MARCH 1999 TABLE OF CONTENTS
HOME | JOURNAL | PATIENT NOTES | DIGITAL DOC | PEARLS | CME | CLASSIFIED
ADVERTISING | ABOUT US
Copyright (C) 1999. The McGraw-Hill Companies. All Rights Reserved
E-mail Privacy Notice