Lessons 6-9
advertisement

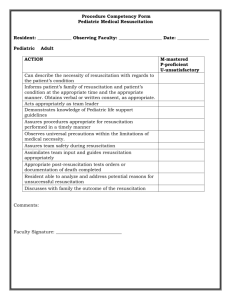
RSPT 2353 – Neonatal/Pediatric Cardiopulmonary Care Neonatal Resuscitation Program Lecture Notes: Lessons 6 - 9 Reference & Reading: Textbook of Neonatal Resuscitation, 5 t h ed. I. LESSON 6: MEDICATIONS a. Epinephrine is indicated when the HR remains below 60 bpm, despite 30 seconds of effective assisted ventilation & another 30 seconds of coordinated chest compressions & ventilation. A small number of newborns (<2 per 1,000 births) will still require medication during resuscitation. Before administering epi, ensure ventilation & compressions are being given optimally & that 100% FiO2 is being used 1. Is there good chest movement? 2. Audible bilateral breath sounds? 3. Intubation completed & tube placement confirmed? When expecting a very ill newborn, who will likely require extensive resuscitation, prepare UVC & epinephrine prior to birth if possible b. The umbilical vein is the preferred route for epinephrine administration. Should be sterile c. Alternative routes ETT – should use higher dose; used as alternative while IV or UVC access is being established Intraosseous – usually in outpatient setting d. Give epinephrine after ventilation has been established Giving epi, prior to establishing ventilation wastes valuable time that should be focused on ventilation & oxygenation e. Preparation & Dose Concentration: 1:10,000 Recommended preparation: 1. IV: 0.1-0.3 mL/kg 2. ETT: 0.3 – 1 mL/kg Rate – Rapidly Follow with compression & ventilation May be repeated q3 – 5 minutes; if no improvement – check everything f. If there is evidence of blood loss, & poor response to resuscitation, consider possibility of volume loss Indications: 1. Poor response to effective ventilation, chest compressions & epinephrine 2. Pale 3. Delayed cap refill 4. Weak pulses 5. Persistently low HR 6. Hx of condition associated with fetal blood loss Recommended solutions 1. Normal saline, ringer’s lactate 2. O Rh-negative PRBCs (cross match to mother if time) Dose: 10 mL/kg Route: UVC, IV Rate: 5-10 minutes Signs of improvement: ↑ HR, Pulses strengthen, Pallor Lessens , ↑ BP If no improvement – consider hypovolemia, pneumothorax, CDH, or CHD If HR absent or no progress is made in certain conditions (extreme prematurity) – it may be appropriate to discontinue resuscitative efforts. Hiccup twins II. LESSON 7: SPECIAL CONSIDERATIONS a. There are 3 main categories of babies who do not improve after resuscitation PPV fails to result in adequate ventilation of the lungs Baby remains cyanotic or bradycardic despite goo ventilation Baby fails to begin spontaneous respirations b. PPV fails to result in adequate ventilation of the lungs Mechanical blockage 1. Meconium or mucus in the pharynx or trachea 2. Choanal atresia 3. Pharyngeal airway malformation (Pierre Robin) 4. Other rare conditions: laryngeal webs, cystic hygroma, congenital goiter Impaired lung function 1. Pneumothorax 2. Congenital pleural effusions 3. Congenital Diaphragmatic hernia 4. Pulmonary hypoplasia 5. Extreme immaturity 6. Congenital pneumonia c. Persistent cyanosis, bradycardia Consider congenital heart disease Rarely caused by CHD, problem is more likely due to inadequate ventilation d. Failure to begin spontaneous respirations If PPV results in normal HR & color, yet baby still has poor muscle tone & no spontaneous respirations Consider 1. Brain injury 2. Severe acidosis 3. Congenital neuromuscular disorder 4. Sedation due to maternal drugs pass to the baby across placenta Naloxone HCL 1. Concentration: 1.0 mg/mL 2. Route: IV, UVC 3. Dose: 0.1 mg/kg 4. If addiction present or on methadone maintenance – do not give narcan, may result in seizures e. Post-resuscitation care – Do not assume that a baby who has been successfully resuscitated is healthy & can be treated as a routine newborn. Those who required prolonged PPV, intubation, and/or compressions are at risk for multi-organ damage f. PPHN – term & post-term are most susceptible; maintain high levels of O2 Pneumonia – at risk from aspiration or congenital infection Metabolic acidosis – lactic acid build up from prolonged insufficient tissue oxygenation; use NaHCO3 – controversial Hypotension – Heart muscle & vascular tone can be stressed during compromise. Fluid management – perinatal compromise can cause transient renal failure; monitor closely Seizures or apnea – resuscitated babies may develop hypoxic-ischemic encephalopathy Hypoglycemia – metabolism during oxygen deprivation uses more glucose than during adequate oxygenation Feeding problems – the newborn GI tract is sensitive to hypoxiaischemia. Ileus, GI bleeding & NEC can result Temperature management –Maintain the baby’s temperature in the normal range; do not overheat! Resuscitation outside the hospital or beyond immediate newborn period. Physiologic principles & steps for resuscitation remain the same: 1. Warm positions, clear airway, stimulate to breathe, & give oxygen if necessary. 2. Establish effective ventilation 3. Provide chest compressions 4. Administer medications Restoring adequate ventilation remains priority. Once ventilation is ensured, consider additional information about hx to guide focus of resuscitation efforts Challenges & strategies: 1. Temperature control: increase environmental heat, dry with bath towels, blankets or clean clothing; skin-to-skin 2. Clear airway: handkerchief or blub syringe 3. Ventilation: if no device is available, mouth-to-mouth-and-nose 4. Vascular access: use IO, peripheral access 5. Medications: epinephrine is preferred for resuscitation, other may be necessary III. LESSON 8: RESUSCITATION OF BABIES BORN PRETERM a. Preterm babies are at higher risk for complications due to anatomic & physiologic immaturity. Thin skin, large surface area, decreased fat = easy heat loss Immature tissues Weak muscles Immature nervous system Immature lungs deficient in surfactant Immature immune system Fragile capillaries Low blood volume b. Delivery requires Additional personnel Additional means to maintain temperature c. Keeping preterm babies warm ↑ room temperature Preheat radiant warmer Obtain portable warming pad Babies < 28 weeks use recloseable polyethylene bag or plastic wrap from neck down Use prewarmed transport incubator Do not overheat Maintain axillary temperature of 36.5OC d. Oxygen administration NRP recommends 100% Consider blending Amount to deliver is determined by: 1. Clinical assessment 2. Concentration of O2 delivered 3. Pulse oximeter measurement Aim for saturations of 85-95% e. Assisting ventilation Consider CPAP if: 1. Baby is breathing 2. HR >100bpm And 3. Has labored respirations, cyanosis or low SpO2 Administer with flow-inflating bag or T-piece resuscitator Use 4-6 cmH2O, ensure tight seal Give PPV if – baby is apneic, HR <100 bpm and persistent cyanosis Giving PPV: 1. Use 20-25 cmH2O 2. Avoid excessive chest rise f. Consider surfactant if: Baby is <30 weeks gestation Even if not in respiratory distress Baby is fully resuscitated Prophylactic administration is within local practice g. Decreasing brain injury Handle gently Avoid trendelenburg Avoid excessive pressures, even CPAP Do not rapidly infuse fluids Karate Baby IV. LESSON 9: ETHICS & CARE AT THE END OF LIFE a. Ethical principles of neonatal resuscitation are not different from those followed in resuscitating an older child or adult. b. Common ethical principles that apply to all medical care include the following: Autonomy: Respect the right to liberty & freedom. (exceptions : life threatening medical emergencies & patient’s are not competent to make their own decisions Beneficence: Do good things for people. Nonmaleficence: Do not harm people. Justice: treat people truthfully & fairly c. Parents are usually considered to be best decision maker for their infant. Parents are usually given the responsibility of guarding the infant’s best interests. d. Give relevant, accurate, and honest information about risks & benefits of each tx option. e. Give time to consider, ask questions & seek other opinions f. Factors to consider: What is in the baby’s best interest? 1. Chances that therapy will succeed 2. Risks involved with tx, & non-tx 3. Degree to which therapy, if successful will extend life 4. Pain & discomfort associated with therapy 5. Anticipated quality of life for the newborn with and without tx g. Laws and Neonatal Resuscitation There is no US federal law mandating delivery room resuscitation in all circumstances In most cases, it is ethically and legally acceptable to withhold or withdraw resuscitation efforts, if there is agreement from healthcare professionals & parents that further medical intervention will be futile, prolong dying or would not offer sufficient benefit to justify the burdens imposed. h. Noninitiation of resuscitation Prognosis certain: gestation, birth weight, and/or congenital anomalies are associated with almost certain death, and unacceptably high morbidity. Exceptions may be made based on parental desires. 1. Newborns with confirmed gestation of < 23 weeks or birth weight < 400g 2. Anencephaly 3. Confirmed trisomy 13 or trisomy 18 syndrome Prognosis uncertain: there is borderline survival & relatively high rate of morbidity & where burden to child is high – parents’ views on initiating or withholding resuscitation should be honored. Be cautious making unalterable decisions about resuscitations before birth i. Resuscitation against parental wishes In conditions associated with high rate of survival & acceptable rate of morbidity, resuscitation is nearly always indicated and health care providers have a legal & ethical obligation to provide appropriate care. If parents & providers disagree: 1. Consult ethics committee or legal counsel 2. If no time, resuscitation may occur over parental objections 3. Provide accurate documentation of the basis of decision. j. Prenatal counseling Neonatal & OB service should talk to parents – prior both services should discuss case k. Uncertain prognosis immediately after birth Initial resuscitation and provision of life support allows addition time to gather more complete clinical information & permits more input from parents May decide to discontinue life-sustaining treatment Avoid initiating resuscitation many minutes after birth due to a change of plans. l. Baby not responding to efforts If there is no HR after 10 minutes of complete & effective resuscitation More than 10 minutes may have been required to assess the baby to optimize efforts m. Telling parents the baby has died Support parents by giving clear and honest information in a supportive & caring manner DO NOT SAY: 1. “It was for the best.” 2. “It was meant to be.” 3. “You can have more children.” 4. “You didn’t have time to know her.” Provide humane & compassionate care. 1. Let parents hold 2. Promote quiet atmosphere 3. Remove tubes & equipment, clean baby’s face & mouth 4. Wrap baby in clean blanket 5. Explain what they will see. 6. Be available & check in 7. Be culturally sensitive Support of parents : exchange contact information, inform mother’s primary care provider, Support of staff: consider debriefing session, and avoid speculation based on secondhand information