Short Notes on Headache - Vanderbilt University Medical Center
advertisement

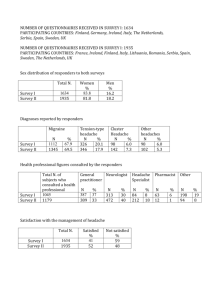
Short Notes on Headache Number Six Tension-Type Headaches Tension-type headaches (TTH) are the second most common type of headache. They are slightly more common in females than males and occur in both children and adults. The incidence declines in the aged. Various studies have shown that 70 – 90 percent of the population has experienced these. The only more common headache is the momentary ice-cream headache which is usually triggered by something cold in the mouth and noted by 90 – 95 percent of the population. In earlier years TTH were called tension headaches or muscle contraction headaches, even though there was no association with tension or anxiety. Muscle tightness or tenderness did not always occur with these. In 1988 the Classification Committee of the International Headache Society called these “tension-type” with a hyphen between the two words and that term has stuck since then. Clinically the TTH are not accompanied by other symptoms or signs of neurological dysfunction such as papilledema, cranial nerve dysfunction or weakness. There is absence of manifestations of systemic disease such as fever or marked hypertension. TTH can be divided into three groups. The first is episodic tension-type (ETTH) which occurs less than 15 days per month and is not associated with other types of headache. The next is chronic tension-type (CTTH) which is noted 15 or more days per month. The third are the tension-type headaches associated with migraine and most often is a part of rebound headaches (medication-overuse headaches). The latter have either a TTH or migraine at least 15 days per month and usually have only 0-2 headache-free days a week. The etiology of episodic TTH is unknown. Throughout the years there have been numerous reports of an alteration of a neurotransmitter or other chemical disorder as the basis of TTH. Then the next article in the same or another journal refutes these chemical changes. Most often there is no association with stress, diet, hunger, any daily activity, lack of sleep or other factor. Thus ETTH is a condition of unknown etiology which is diagnosed by the clinical symptoms. The clinical features of TTH cannot be explained. ETTH usually begin in the afternoons or evenings. The duration is one-half hour to several hours. They most often cease during sleep and are not noted the following day. Rarely they can persist for several days. The pain may be unilateral or bilateral and may be frontal, occipital or generalized. The pain may occasionally be described as throbbing or pulsating. The pain may be mild or moderate, but never severe or disabling. Exertion does not increase the pain and there is no limitation of daily activities and no urge for bed rest. There can be mild photophobia or phonophobia but not both. In contrast to some migraines there is no intensification of the pain with smelling gasoline or perfume –the condition referred to as osmophobia. Anorexia may be noted but not nausea or vomiting. Fortunately the ETTHs are quickly relieved with aspirin, acetaminophen, ibuprofen or sodium naproxen, each being an inexpensive off-the-shelf medication. These patients rarely seek medical attention. This is in contrast to patients with CTTH with or without migraine who are the most frequent headache patients seeking medical care. Chronic tension-type headache (CTTH) without accompanying migraine is infrequent. In contrast to the clinical features of ETTH, the International Headache Society’s classification permits the diagnosis of CTTH when there is nausea without vomiting. There may be multiple causes of CTTH. They may be the result of an adverse effect of a medication taken for some other condition. Headaches due to an adverse effect of a daily medication might start as late as six months after the medication was first taken. When the patient is seeing multiple physicians, the combination of medications that are being prescribed might be the cause of CTTH. CTTH may occur with cryptococccal meningitis and similar chronic infections in the absence of papilledema or other symptoms or signs. When the CTTH last most all day and occur five or more times a week, they may be a presentation of rebound headache (medication-overuse headache). Often CTTH are idiopathic. The patient with CTTH without migraine requires a thorough history, general physical examination and a complete neurological examination. Often laboratory studies and imaging studies are indicated. All medications, both offthe-shelf and those which have been prescribed, must be listed. Those that are not essential should be stopped. If the patient is receiving a medication for a condition requiring treatment, the medication should be stopped and another medication having the same action be substituted. An example would be stopping the beta blocker that is being given for hypertension and using a calcium channel blocker. When the cause of CTTH cannot be determined, the patient might be tried on a tricyclic antidepressant, starting with a low dose and gradually increasing the daily dose if necessary. Non-pharmacological treatments have generally failed. CTTH without migraine may spontaneously cease. Patients with both chronic tension-type headache and migraine are the most frequent referrals to a headache clinic. These account for 1-3% of the patients seen in a primary care physician’s office and an emergency room. Until proven otherwise their diagnosis is rebound headache (medication-overuse headache). This problem will be discussed in detail in a later short notes on headache. John S. Warner, M.D. Professor, Emeritus Department of Neurology Vanderbilt University School of Medicine