Drugs 41 (Suppl. 3): 80-91, 1991
0012-6667/91/0300-0080/$6.00/0
© Adis International Limited All
rights reserved.
DRSUP2155
Low Dose Loop Diuretics in Essential Hypertension
Experience with Torasemide
I. Achhammer and P. Metz
Clinical Development and Project Development, Boehringer Mannheim GmbH,
Mannheim, Federal Republic of Germany
Summary
Diuretics belong to the class of antihypertensive drugs recommended for first-line
therapy of essential hypertension. Although they are widely and effectively used for the
treatment of hypertension, the question remains whether their possible negative influence
on metabolic and electrolyte parameters could partly offset the benefit of blood pressure
reduction with respect to reduction of coronary artery disease.
Recently published data demonstrate that much lower doses of thiazides exert the
same antihypertensive effect as the higher doses used in the past and even prescribed
today. These lower doses produce relatively little change in biochemical parameters. Thus,
the postulated risks can be avoided by using the lowest effective dose. Traditionally, loop
diuretics of the furosemide (frusemide) type are rareiy used as first-line antihypertensive
agents. They seem to display less efficacy coupled with an intense diuresis when used in
standard available doses. However, there is evidence that newly developed loop diuretics,
in lower doses than used in congestive heart failure, are effective antihypertensive agents.
For example, torasemide 2.5mg once daily, which does not exert a significant diuresis
over 24 hours compared with placebo, lowers elevated blood pressure to a similar extent
than thiazides or related compounds. This antihypertensive effect is accompanied by less,
if any, changes in metabolic or electrolyte parameters compared with widely used standard diuretics such as hydrochlorothiazide, indapamide or chlorthalidone. The influence
on serum potassium and magnesium is similar to or even less than fixed combinations
of hydrochlorothiazide and triamterene or amiloride.
Thus, low-dose torasemide constitutes an alternative to established thiazide antihypertensive therapy.
1. Introduction
Continuously high blood pressure presents a
persistent cardiovascular risk. As many as 10 to
20% of the adult population are found to have mild
elevations in blood pressure. Antihypertensive
treatment based on diuretics and -blockers has
improved the risks associated with high blood
pressure in severe, moderate and mild hyperten-
sion. The beneficial effect seems to depend on the
severity of hypertension, being less evident in mild
hypertensives who are the majority. Even if there
is agreement to treat patients with essential hypertension in order to prevent cardiovascular complications, large scale intervention trials clearly
showed prevention of stroke, progression of hypertension and of cardiac failure, but failed to prove
consistent significant effects on coronary artery
Torasemide in Essential Hypertension
disease. In fact, meta-analysis of several large scale
intervention trials has indicated that the reduction
of coronary heart disease mortality which occurs
as less than half of that expected, based on epiemiological data on the associaton between high
Wood pressure and coronary heart disease (Amery
et al. 1990; Collins et al. 1990; McMahon at al.
1990). To date, there are no data on cardiovascular
mortality and morbidity for the newer antihypertensive agents, e.g. angiotensin converting enzyme
(ACE) inhibitors and calcium channel blockers in
the treatment of hypertensive patients. However,
based on their possible potential advantages over
thiazides and -blockers with respect to metabolic
effects, they are recommended as 'first-line' therapy
together with diuretics and -blockers (Joint National Committee 1988). This approach is not
completely shared by others (Swales et al.
1989;
Swales 1990) who more rigidly recommend diaretics-and -blockers as first-line antihypertensive
drugs and the other classes in case of contraindications or ineffectiveness.
2. Diuretics in the Treatment of Mild
Hypertension
The appearance of thiazide diuretics in the
1950s, with their improved tolerability profile over
existing agents constituted a turning point in the
pharmaceutical handling of essential hypertension.
Today, there is no doubt that diuretics induce
a decrease in arterial blood pressure in hypertensive patients during long term therapy. However,
the mode of antihypertensive action of diuretics
has not been completely understood. The loss in
intravascular volume can only explain the early
phase of antihypertensive activity, but not the
chronic phase.
Several mechanisms have been proposed for the
antihypertensive action of diuretics:
• intravascular volume contraction
• reduced vascular responsiveness to naturally oc
curring vasoconstrictor substances and enhanced
responsiveness to depressor substances
• decreased sodium content of the arterial wall
• altered transmembrane ionic exchange
• diminished baroreceplor activity
• induction of local tissue dilators (e.g. kinins,
prostacyclins) in the arterial wall
• a direct vasodilating action on the arteriole
(Bakris & Frohlich 1989).
Despite their obscure mechanism of action, diuretics are an effective antihypertensive treatment
and are widely used. They are usually well tolerated and physicians can rely on a long history of
experience in their use. Diuretics require less titration to arrive at an effective dose compared with
other antihypertensive drugs (Kau 1988), and are
less expensive on a cost per day basis. Furthermore, the development of tolerance has not been
described.
Many of the disadvantages associated with diuretic therapy result from their use as first-line
treatment in the traditional stepped care appronch, with
titration to high doses resulting. in metabolic side
effects. Adverse effects such as glucose intolerance,
decreased serum potassium, magnesium and
sodium, and increased serum uric acid, cholesterol
and tridycerides have been reported. Metabolic
disturbances inclease with higher diuretic
doses, but
antihypertensive efficacy does not increase in parallel (Beermann & Groschinsky-Grind 1978; Carlson et al. 1990; Materson et al. 1978; McVeigh et
al. 1988).
It has been debated whether negative effects on
metabolic parameters, or arrhythmia through potassium and magnesium depletion caused by diuretics could, at least in part, offset the possible
benefit of blood pressure reduction on coronary artery disease. Hypercholesterolaemia, glucose intolerance and hyperinsulinaemia are risk factors for
coronary artery disease which may be aggravated
by diuretics.
There is some evidence for a negative effect of
diuretics, especially on glucose metabolism, over
long term treatment but data available from prospective studies are inconclusive (Freis 1989;
McMahon 1990; Morgan 1990; Skarfors et al. 1989;
Thomson 1990). In addition, the data on the effect
of diuretics on regression of left ventricular hypertrophy are contradictory (Komajda et al. 1990;
Mace et al. 1985; Shigematsu et al. 1990).
82
Drugs 41 (Suppl. 3} 1991
Today a more individualised approach is
recommended, which also takes into consideration
the risk: benefit ratio for the particular patient. Low
doses of diuretics are recommended for initial
monotherapy. Before titrating one compound to
high levels, a second should be added or another
drug with a different mechanism of action should
be tried (Joint National Committee 1988). In the
spectrum of antihypertensive drugs, diuretics have
the advantage of fewer contraindications and a welldefined tolerability profile. The basic requirement
for optimal therapy is knowledge of the dose-response curve in order to avoid unnecessarily high
doses (Brunner et al. 1990).
3. Loop Diuretics in Mild Hypertension
Loop diuretics are often regarded as more potent natriuretics than thiazide diuretics due to their
rapid onset of diuretic action after administration.
This concept is questionable however, when the effects of once-daily dosing on 24-hour excretion of
water and solutes are evaluated (Reyes et al. 1988,
1990a; Leary & Reyes 1988).
Additionally, data available for furosemide suggested less antihypertensive efficacy than standard
doses of thiazides (McMahon 1990). In consequence, the use of loop diuretics was recommended in cases with concomitant chronic renal
failure and in the treatment of hypertensive crisis,
but not as first-line therapy of mild hypertension.
However, during the last few years well-controlled
studies have been published indicating that newly
developed loop diuretics such as torasemide, muzolimine and etozoline, which differ from furosemide by a longer duration of action, are efficacious
antihypertensive agents when used as monotherapy compared with thiazides or other antihypertensives (Achhammer & Eberhard 1990; Cocchieri
et al. 1985; Kirsten et al. 1985; Lucsko et al. 1985;
Pagano et al. 1985; Reyes et al. 1990a; Romano et
al. 1987; Russo et al. 1987; Spannbrucker et al.
1988).
4. Thiazide and Loop Diuretics,
Establishing the Antihypertensive
Dose Range
Loop diuretics have a striking diuretic effect
within hours of administration of a standard dose
(e.g. furosemide 40mg or torasemide l0mg) and a
clear dose-response relationship over a wide dose
range (Lambe et al. 1986). In contrast, thiazides
show a fairly flat dose-response relationship; doses
higher than hydrochlorothiazide 12.5 to 25mg do
not provoke increased excretion of volume and
sodium compared with the lower dose (Beermann
& Groschinski-Grind 1977).
Doses as low as hydrochlorothiazide or chlorthalidone 12.5mg have been used effectively to
lower blood pressure in essential hypertension
without the pronounced electrolyte and metabolic
disturbances of high doses (Beermann & Groschinski-Grind 1978; Materson et al. 1978). Recently published placebo-controlled studies clearly
establish that doses far below those commonly
marketed display similar antihypertensive effects
with little if any influence on electrolyte or metabolic parameters (Carlson et al. 1990; McVeigh et
al. 1988). Cyclopenthiazide 125 and 500 g produced the same blood-pressure lowering effect, and
bendroflumethiazide 1.25mg produced the same
effect as bendroflumethiazide l0mg, the dose used
in the MRC trial (Medical Research Council
Working Party 1985). The use of thiazides is open
to challenge by newer agents because of the formers' negative biochemical effects and little impact
on cardiovascular mortality in the large intervention trials. However, in the context of recent data
the use of thiazides in lower doses might have a
more favourable impact than already discussed.
There is comparable evidence available for
torasemide that doses lower than those used for
treatment of oedema are useful for antihypertensive treatment. Clinical pharmacological studies
comparing placebo and torasemide 2.5 to 20mg
show a dose-dependent increase in volume and
sodium excretion in the early phase (0 to 6 hours)
after administration, followed by a rebound phenomenon at doses of 10mg and higher (Reyes et al.
Fig. 1 Mean values of intracellular Ca++ and Na+ activity and diastolic blood pressure from all patients (n = 14) during
antihypertensive treatment with torasemide (median dose 5mg) [H. Vetter, unpublished, with permission].
1990b). The increase after torasemide 2.5 or 5mg
is small, with changes in maximal urinary flow and
the peak effect being similar for torasemide 5mg
and hydrochlorothiazide 25mg, demonstrating that
the striking diuretic effect of standard loop diuretic
doses used in congestive heart failure (e.g. torasemide l0mg and furosemide 40mg) is not overt at
lower doses (Reyes et al. 1988, 1990b). The time
course of the excretory effects of torasemide on urinary fluid and electrolytes was also dose dependent. Compared with placebo, maximal urinary flow
increased and time to maximum flow decreased as
a function of dose. Low doses, of a loop diuretic
therefore mimic the excretory profile of a thiazide
diuretic (e.g. hydrochlorothiazide 25mg), but the
potency in terms of absolute urinary excretion is
much lower (for review see Reyes, pp. 35-59 this
issue). Torasemide 2.5 or 5mg once daily increased
24-hour volume and electrolyte excretion slightly
but nonsignificantly compared with placebo, without a significant rebound effect.
two open-dose titration studies in a total of 34
patients addressed the question of whether these
low doses would be effective antihypertensive
treatment. Both studies started with torasemide
2.5mg after a placebo washout and allowed incremental increases in dose after 2 or 4 weeks, respectively. In 1 study (n = 20), torasemide 2.5mg
administered for 4 weeks lowered blood pressure
significantly. When the dose was doubled a further
decrease in blood pressure resulted with a total response rate after 6 weeks [diastolic blood pressure
(DBF) 90mm Hg] of 75%. An increase to torasemide l0mg did not result in an additive decrease
in blood pressure (Mueller & Haecker 1985). In the
second study (n = 14), the starting dose was torasemide 2.5mg doubled every 2 weeks in nonresponders. Response was reached in the dose range
of 2.5 to 5mg in 64% of patients, confirming the
84
Drugs 41(Suppl.3) 1991
results of the first study. No additional antihyperiensive effect was seen in the remaining nonresponders using up to 15mg of torasemide (H. Vetter, personal communication). In the latter study,
the decrease in DBP from 112.4 + 13.4mm Hg to
88.2 + 11.4mm Hg was accompanied by a small
increase in intracellular erythrocyte free-sodium
activity and a significant decrease in intracellular
free-calcium (fig. 1). This effect on intracellular
electrolyte activity has also been demonstrated in
a single-dose study (Spieker et al. 1990), suggesting
that intracellular free-calcium plays a dominant role
in regulating vascular tone in essential hypertension (Spieker et al. 1988; Zidek et al. 1982, 1984).
In a multicentre, double-blind placebo-con-trolled
parallel group study, patients with a DBF of 95 to
115mm Hg received torasemide 2.5 or 5mg for 12
weeks (table I; Achhammer et al., unpublished
data). 154 patients were enrolled and 147 qualified
for efficacy analysis according to intention-to-treat
analysis. Blood pressure was reduced significantly
(p < 0.05) in all 3 groups, but torasemide
significantly reduced sitting DBF compared with
placebo at end-point without a significant difference
between the 2 doses. Although the difference
between torasemide and placebo was evident 2 to 4
weeks after the start of treatment, maximum and
statistically significant differences were not
observed until 8 weeks. No significant decrease
in bodyweight, which could serve as an indicator
for increased diuresis, could be detected. Blood
pressure response (defined as DBF 90mm Hg or
decrease in DBF of 10%) was achieved in 28%
of patients in the placebo group, 46%jin the torasemide 2.5mg group and 50% in the torasemide
5mg group. Eight of 50 patients receiving torasemide 2.5mg, 10 of 53 patients receiving torasemide
5mg and 13 of 51 patients receiving placebo withdrew from the study. The higher trend for placebo
was caused by withdrawal due to nonresponse. The
adverse event rate was similarly distributed over
all 3 groups with 4 of 50, 5 of 53 and 5 of 51 patients
receiving torasemide 2.5 and 5mg and placebo, respectively. Adverse events reported were mainly
dizziness and headache. No significant difference
in serum concentrations of potassium, uric acid,
glucose, cholesterol and triglycerides was found after
torasemide or placebo.
Two other single-centre trials compared torasemide 2.5mg once-daily with placebo over 4 weeks
(Dupont et al. 1988), or over 8 weeks with chlorthalidone 25mg as a positive control (Porcellati et
al. 1990).
Both studies revealed a significant blood pressure-lowering effect of torasemide 2.5mg compared
with placebo, which was similar to that achieved
with chlorthalidone. Torasemide 2.5mg did not affect serum potassium, magnesium, glucose or chol-
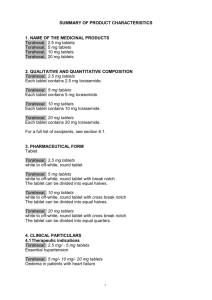
Table I. Effect of once-daily placebo, torasemide 2.5 and 5mg for 12 weeks on sitting systolic blood pressure (SBP), diastolic blood
pressure (DBP) and serum biochemical parameters in patients with essential hypertension (DBP 95-115mm Hg at baseline) [all values
mean ± SD]
Parameter
Placebo (n = 50)
start
12 weeks
Torasemide 2.: 5mg (n = 47)
Torasemide 5mg
(n = 50)
start
12 weeks
start
12 weeks
SBP (mm Hg)
175.4 ± 19.0
168.8 ± 24.3
172.1 ± 16.1
158.2 ± 16.2*
169.6 ± 17.2
159.3 ± 13.4'
DBP (mm Hg)
Heart rate (beats/min)
102.4 ± 4.5
76.4 ± 4.9
97.4 ± 9.2
76.7 ± 9.8
101.2 + 3.8
75.7 ± 6.3
92.6 ± 9.0*
74.6 ± 5.1
102.2 ± 4.0
75.3 ± 4.0
92.4 ± 8.7*
74.5 ± 5.8
K+ (mmol/L)
4.4 ± 0.4
4.4 ± 0.3
4.5 ± 0.5
4.7 ± 0.5
Uric acid (mol/L)
345 ± 105
348 ± 106
356 ± 75
312 ± 69*
368 ± 98
Glucose (mmol/L)
Cholesterol (mmol/L)
Triglycerides (mmol/L)
5.5 ± 1.2
6.7 ± 1.1
1.7 ± 0.9
5.7 ± 1.3
6.7 ± 1.3
1.9 ± 1.1
5.1 ± 1.2
6.9 ± 1.2
1.7 ± 0.9
5.1 + 2.3
6.9 ± 1.2
1.9 ± 1.1
4.8 ± 0.7
6.6 ± 1.2
1.8 ± 1.0
* = p < 0.05 compared with placebo.
4.3 ± 0.4
4.4 ± 0.3
366 ± 97
5.1 ± 0.7
6.5 ± 1.2
2.4 ± 2.0
85
Trasemide in Essential Hypertension
terol compared with placebo, whereas chlorthalidone produced a significant increase in uric acid,
glucose and cholesterol, and a significant decrease
in serum potassium (table II).
Dupont et al. (1988) also reported no increase in
the activity of the renin-angiotensin system and
no stimulation of plasma renin activity or haemoglobin A1 with torasemide compared to placebo.
5. Torasemide Compared with
Other Diuretics
5.1 Efficacy
Several studies compared torasemide 2.5mg once
daily with other commonly used diuretics, using a
double-blind parallel group design and lasting 8 to
24 weeks. Patients presenting with mild to moderate hypertension were included (table HI).
Blood pressure showed a significant reduction
within the first week after starting therapy and
con-tinued to decrease up to 'weeks 8 to 12 for
both torasemide and the comparator drugs. In
some studies where dose-doubling was allowed in
patients not responding to the initial dose, a
similar number of patients with torasemide or the
comparison diuretic received the double dose
according to protocol (usually about 20 to 30% of
patients) [Ach-hammer & Eberhard 1990; Boelke
et al. 1990b; Spannbrucker et al. 1988].
Significant differences between treatments in the
blood pressure-lowering effect were seen in only
2 studies during the course of treatment.
Torasemide 2.5mg lowered sitting DBF and systolic blood pressure (SBP) significantly less than a
fixed combination of hydrochlorothiazide 50mg and
amiloride 5mg after 10 weeks of treatment, but not
at end-point after 24 weeks (Boelke et al. 1990b).
Reyes et al. (1990) reported a significantly more
pronounced effect of hydrochlorothiazide 25mg
compared with torasemide 2.5mg on SBP but not
on DBF in patients aged > 65 years.
On average, SBP and DBP decreased in the
range of 13-27/13-22mm Hg with lorasemide compared with 15-42/14-23mm Hg with thiazides and
related compounds. The overall response rate was
defined as DBP 90mm Hg with some studies also
requiring a decrease in DBP of 10mm Hg. 70 to
90% of patients responded irrespective of the diuretic used (including dose-doubling) [table III].
The time course of the blood pressuse lowering effect was similar for thiazides and torasemide.
Steady-state antihypertensive effect was reached
between 8 to 12 weeks after initiating therapy. Additionally, it could be shown that torasemide 2,5 mg
lowered continuously monitored 24-hour ambulatory
blood pressure to a similar extent compared with
the combination of hydrochlorothiazide 25mg/
triamterene 50mg, by preserving circadian rhythm
over time (Boelke et al. 1990a).
5.2 Safety
In accordance with the results of placebo-controlled studies, torasemide, in the dose range 2.5
to 5mg once daily, did not affect serum potassium
Table II. Effect of once-daily placebo, torasemide 2.5mg and chlorthalidone 25mg for 8 weeks on systolic blood pressure
(SBP), diastolic blood pressure (DBP) and serum biochemical parameters in patients with essential hypertension (DBP > 95mm
Hg) [adapted from Porcellati et al. 1990]
Mean change from baseline
no. of
cholesterol
(mg/dl)
SBP
patients
DBP
(mm Hg)
potassium
uric acid
glucose
(mm Hg)
(mmol/L)
(mg/dl)
(mg/dl)
Placebo
9
-2.0
-1.0
+0.2
+0.1
±0.0
-8.0
Torasemide 2.5mg
9
-13.0*
-14.0*
±0.0
+0.2
-6.0
+6.0
Chlorthalidone 25mg
9
-15.0*
-15.0*
-0.7*
+1.4*
+15.0*
+28.0*
*= p < 0,01 vs baseline (no significant changes were seen for serum concentrations of chloride, calcium, magnesium, or
creatinine for either treatment).
86
Drugs 41 (Suppl. 3) 1991
or glucose significantly, whereas all monodiuretics
used (indapamide, hydrochlorothiazide or chlorthalidone) caused significant decreases in serum
potassium and increases in blood glucose (Porcellati et al. 1990; Reyes et al. 1990a; Spannbrucker
et al. 1988). Torasemide did not affect serum potassium and magnesium compared to a fixed combination of hydrochlorothiazide/triamterene 25/
50mg (fig. 2; Achhammer & Eberhard 1990). In this
study, transient decreases in serum potassium below
3.5 mmol/L were noted in 1 of 29 patients in the
torasemide group and 3 of 29 patients in the combination group. Serum potassium was reduced more
with the fixed combination of hydrochlorothiazide/amiloride 50/5mg than with torasemide; the
same applies for the number of hypokalaemic
events comparing both drugs [serum potassium <
3.5 mmol/L in 3 of 71 patients and 6 of 72 patients
with torasemide or the fixed combination, respectively (Boelke et al. 1990b)]. These data are in ac-
cordance with literature on this fixed combination,
reporting more frequent hypokalaemic events than
expected for a 'potassium sparing' combination.
A usual finding for all diuretics studied was the
incremental increase in uric acid, achieving partial
significance in some studies. The incremental increase in uric acid and glucose was found to be
comparatively higher for hydrochlorothiazide/amiloride 50/5mg than for torasemide 2.5mg, most
likely as a result of the full diuretic dose of the
thiazide being used (Boelke et al. 1990b).
Torasemide had a favourable tolerability profile
when the cumulative rate of subjective adverse
events was evaluated. About 20% of patients receiving torasemide experienced at least 1 adverse
event, compared with about 40% of those receiving
thiazides, or thiazide/amiloride or triamterene
combination therapy. The most common adverse
events with torasemide were headache, dizziness,
nausea, asthenia and muscle cramps. The pattern
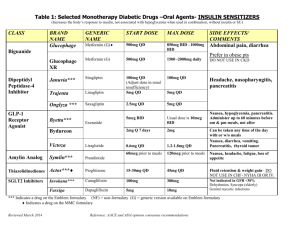
Table III. Comparison of antihypertensive effects of torasemide (TS) with indapamide (IND), hydrochlorothiazide (HCT), chlorthalidone
(CHL) and the fixed combinations of hydrochlorothiazide with triamterene (HCT/T) or amiloride (HCT/A) in a double-blind randomised
group comparison design
Study drug and dose
No. of
Duration
Initial BP/DBP
Decrease in SBP/
Decrease in SBP/
(mg)
patients
(weeks)
(mm Hg)
DBP (mm Hg)
before dose
doubling (weeks)
DBP at end-point
(mm Hg)
12
166/107
-17/ -1 5(4)
-25/-22
Spannbrucker et
164/106
-16/-15 (4)
-2 8 / - 2 2
al. (1988)
175/105
177/103
-27/-21
Reyes et al.
(1990a)
157/106
162/106
-13/-14
TS 2.5-5
32
IND 2.5-5
34
TS 2.5
HCT 25
13
11
19
TS 2.5
CHL 25
9
9
8
Placebo
9
29
TS 2.5-5
HCT/T 25/50-50/100
29
TS 2.5
HCT/T 25/50
43
41
TS 2.5-5
72
HCT/A 50/5-100/0
71
24
-42*/-23
-15/-15
Reference
Porcellati et al.
(1990)
-2/-1
162/103
165/101
-18/-14 (12)
-17/-14
Achhammer &
168/102
-19/-15 (12)
-23/-17
Eberhard (1990)
-17/-13
-21/-14
Boelke et al.
(1990a)
12
167/100
171/102
24
168/103
-17/-13 (10)
-25/-17
Boelke et al.
170/103
-25*/ -16*(10)
-31/-19
(1990b)
Data show a decrease in mean sitting diastolic blood pressure (DBF) and systolic blood pressure (SBP), except in Reyes et al. (1990)
where supine blood pressure was reported, and in Boelke et al. (1990a) where median values were reported. * = p < 0.05 group
comparison.
Fig. 2. Influence of once-daily application of torasemide 2.5
or 5mg (—) and the fixed combination of hydrochlorothiazide/triamterene 25/50 to 50/100mg (---) on serum potassium (a) and magnesium (b) during 24 weeks (adapted from
Achhammer & Eberhard 1990). Data were measured at the
lime points shown on the x axis.
was similar with thiazides: most often dizziness,
followed by muscle cramps, asthenia, headache and
nausea.
The low incidence of adverse events with torasemide, especially hypokalaemia, can be regarded as a consequence of the low dose used in
these studies. Hypokalaemia and increased blood
glucose occur with indapamide, hydrochlorothiazide and chlorthalidone as monotherapy, and with
the fixed combination of hydrochlorothiazide and
amiloride.
6. Long term Efficacy and Safety
In addition to the comparative studies described above which lasted up to 24 weeks, a dosecontrolled double-blind study was carried out in
newly diagnosed patients with hypertension (DBP
between 100 and 115mm Hg) comparing torasem-
ide 2.5 and 5mg once daily over 48 weeks (Baumgart et al. 1990). 98 patients qualified for statistical
evaluation after 48 weeks according to a protocol
which allowed only 1 dose doubling after 4 weeks
in case of insufficient response, too early for the
full antihypertensive effect of 2.5 or 5mg according
to the available results of other studies cited. However, torasemide 2.5 to 5mg administered once daily
exerted, an antihypertensive effect similar to 5 to
l0mg over time; the steady-state effect was reached
after 12 weeks.
Before dose doubling at week 4, the effect of
5mg was somewhat more pronounced than that of
2.5mg, which is also reflected in the percentage of
patients in which the dose was doubled (38% in the
2.5mg group and 19% in the 5mg group). However,
in patients continuing on the initial doses the blood
pressure reduction was similar for both doses (fig.
3).
Torasemide was well tolerated. One patient
withdrew with allergic exanthema, and transient
adverse events were reported in 10% of the patients
(hypokalaemia and gastrointestinal complaints each
2%; exanthema, headache and dizziness each 1.4%:
pruritus, paraesthesia and chest pain each in 1
patient). The trend in laboratory values of serum
concentrations of potassium, magnesium and uric
acid, and blood glucose is given in figure 4a, and
that of triglycerides, cholesterol, low density lipoprotein (LDL)-cholesterol and high density lipoprotein (HDL)-cholesterol in figure 4b for torasemide 2.5 and 5mg given over 48 weeks. The initial
small change in potassium in the range of —0.15
mmol/L was only seen within the first 4 weeks of
application. No significant changes were seen in
magnesium, glucose, triglycerides, and total as well
as HDL- and LDL-cholesterol. Uric acid increased
slightly but significantly during the first 6 months
and tended to decrease to normal values thereafter.
7, Conclusion
Diuretics have been a cornerstone of modern
antihypertensive treatment over the past 3 decades. Their use has been challenged because they
may produce metabolic disturbances such as glu-
88
cose intolerance, increases in serum cholesterol and
triglycerides as well as decreases in serum potassium and magnesium. Large intervention trials with
diuretics or -blockers have generally demonstrated a significant reduction in stroke, but failed
to provide a significant reduction in myocardial infarction. There has been speculation that the metabolic sequelae as well as arrhythmias caused by potassium depletion associated with diuretic use partly
offset the cardiovascular benefit of this class of
drugs. In a recent meta-analysis of 14 randomised
trials with predominantly diuretic-based therapy
involving 37 000 patients and a mean duration of
treatment of 5 years, the incidence of myocardial
infarction was reduced by 14%, less than that expected from epidemiological data (Collins et al.
1990). In contrast, there is no evidence of an effect
of newer agents such as ACE inhibitors and calcium channel blockers on stroke or heart attacks.
This may change in the future as the US Trial on
Diet and Drug Treatment of Mild Hypertension
(TOMHS) study and the Captopril Prevention
Drugs 41 (Suppl. 3) 1991
Project address this question (Captopril Prevention Project 1990; Stamler 1987). Recent studies
have shown that using the lowest effective dose of
a diuretic avoids significant changes in metabolic
parameters, which usually occur only at the high
doses often used in the large scale intervention
studies (Carlson et al. 1990; McVeigh et al. 1988)
or recommended and used as standard dosage regimens today. Traditionally, furosemide used in the
available standard diuretic dose of 40mg has not
been widely accepted as an effective antihypertensive treatment. Based on an overview of published
comparative trials, McMahon (1990) concluded
that thiazides are more effective than furosemide
in reducing blood pressure in the treatment of
hypertension. Furosemide has been advocated as
an addition to other standard antihypertensives in
hypertensive crisis or in hypertensive patients with
renal impairment. However, when assessing the
metabolic effects of furosemide in hypertensive
patients a trend for less potassium loss and influence on glucose metabolism compared with thia12
Fig. 3. Decrease in diastolic blood pressure (DBP) in patients with essential hypertension responding to the initially applied
dose of either torasemide 2.5 (—) or 5mg (---) [Baumgart et al. 1990]. Data were measured at the time points shown on
the x axis.
Torasemide in Essential Hypertension
Fig, 4. Influence of torasemide 2.5mg (—) or 5mg (---) once daily on serum parameters and blood glucose during 48 weeks'
treatment in patients with essential hypertension (adapted from Baumgart et al. 1990). LDL = low density lipoprotein;
HDL = high density lipoprotein. Data were measured as the time points shown on the x axis.
zides has been described (Bloomgarden et al. 1984;
McMahon 1990; Mroczek et al. 1978).
Recently published data show that newly developed loop diuretics, used in lower than regular
doses in patients with oedema (e.g. muzolimine 15
to 20mg or torasemide 2.5 to 5mg), lower blood
pressure to a similar extent compared with thiazides and other drug classes used in hypertension
(Cocchieri et al. 1985; Kirsten et al. 1985; Lucsko
etal. 1985; Pirelli & Stella 1983). As shown for low
doses of torasemide, the influence on metabolic and
electrolyte parameters is minimal or absent. Low
doses of those loop diuretics are generally well tolerated without causing polyuria or the striking and
intensive fluid excretion over the first hours after
application. A low dose of torasemide 2.5 to 5mg
does not increase potassium or magnesium excretion in the first hours after application compared
with placebo, even if natriuresis is slightly and significantly increased, which may serve as an explanation for the noneffect of this dose on electrolyte parameters in long term treatment. Further
studies are needed to elucidate the mechanism of
action whereby low doses of cither loop or thiazide
diuretics reduce blood pressure, because the initial
volume contraction reported for usual doses of
thiazides is not to be expected with these smaller
doses. Vasodilatation mediated by small shifts in
intracellular electrolytes and no counter-regulation
via increases in the renin-angiotensin system induced by diuretics may partly explain the antihypertensive effect of low doses of diuretics.
90
Drugs 41 (Suppl. 3) 1991
References
Achhammer I, Eberhard R, Comparison of serum potassium levels during long-term treatment of hypertensive patients with
2.5mg torasemide/day or 50mg triamterene/25mg hydrochlorothiazide/day. In Kruck et al. (Eds) Torasemide: Clinical
Pharmacology and Therapeutic Applications. Progress in
Pharmacology and Clinical Pharmacology, Vol. 8/1, pp. 211220, Gustav Fischer Verlag, Stuttgart, 1990
Amery A, Fagard R, Lijnen P, Staessen J, Van Hoof R. Treatment
of the elderly hypertensive patient. Journal of Hypertension 8
(Suppl. 2): 39-47, 1990
Bakris E, Frohlich ED. Evolution of antihypertensive therapy.
Journal of the American College of Cardiology 14: 1595-1688,
1989
Baumgart P, Walger P, van Eiff M, Achhammer I. Long-term
efficacy and tolerance of torasemide in essential
hypertension In Kruck et al. (Eds) Torasemide: Clinical
Pharmacology and Therapeutic Applications. Progress in
Pharmacology and Clinical Pharmacology, Vol. 8/1, pp. 169182, Gustav Fischer Verlag, Stuttgart, 1990
Beermann B, Groschinski-Grind M. Pharmacokinetics of hydrochlorothiazide in man. European Journal of Clinical Pharmacology 12: 297-303, 1977
Beermann B, Groschinsky-Grind M. Antihypertensive effect of
various doses of hydrochlorothiazide and its relation to the -
plasma level of the drug. European Journal of Clinical
Pharmacology 13: 195-201, 1978
Bloomgarden ZT, Ginsberg-Fellner F, Rayfield EJ, Bookman J,
Brown WV. Elevated hemoglobin A1c and low-density lipoprotein cholesterol levels in thiazide-treated diabetic patients.
American Journal of Medicine 77: 823-827, 1984
Boelke T, Achhammer I, Meyer-Sabellek WA, Streitberg P, Tagesund Nachtrhythmik ambulanter 24 - h Blutdruckwerte von alteren essentiellen Hypertonikern bei Therapie mil verschiedenen Antihypertonika. Hochdruck 10: 40, 1990a
Boelke T, Achhammer I, Meyer-Sabellek WA. Blutdrucksenkung
und metabolische Veranderungen bei essentiellen Hypertonikern nach Lanzeitgabe unterschiedlicher Diuretika. Hochdruck 9: 40-41, 1990b
Brunner HR, Menard J, Waeber B, et al. Treating the individual
hypertensive patient: considerations on dose, sequential
monotherapy and drug combinations. Journal of Hypertension
8: 3-11, 1990
Captopril Prevention Project. A prospective intervention trial of
angiotensin converting enzyme inhibition in the treatment of
hypertension. Journal of Hypertension 8: 985-990, 1990
Carlson JE, Kober L, Torp-Peterson C, Johansen P. Relation between dose of bendrofluazide, antihypertensive effect and adverse biochemical effects. British Medical Journal 300: 975978, 1990
Cocchieri M, Chiuini E, Fortunati F, Fedeli L, Solinas P. Efficacy
of two different doses of muzolimine in the treatment of mild
hypertension. Zeitschrift fur Kardiologie 74 (Suppl. 2): 56-59,
1985
Collins R, Peto R, McMahon S, et al. Blood pressure, stroke and
coronary heart disease. Part 2. Short-term reductions in blood
pressure: overview of randomised drug trials in their epidemiological context. Lancet 335: 827-838, 1990
Dupont AG, Schoors D, Six RO, Vanhaelst L. Antihypertensiveefficacy of low dose torasemide in essential Hypertension: a
placebo-controlled study. Journal of Human Hypertension 2: 265268, 1988
Freis ED. Critique of the clinical importance of diuretic induced
hypokalemia and elevated cholesterol level. Archives of Internal Medicine 149: 2640-2648, 1989
Joint National Committee. The 1988 report of the Joint National
Committee on detection, evaluation and treatment of high blood
pressure. Archives of Internal Medicine 148: 1023-1038, 1988
Kau ST. Diuretics: what we have and what we need. In Reyes
A.J. and Leary W.P (Eds) Clinical Pharmacology and Therapeutic Uses of Diuretics. Progress in Pharmacology and Clinical
Pharmacology 6/3, pp. 1-63, Gustav Fischer Verlag, Stuttgart,
1988
Kirsten R, Molz KH, Tzonev I, Nelson K. Clinical evaluation of
muzolimine and indapamide during treatment for essential
hypertension. Zeitschrift fur Kardiologie (Suppl. 2): 66-72, 1985
Komajda M, Klimczak K, Boutin B, et al. Effects of indapamide
on left ventricular mass and function in systemic hypertension
with left ventricular hypertrophy. American Journal of Cardiology 65: 37H-42H, 1990
Lambe R, Kennedy O, Kenny M, Darragh A. Study of the tolerance and diuretic properties of torasemide following oral or
intravenous administration to healthy volunteers. European
Journal of Clinical Pharmacology 31 (Suppl. 1): 9-14, 1986
Leary WP, Reyes AJ. Renal excretory actions of diuretics in man:
corrections of various current errors and redefinition of basic
concepts. In Reyes AJ, Leary WB. (Eds) Clinical Pharmacology
and Therapeutic Uses of Diuretics. Progress in Pharmacology
and Clinical Pharmacology 6/3, pp. 153-166, Gustav Fischer
Verlag, Stuttgart, 1988
Lucsko M, Kerihuel JC, Chaignon M, Aubert PH, Guedon J.
Comparative study of muzolimine and acebutolol in the treatment of moderate hypertension. Zeitschrift fur Kardiologie
(Suppl. 2): 73-76, 1985
Mace PJE, Littler WA, Glover DR, et al. Regression of left ventricular hypertrophy in hypertension: comparative effects of
three different drugs. Journal of Cardiovascular
Pharmacology 7 (Suppl. 2): 52-55, 1985
Materson B, Oster J, Michael UF, Bolton SM, Burton ZC, et al.
Dose response to chlorthalidone in patients with mild hypertension efficacy of a lower dose. Clinical Pharmacology and
Therapeutics 24: 192-198, 1978
McMahon FG. Management of essential hypertension. The oncea-day era. pp. 297-378. Futura Publishing Company Inc., Mount
Kisco, New York, 1990.
McMahon S, Petro R, Cutler J. et al. Blood pressure, stroke and
coronary heart disease. Part I. Prolonged differences in blood
pressure: prospective observational studies corrected for the
regression dilution bias. Lancet 335: 765-774, 1990
McVeigh G, Galloway D, Johnston D. The case for low dose
diuretics in hypertension: comparison of low and conventional
doses of cyclopenthiazide. British Medical Journal 297: 95-98,
1988
Medical Research Council Working Party. MRC trial of treatment of mild hypertension: principal results. British Medical
Journal 291: 97-104, 1985
Morgan TO. Metabolic effects of various antihypertensive agents.
Journal of Cardiovascular Pharmacology 15 (Suppl. 5): 39-45,
1990
Mroczek WJ, Martin CH, Hattwick MAW, Kennedy M. Once
daily furosemide therapy in diuretic-treated hypertensive
patients. Current Therapeutic Research 24: 824-830, 1978
Mueller G, Haecker W. Torasemide a new loop diuretic in
the treatment of essential hypertension without renal
impairment. Abstract no. l3. Cardiovascular Pharmacotherapy
International Symposium, Geneva, 1985
Pagano G, Dal Molin V, Bozzo C, Carta Q. Interference on metabolism induced by muzolimine and chlorthalidone in type
II hypertensive diabetics. Zeitschrift fur Kardiologie 74 (Suppl.
2): 80-83, 1985
Pirelli A, Stella M. Comparison of the antihypertensive effects of
methyldopa and muzolimine in arterial hypertension. In Andreucci VE (Ed.) Recent advances in diuretic therapy, pp. 127135, Exerpta Medica, Amsterdam, 1983
Porcellati C, Verdecctria P, Schillaci G, et al. La torasemide, nuovo
diuretico dell'ansa, nel trattamento dell'ipertensione arteriosa.
Torasemide in Essential Hypertension
Studio controllata in doppia cecita. Basi-Razion Terapia 20:
407-410, 1990
Reyes AJ, Leary WP, van der Byl K, Manaraj B. Renal_excretory
pharmacodynamics of diuretics in man: comparison between
furosemide. hydrochlorothiazide and torasemide. In Reyes AJ &
Leary WP (Eds) Clinical Pharmacology and Therapeutic Uses of
Diuretics. Progress in Pharmacology and Clinical Pharmacology 6/3, pp. 83-151, Gustav Fischer Verlag, Stuttgart, 1988
Reyes AJ, Chiesa PD, Santucci MR. Batista LB, Olhaberry JV,
et al. Hydrochlorothiazide versus a non-diuretic dose. of torasemide as once-daily antihypertensive monopharmacotherapy in elderly patients. A randomized and double-blind study.
In Kruck et al. (Eds) Torasemide: Clinical Pharmacology and
Therapeutic Applications. Progress in Pharmacology and
Clinical Pharmacology, Vol. 8/1, pp. 183-210, Gustav Fischer
Verlag, Stuttgart, 1990a
Reyes AJ, Leary WP, van der Byl K. Excretions of urinary fluid
and solutes after single doses of furosemide and
hydrochloro-thiazide-and of four different single doses of the
diuretic to-rasemide in healthy subjects. In Kruck el al. (Eds)
Torasemide: Clinical Pharmacology and Therapeutic
Applications. Progress in Pharmacology and Clinical
Pharmacology, Vol.8/1, pp 4772, Gustay Fischer Verlag,
Struttgart. 1990b
Romano C, Copercini B, Ghiringhelli P. Gnocchi E, Pecchini E.
Etozoline induced urine excretion of water and solutes in
patients with hypertension. In Andreucci VE & Dal Canton A
(Eds) Diuretics: basic, pharmacological and clinical aspects, pp.
289-291, Martinus Nijhoff Publishing, Boston, 1987
Russo D, Cofelice G, Conte G. Giunta A, Malone S, et al Antihypertensive mechanisms of muzolimine. In Andreucci VE &
Dai Canton A (Eds) Diuretics: basic, pharmacological and
clinical aspects, pp. 268-270, Martinus Nijhoff Publishing,
Boston, 1987
Shigmatsu S, Hiramatsu K, Aizawa T, et al. Regression of left
ventricular hypertrophy in patients with essential hypertension: outcome of 12 years antihypertensive treatment. Cardiology 77: 280-286, 1990
Skarfors ET, Lithell HO, Selernius I, Aberg H. Do antihypertensive drugs precipitate diabetes in predisposed man? British
Medical Journal 298: 1147-1152, 1989
Spannbrucker N, Achhammer I, Metz P. Glocke M.
Comparative study on the antihypertentive efficacy of torasemide
and in-dapamide in patients with esseatial hypertension.
Arzneimit-tel-Forschung 38: 190-193, 1988
Spieker C, Zidek W, Hacker W, Schmidt W, Vetter H. Assessment of intracellular sodium and calcium in essential hypertension during diuretic treatment. Arzneimittel-Forschung 38:
188-190, 1988
Spieker C, Zidek W, Vetter H. Acute effect of torasemide on the
renin activity and on intracellular electrolytes in hypertensive
patients. In Kruck et al. (Eds) Torasemide: Ciinical Pharmacology and Therapeutic Applications. Progress in Pharmacology and Clinical Pharmacology, Vol. 8/1, pp. 221-226. Gustav
Fischer Verlag, Stuttgart, 1990
Stamler J, Prineas RJ, Neaton JD, Grimm RH, McDonald RH,
et al. Background and design of the new US trial on diet and
drug treatment of "mild" hypertension (TOMHS). American
Journal of Cardiology 59: 51G-60G, 1987
Swales JD, Ramsay LE, Coope JR. Pocock SJ. Robertson JIS, et
al. Treating mild hypertension. Agreement from the large trials.
Report of the British Hypertension Society working party.
British Medical Journal 301: 1172-1173, 1990
Swales JD. Fist line treatment in hypertension still -blockers and
diureties British Medical Journal 301; 1172-1173. 1990
Thompson WG. Review. An assault on old friends: Thiazide diuretics under siege. American Journal of Medical Sciences 300152-158, 1990
Zidek W, Losse H, Dorst KG, Zumkley H, Vetter H. Intracellular sodium and calcium in essential hypertension. Klinische
Wochenschrift 60: 839-862. 1982
Zidek. W, Losse H, Schmidt, Fckske KJ, Vetter H. Intracellular
electrolytes during antihypertensive treatment with a loop diuretic. Journal of Hypertension 2: 393-395, 1984
Correspondence and reprints: Dr P. Metz, Project Development,
Boehringer Mannheim GmbH, Sandhoferstrasse 116, D-6800
Mannheim 31, Federal Republic of Germany.