Dynamic information improves discharge prediction after cardiac
advertisement
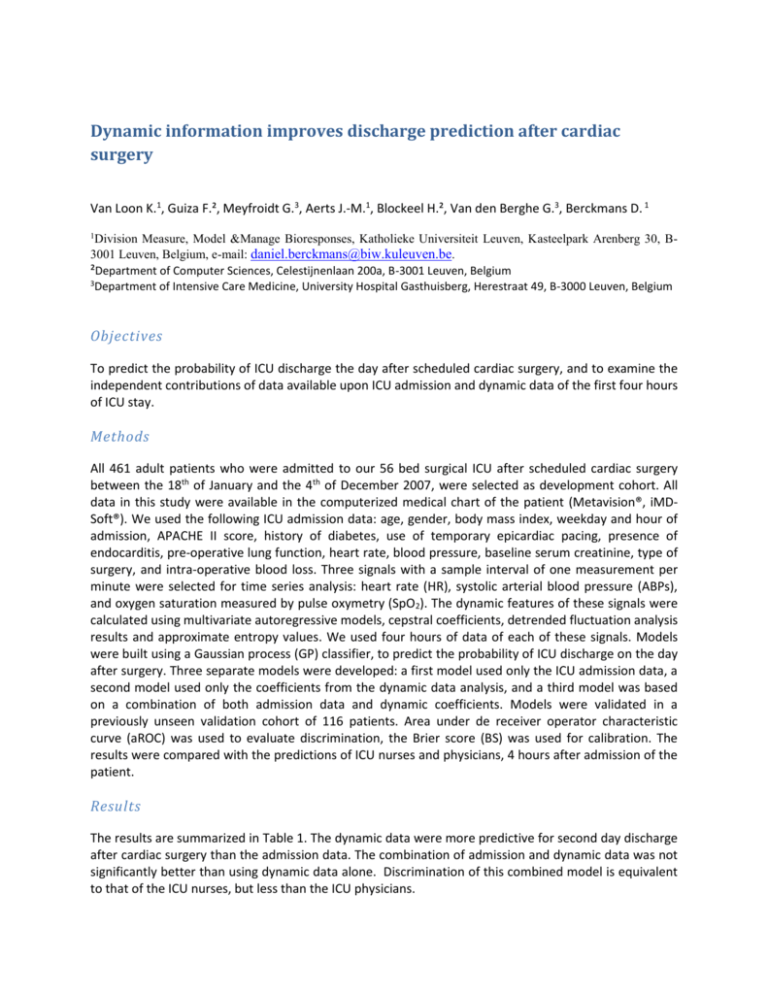
Dynamic information improves discharge prediction after cardiac surgery Van Loon K.1, Guiza F.², Meyfroidt G.3, Aerts J.-M.1, Blockeel H.², Van den Berghe G.3, Berckmans D. 1 1 Division Measure, Model &Manage Bioresponses, Katholieke Universiteit Leuven, Kasteelpark Arenberg 30, B3001 Leuven, Belgium, e-mail: daniel.berckmans@biw.kuleuven.be. ²Department of Computer Sciences, Celestijnenlaan 200a, B-3001 Leuven, Belgium 3 Department of Intensive Care Medicine, University Hospital Gasthuisberg, Herestraat 49, B-3000 Leuven, Belgium Objectives To predict the probability of ICU discharge the day after scheduled cardiac surgery, and to examine the independent contributions of data available upon ICU admission and dynamic data of the first four hours of ICU stay. Methods All 461 adult patients who were admitted to our 56 bed surgical ICU after scheduled cardiac surgery between the 18th of January and the 4th of December 2007, were selected as development cohort. All data in this study were available in the computerized medical chart of the patient (Metavision®, iMDSoft®). We used the following ICU admission data: age, gender, body mass index, weekday and hour of admission, APACHE II score, history of diabetes, use of temporary epicardiac pacing, presence of endocarditis, pre-operative lung function, heart rate, blood pressure, baseline serum creatinine, type of surgery, and intra-operative blood loss. Three signals with a sample interval of one measurement per minute were selected for time series analysis: heart rate (HR), systolic arterial blood pressure (ABPs), and oxygen saturation measured by pulse oxymetry (SpO2). The dynamic features of these signals were calculated using multivariate autoregressive models, cepstral coefficients, detrended fluctuation analysis results and approximate entropy values. We used four hours of data of each of these signals. Models were built using a Gaussian process (GP) classifier, to predict the probability of ICU discharge on the day after surgery. Three separate models were developed: a first model used only the ICU admission data, a second model used only the coefficients from the dynamic data analysis, and a third model was based on a combination of both admission data and dynamic coefficients. Models were validated in a previously unseen validation cohort of 116 patients. Area under de receiver operator characteristic curve (aROC) was used to evaluate discrimination, the Brier score (BS) was used for calibration. The results were compared with the predictions of ICU nurses and physicians, 4 hours after admission of the patient. Results The results are summarized in Table 1. The dynamic data were more predictive for second day discharge after cardiac surgery than the admission data. The combination of admission and dynamic data was not significantly better than using dynamic data alone. Discrimination of this combined model is equivalent to that of the ICU nurses, but less than the ICU physicians. Table 1: The aROC values and Brier scores of the different experiments Input Admission Dynamic Coefficients Combined Model Nurses Doctors aROC 0.650 0.721 0.720 0.724 0.788 BS 0.226 0.182 0.187 0.241 0.212 Conclusion Dynamic information of only three physiological variables (heart rate, systolic arterial blood pressure and oxygen saturation) measured during the first few hours of ICU stay is more predictive for ICU discharge than static admission data. The dynamic models are as performant as ICU nurses, but less than ICU physicians.