Liver and Gall Bladder
LIVER AND GALLBLADDER
The liver is a soft, red organ that’s the largest internal organ in the body. Only the skin outsize’s the liver; however it is an external organ. The liver lies anatomically inferior to the thoracic cavity and diaphragm, and it occupies most of the abdominopelvic cavity.
The gall bladder is a short (3-4 inches), pear-shaped sac, which stores and concentrates bile, a digestive fluid.
The gallbladder is usually hanging inferior to the anterior inferior margin of the liver.
Anatomy
The liver mostly under the thoracic cage and is covered by a more superficial visceral peritoneum and a shell of dense irregular connective tissue that’s deeper. The liver can be divided into two wedge-shaped lobes that are separated by the falciform ligament. The falciform ligament is a flap that runs from the parietal peritoneum of the diaphragm to the visceral peritoneum of the liver; this ligament also helps suspend the liver in the abdominal cavity. The right lobe is considered by many to include an inferior quadrate lobe and a posterior caudate lobe, however, these two more appropriately belong to the left lobe. The liver lies to the right [lateral] of the median plane and may even reach your iliac crest.
The middle or central portion of the gallbladder is called the body of the gallbladder. The pointed portion is referred to as the neck, which along with the body project superiorly. The downward projection of the gallbladder is the fundus, which extends beyond the inferior border of the liver.
Histology
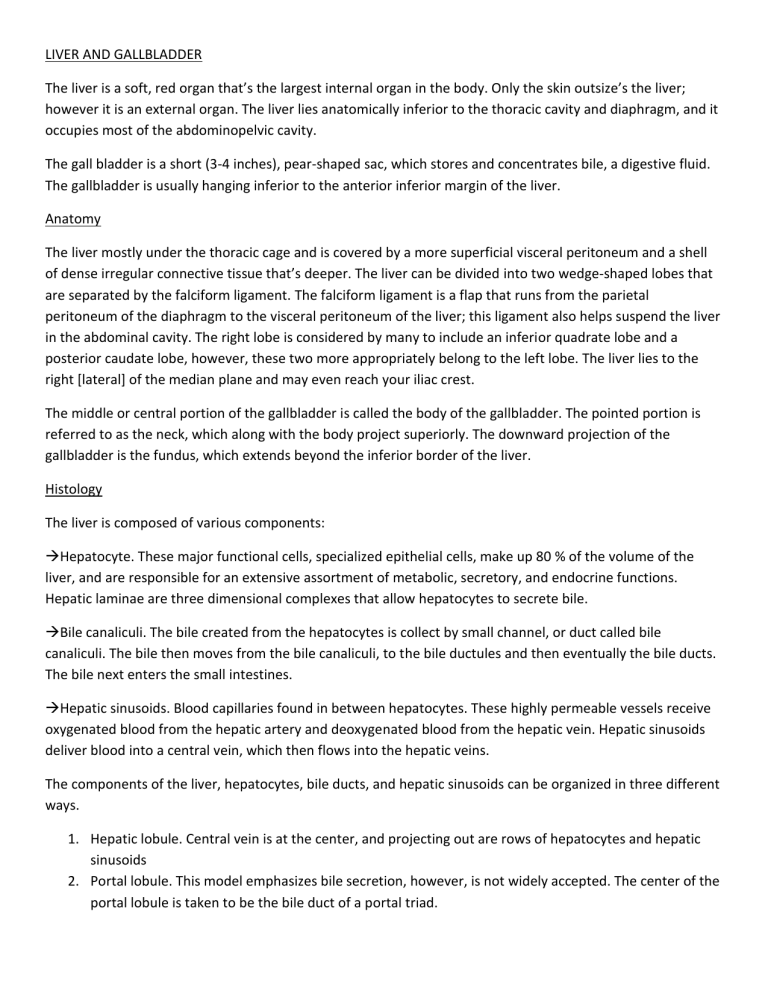
The liver is composed of various components:
Hepatocyte. These major functional cells, specialized epithelial cells, make up 80 % of the volume of the liver, and are responsible for an extensive assortment of metabolic, secretory, and endocrine functions.
Hepatic laminae are three dimensional complexes that allow hepatocytes to secrete bile.
Bile canaliculi. The bile created from the hepatocytes is collect by small channel, or duct called bile canaliculi. The bile then moves from the bile canaliculi, to the bile ductules and then eventually the bile ducts.
The bile next enters the small intestines.
Hepatic sinusoids. Blood capillaries found in between hepatocytes. These highly permeable vessels receive oxygenated blood from the hepatic artery and deoxygenated blood from the hepatic vein. Hepatic sinusoids deliver blood into a central vein, which then flows into the hepatic veins.
The components of the liver, hepatocytes, bile ducts, and hepatic sinusoids can be organized in three different ways.
1.
Hepatic lobule. Central vein is at the center, and projecting out are rows of hepatocytes and hepatic sinusoids
2.
Portal lobule. This model emphasizes bile secretion, however, is not widely accepted. The center of the portal lobule is taken to be the bile duct of a portal triad.
3.
Hepatic acinus. This is the most accepted structural and functional unit of the liver. The cells are divided into three zones. Zone 1 cells are first to receive oxygenated blood. Zone 3 cells are the last to regenerate, and showing effects of toxins. Zone 2 cells have characteristics that intermediate between zone 1 and 3.
The inner surface of the gallbladder, the mucosa, is simple columnar epithelium. The muscular coat of the gallbladder consists of smooth muscle fibers. The outer coat of the gallbladder is the visceral peritoneum.
Blood and Nerve supply
The liver receives blood from two sources. The hepatic artery provides oxygenated blood to liver, and the hepatic vein provides deoxygenated blood to the liver. The nerve that triggers the liver is the 10 th cranial nerve, the vagus nerves.
The gallbladder is also controlled by the vagus nerve, but it also includes branches of the celiac plexus. The cystic artery supplies blood to the gallbladder and its corresponding artery drains the gallbladder.
Functions
The liver’s main function is to secrete bile, which emulsify and absorb digested lipids, however the liver performs much more essential functions:
Carbohydrate metabolism - Maintain a normal blood glucose level
Lipid metabolism - Generate ATP by breaking fatty acids.
Protein metabolism – Hepatocytes deaminate (removing amino group) amino acids so they are used for ATP production.
Processing of drugs and hormones – the liver can detoxify harmful substances.
Excretion of bilirubin- metabolized by small intestines.
Synthesis of bile salts.
Storage - store certain vitamins in liver.
Phagocytosis - engulf aged red blood cells, white blood cells, and some bacteria.
Activation of vitamin D – synthesize active form of vitamin D.
The function of the gallbladder is to store and concentrate bile until they bile is ready for use by the small intestines.